Predictors of Major Depression and Posttraumatic Stress Disorder Following Traumatic Brain Injury: A Systematic Review and Meta-Analysis
Abstract
Materials and Methods
Information Sources
Study Selection
Participants.
Outcome measurement.
Predictors.
Study design.
Data Extraction and Assessment of Risk of Bias
Data Synthesis
Multiple Publications
Results
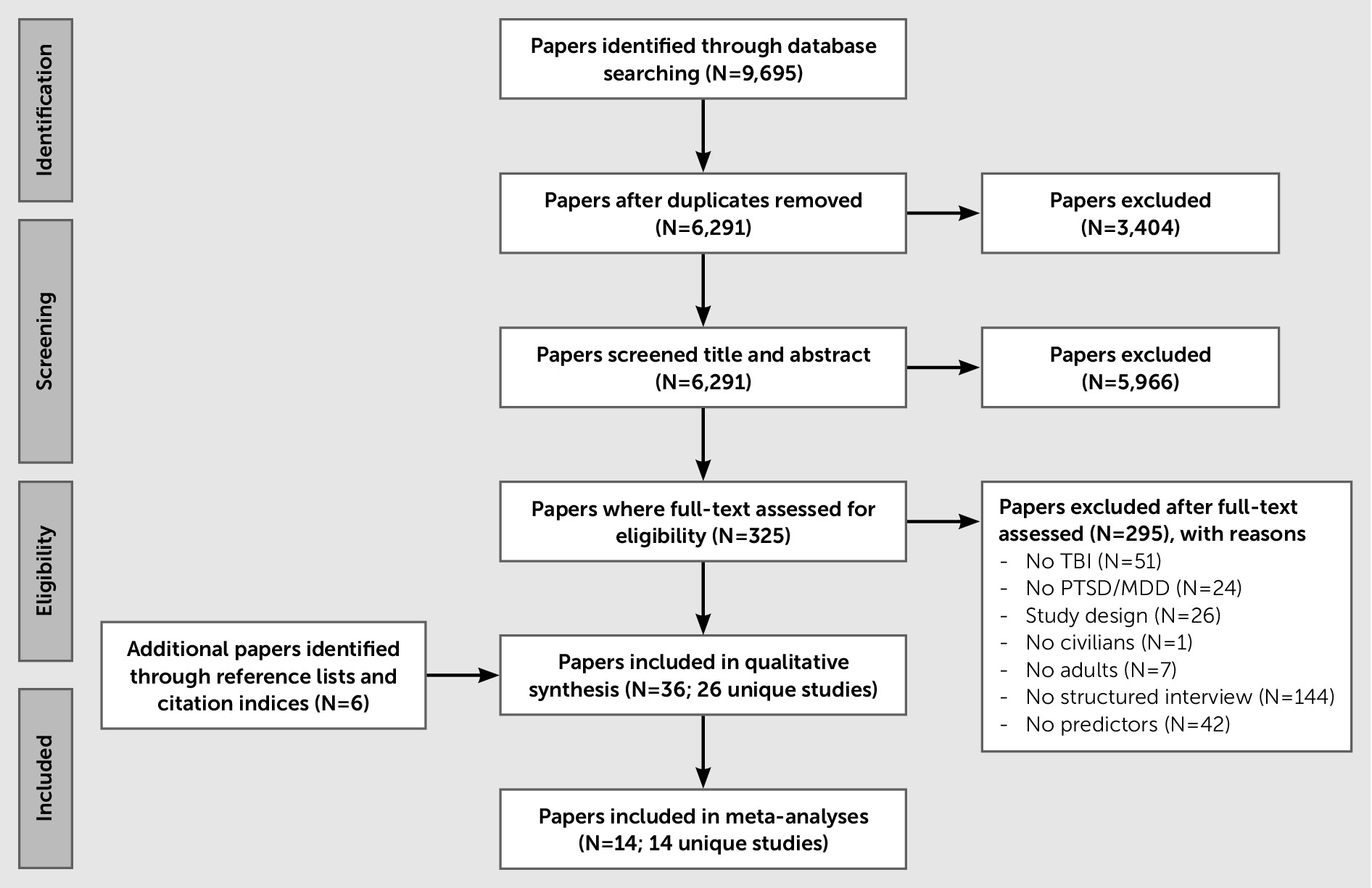
Study Selection
Study Characteristics
| Study | Study Design, Setting | Study Population | Inclusion and Exclusion Criteria | Patient Characteristicsb | No. of Predictors | Disorder and No. of Patients With Disorder | Interview | Timing Outcome | Assessment |
|---|---|---|---|---|---|---|---|---|---|
| Alway et al.37 | Pros cohort, Australia | Consecutive moderate and severe TBI admitted to hospital (N=203) | PTA >24 h; age 16–80 y; no prior TBI/neurological disorder; residence in Australia, sufficient English language | Age: 34 y ±16 y | 5 | PTSD (N=27)c | SCID (DSM-IV) | 3 m to 5 y | Face-to-face interview at initial assessment; telephone interview at follow-up |
| 78% male | |||||||||
| Related: Alway et al.62 | GCS: 9.3±4.3 | ||||||||
| 80% MVA | |||||||||
| Ashman et al.54 | Cross-sectional, longitudinal, and cross-sequential, United States | Self-identified mild to severe TBI from community (N=188) | US residents in the community 3 m to 4 y postinjury; age 18–87; capable of giving informed consent; no acquired brain injury/ neurocognitive disorder/psychotic disorder | Age: 40 y ±15 y | 3 MDD /3 PTSD | MDD (N=66)d and PTSD (N=56)d | SCID (DSM-IV) | 1–6 y | Interview by clinician with ≥3 y experience |
| Related: Hibbard et al.59 | 53% male | ||||||||
| GCS: 13–15, 29%; 3–12, 62%; unknown, 9% | |||||||||
| Barker-Collo et al.48 | Pros and retro cohort, New Zealand | Mild to severe TBI from a large incidence and outcome study or self-referred (N=296) | Age ≥16 | Age: 37 y ±18 y | 17 | PTSD (N=53) | PDS (DSM-IV) | 1 y | Interview by trained researchers |
| 60% male | |||||||||
| Worst GCS: 14.1 ±2.3 | |||||||||
| 30% falls, 24% assault, 17% traffic | |||||||||
| Bryant and Harvey38 | Pros cohort, Australia | Consecutive MVA victims admitted to trauma hospital (N=63) | Exclusion: inability to be interviewed with aid of an interpreter; not medically fit; taking narcotic analgesia 4weeks after trauma; PTA >24 h | Age: 29 y ±13 ye | 25 | PTSD (N=15) | CIDI (DSM-III) | 6 m | Interview by clinical psychologist blinded for ASD status |
| Related: Harvey and Bryant58 | 70% malee | ||||||||
| Bryant et al.39 | Pros cohort, Australia | Severe TBI admitted to rehabilitation unit (N=96) | Exclusion: inability to be interviewed with aid of an interpreter; insufficient cognitive abilities | Age: 34 y ±13 y | 5 | PTSD (N=26) | PTSD-I (DSM-III) | 6 m | Interview by rehabilitation consultant |
| 80% male | |||||||||
| Caspi et al.50 | Retro cohort, Israel | Mild to moderate TBI admitted to neurocognitive clinic (N=120) | Age: 18–50 y, fluent in Hebrew; no active chronic medical condition; no preinjury psychiatric illness, substance abuse, cognitive deficits, or brain damage | Age: 36 y ±6 y | 4 | PTSD (N=22) | SCID-I (DSM-IV) | 3 y | Interview |
| 59% male | |||||||||
| 84% car accident | |||||||||
| Deb and Burns40 | Pros cohort, United Kingdom | Minor to severe TBI admitted to hospital (N=165) | Any of the following: unconsciousness; evidence of skull fracture on x-rays; contusion/hemorrhage on CT or MRI; focal neurological signs; GCS <15 | Age: young group: 36; elderly group: 79 | 1 | MDD (N=24) | SCAN (ICD–10) | 1 y | Interview by two trained psychiatrists |
| 67% male | |||||||||
| 82% mild, 13% moderate, 5% severe TBI | |||||||||
| Diaz et al.41 | Pros cohort, Brazil | Consecutive severe TBI admitted to ICU (N=33) | GCS ≤8 within 48 h; age ≥18 y; resident of the Florianopolis metropolitan area; no gunshot injury | Age: 31 y ±11 y | 7 | MDD (N=10) | SCID (DSM-IV) | 18 m | Interview by two board-certified psychiatrists, blinded for hospital data |
| 88% male | |||||||||
| GCS: 7–8, 46%; 5–6, 30%; 3–4, 24% | |||||||||
| Fedoroff et al.36 | Pros cohort, United States | Consecutive mild to severe TBI admitted to shock trauma center (N=64) | Acute closed HI, no open HI, no spinal cord injury, no multiple system injury, no decreased consciousness or aphasia | Age: MDD 27 y ±6 y; no MDD: 30 y ±11 y | 25 | MDD (N=17) | PSE (DSM-III) | 1 m | Interview by trained research psychiatrist |
| Related: Jorge et al.79, Jorge et al.80b | 86% male | ||||||||
| GCS: 12–15, 17%; 8–15 & intracranial surgery or focal lesions >35 cc, 58%; 3–7, 15% | |||||||||
| Gil et al.35 | Pros cohort, Israel | Mild TBI admitted to surgical ward (N=120) | Age 18–50 y; fluent in Hebrew | Age: 31 y ±3 y | 16 | PTSD (N=17) | SCID (DSM-IV) | 6 m | Interview by trained clinician |
| 58% male | |||||||||
| Exclusion: psychiatric care at time of injury; prior HI; cognitive deficits; substance abuse; major untreated medical condition | 90% traffic accident | ||||||||
| GCS: 13–15 100% | |||||||||
| Gould et al.42 | Pros cohort, Australia | Consecutive TBI admissions to a rehabilitation hospital (N=122) | Mild, moderate, or severe TBI; age 16–80; no previous TBI/ neurological disorder; residence in Australia; sufficient cognitive and English ability | Age: 35; 16 y | 7 | MDD (N=40) | SCID (DSM-IV) | 12 m | Interview |
| Related: Gould et al.60 and Schonberger et al.81 | GCS: 9.15 ±4.3 | ||||||||
| Hibbard et al.43 | Pros cohort, United States | Mild to severe TBI randomly selected for quality of life survey (N=100) | TBI ≤1 y prior to interview; age 18–65; resident of New York state; living in the community; no nontraumatic brain injury | Agef:40 y ±10 y | 5 MDD /1 PTSD | MDD (N=48) and PTSD (N=17) | SCID (DSM-IV) | 8 y | Interview by licensed psychologist with background in clinical neuropsychology and brain injury |
| 53% male | |||||||||
| 62% MVA | |||||||||
| Jorge et al.57 | Pros case-control, United States | Consecutive mild to severe TBI admitted to hospital (N=91) | Exclude: penetrating HI; spinal cord injury; severe comprehension deficits | Age: 36 y ±16 y | 32 | MDD (N=30) | PSE and SCID-I (DSM-IV) | 9 m | Interview by psychiatrist |
| 59% male | |||||||||
| Related: Jorge et al.61 | 44% mild, 33% moderate, 23% severe TBI | ||||||||
| 75% MVA | |||||||||
| Kennedy et al.19 | Pros cohort, United States | Mild to mod TBI admitted to neuropsychiatric clinic (N=78) | 3 m postinjury; age≥ 18 | Age: 38 y ±12 y | 10 | MDD (N=23) | SCID (DSM-IV) | 76 m | Interview by three trained research team members |
| 69% male | |||||||||
| Mean GCS: 9.3 ±4.8 | |||||||||
| 77% MVA | |||||||||
| Koponen et al.51 | Retro cohort, Finland | Mild to severe TBI seen for neuropsychological evaluation (N=60) | TBI causing neurological symptoms ≥1 week; one of the following: 1) LOC ≥1 min; 2) PTA ≥30 min; 3) neurological symptoms during the first 3 d; 4) neuroradiological findings suggesting TBI. No nontraumatic neurological illness | Age: 29 y ±11 y | 2 | MDD (N=16) | SCAN (DSM-III) | 31 y | Interview by trained research psychiatrist |
| Related: Koponen et al.82 | 68% male | ||||||||
| Levin et al.44 | Pros cohort, United States | Consecutive mild TBI admitted to level I trauma hospital (N=129) | Hospital arrival ≤24 h; BAL ≤200 mg/dl; age ≥16 y; fluent in English or Spanish; resident in catchment area | Age: 32±13 y | 8 | MDD (N=15) | SCID (DSM-IV) | 3 m | Interview |
| 67% male | |||||||||
| Exclusion: undocumented alien; incarcerated; homeless; active military service; spinal cord injury; previous TBI requiring hospitalization; preinjury substance dependence, mental retardation, psychiatric disorders or other central nervous system disturbances; no preexisting condition preventing outcome measurement | GCS: 14.8±0.5 | ||||||||
| 67% MVA | |||||||||
| Li et al.49 | Pros cohort, China | Consecutive mild TBI patients at the ED of three hospitals (N=43) | LOC <20 min, PTA <24 h, GCS 13–15, no abnormal CT/MRI findings | Age: PTSD 35.8 y ±7.6; no PTSD 36.7 y ±7.1 | 9 | PTSD (N=21)— | CAPS | 6 m | Interview |
| 49% male | |||||||||
| Mauri et al.5 | Pros case-control, Italy | Consecutive closed HI admitted to neurosurgery (N=16) | LOC ≥1m; PTA ≥30 min; neuroradiological evidence of TBI; no preinjury neurological/cardiorespiratory/psychiatric conditions; no substance abuse | Age: 40 y ±14 y | 4 | MDD (N=10) | SCID (DSM-IV) | 1 m | Interview by expert clinician |
| 63% male | |||||||||
| GCS 10.6±4.4 | |||||||||
| 81% MVA | |||||||||
| O’Donnell et al.26 | Pros cohort, Australia | Randomly selected mild TBI patients at four level I trauma centers (N=404) | Age 18–70 y; English proficiency, hospitalized≥24 h, LOC ≤30 min, GCS 13–15, PTA ≤24 h, not currently psychotic or suicidal | Age: 37.9 y ±14 y | 2 MDD /2 PTSD | MDD (N=65) and PTSD (N=32) | MINI (MDD, DSM-IV); CAPS (PTSD, DSM-IV) | 12 m | Telephone interview |
| 72% male | |||||||||
| 62% transport accidents, 17% falls | |||||||||
| Rao et al.55 | Cross-sectional, United States | Closed HI recruited by advertisements in local newspapers (N=17) | Age ≥18 y; TBI 3–60 m prior to evaluation; no history of diagnosable mood disorder; MMSE >18, stable medical history; sufficient cognitive capacity | Age: MDD, 53; no MDD, 27 | 38 | MDD (N=10) | SCID (DSM-IV) | 3–60 m | Interview |
| Rapoport et al.17 | Pros cohort, Canada | Consecutive mild TBI with appointment at TBI clinic (N=210) | Nonpenetrating mild TBI | Age: 47 y ±20 y | 10 | MDD (N=35) | SCID (DSM-IV) | 49 d | Interview by psychiatrist |
| Related: Rapoport et al.45 | Exclusion: preinjury focal brain disease; serious acute medical illness; schizophrenia; bipolar disorder; dementia | 60% male | |||||||
| 61% MVA | |||||||||
| Rapoport et al.56 | Cross-sectional, Canada | Mild and mod TBI attending a TBI clinic (N=74) | Exclusion: premorbid focal brain disease; serious medical illness; schizophrenia; bipolar disorder; dementia | Age: 35y; ±13y | 16 | MDD (N=21) | SCID (DSM-IV) | 200 d | Interview |
| van Reekum et al.46 | Pros cohort, Canada | Mild to severe TBI admitted to TBI rehabilitation program. Patients were contacted with a female:male ratio of 3:1 (N=18) | TBI due to MVA ≥2 y prior to the study; age <50 y; sufficient language, motor, and perceptual skills to permit testing; no preinjury psychiatric disorder; living in the community | Age: 31 y ±9 y | 4 | MDD (N=9) | SADS-L (DSM-III) | 5 y | Interview by experienced registered psychiatric nurse |
| 44% male | |||||||||
| GCS: 13–15, 28%; 9–12, 17%; 3–8, 56% | |||||||||
| Roitman et al.47 | Pros cohort, Israel | Consecutive mild TBI attended ED (N=402) | MVA survivors | Age: 37 y ±13 y | 1 | PTSD (N=127) | PSS (DSM-IV) | 8 m | Telephone interview |
| Exclusion: arrived to the hospital in coma; LOC >30 min; admitted to the hospital >7 days | 52% male | ||||||||
| Turnbull et al.53 | Retro cohort, Scotland | Mild to severe TBI attended ED who respond to a postal questionnaire (N=53) | Age: 16–65; evidence of TBI; no chronic alcohol abuse | Age: 35 y ±11 y | 1 | PTSD (N=11) | CAPS (DSM-IV) | 6 m | Telephone interview by postgraduate psychologist |
| 87% male | |||||||||
| 32% traffic; 60% assault | |||||||||
| Whelan-Goodinson et al.52 | Retro cross-sectional, Australia | Mild to severe TBI admitted to rehabilitation unit (N=100) | GCS <15; cognitive capable; reliable historians according to treating doctor/neuropsychologist, sufficiently proficient in English; no previous TBI/neurological disorder | Age: 37 y ±14 y | 13 | MDD (N=46) | SCID (DSM-IV) | 0.5–5.5 y | Face-to-face or telephone interview |
| 71% male | |||||||||
| GCS: 9.1; 4.1 | |||||||||
| 86% MVA |
Risk of Bias of the Studies
| Study | Study Participation | Study Attrition | Prognostic Factor Measurement | Outcome Measurement | Study Confounding | Statistical Analyses and Presentation |
|---|---|---|---|---|---|---|
| Alway et al.37 | Moderate | Moderate | Low | Low | Low | Low |
| Ashman et al.54 | Moderate | Moderate | Moderate | Low | Low | Moderate |
| Barker-Collo et al.48 | Moderate | Moderate | Low | Low | High | Low |
| Bryant and Harvey38 | Low | Low | Low | Low | High | Low |
| Bryant et al.39 | Low | Moderate | Low | Low | High | Low |
| Caspi et al.50 | Low | Moderate | Low | Low | Low | High |
| Deb and Burns40 | Low | High | Low | Moderate | High | Low |
| Diaz et al.41 | Low | Low | Low | Low | High | Low |
| Federoff et al.83 | Low | Low | Low | Low | High | Low |
| Gil et al.35 | Low | Moderate | Low | Low | Low | Low |
| Gould et al.42 | Low | Moderate | Low | Low | Low | High |
| Hibbard et al.43 | High | Moderate | Moderate | Low | High | Moderate |
| Jorge et al.57 | Low | Low | Low | Low | High | Low |
| Kennedy et al.19 | High | Moderate | Low | Low | High | Low |
| Koponen et al.51 | Moderate | Moderate | Moderate | Low | High | Low |
| Levin et al.44 | Low | Moderate | Low | Low | Low | Low |
| Li et al.49 | Moderate | Low | Moderate | Low | High | High |
| Mauri et al.5 | Moderate | Low | High | Low | High | High |
| O’Donnell et al.26 | Low | Low | Low | Low | High | Low |
| Rao et al.55 | High | Low | Low | Low | High | Moderate |
| Rapoport et al.45 | Moderate | Low | Moderate | Low | Low | Low |
| Rapoport et al.56 | Moderate | Low | Moderate | Low | High | Low |
| van Reekum et al.46 | Moderate | High | Low | Low | High | Low |
| Roitman et al.47 | Moderate | Low | Moderate | Low | High | High |
| Turnbull et al.53 | Moderate | High | Moderate | High | High | High |
| Whelan-Goodinson et al.52 | Moderate | Low | Low | Low | Moderate | Moderate |
Meta-Analyses of Univariable Predictors
| Predictor | No. of Participants (No. of Studies) | Pooled Effect Size Meta-Analysis Odds Ratio (95% CI)b | Heterogeneity (I2) |
|---|---|---|---|
| MDD | |||
| Age (years; MD [95% CI]) | 611 (7) | 1.20 (–1.96 to 4.36) | 49% |
| Female gender | 768 (8) | 1.72 (1.19 to 2.48) | 10% |
| Education (years; MD [95% CI]) | 271 (4) | –0.50 (–1.37 to 0.37) | 43% |
| Caucasian race | 341 (3) | 1.04 (0.61 to 1.75) | 0% |
| Marital statusc | 610 (6) | 1.20 (0.82 to 1.75) | 0% |
| Socioeconomic statusd | 140 (2) | 0.69 (0.33 to 1.43) | 0% |
| Preinjury depression | 470 (5) | 3.86 (2.26 to 6.59) | 0% |
| Preinjury psychiatric disorders | 426 (4) | 1.58 (0.42 to 5.99) | 87% |
| Preinjury alcohol abuse | 244 (2) | 1.49 (0.61 to 3.69) | 0% |
| Preinjury substance abuse | 244 (2) | 2.02 (0.75 to 5.42) | 0% |
| Preinjury unemployment | 244 (2) | 3.80 (0.34 to 42.09) | 77% |
| Family history of psychiatric disorders | 234 (2) | 1.06 (0.52 to 2.14) | 0% |
| Admission GCS (MD [95% CI]) | 151 (2) | 0.49 (0.02 to 0.97) | 0% |
| 24-hour GCS (MD [95% CI]) | 138 (2) | 0.13 (–1.29 to 1.56) | 42% |
| CT abnormalities | 259 (3) | 0.70 (0.35 to 1.43) | 0% |
| Brain contusion | 101 (2) | 1.78 (0.73 to 4.34) | 0% |
| Postinjury unemployment | 211 (3) | 2.04 (1.10 to 3.79) | 9% |
| Postinjury litigation situation | 203 (2) | 0.64 (0.16 to 2.53) | 0% |
| PTSD | |||
| Age (years; MD [95% CI]) | 717 (5) | 1.02 (–1.46 to 3.49) | 75% |
| Female gender | 621 (4) | 1.27 (0.83 to 1.96) | 0% |
| Education (years; MD [95% CI]) | 301 (3) | 0.15 (–0.61 to 0.92) | 11% |
| Preinjury psychiatric disorder | 425 (4) | 1.32 (0.63 to 2.77) | 49% |
| PTA (MD [95% CI]) | 477 (3) | –8.07 (–15.46 to –0.69) | 33% |
| Memory of the traumatic event | 240 (2) | 5.15 (2.37 to 11.21) | 0% |
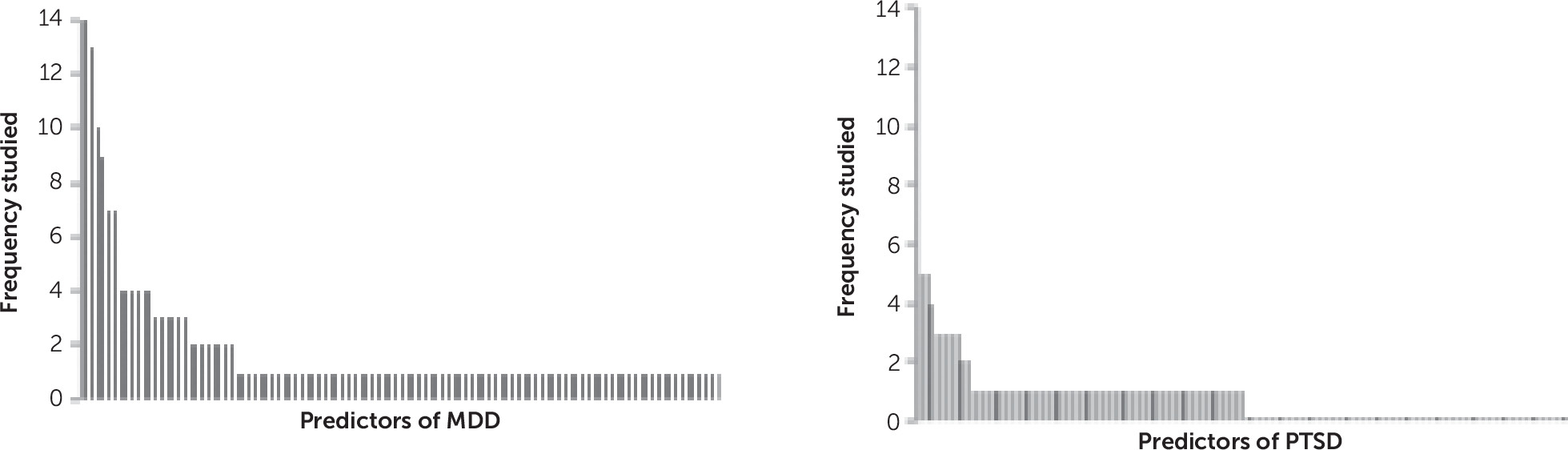
Narrative Synthesis of Univariable Predictors
Narrative Synthesis of Multivariable Models
| Study | Timing Model Use | Number of Patients | Number of Casesb | Number of Candidate Predictors | Selection Procedure of Predictors | Statistical Model | Outcome Measurement and Timing | Summary Statistics | Final Predictors in Model |
|---|---|---|---|---|---|---|---|---|---|
| MDD | |||||||||
| Ashman et al.54 | Unknown | 188 | 35; 24; 21c | 3 | Not reported | Linear random effects longitudinal model | SCID-I at 3 m to 4 y | Not reported | Age (OR: 1.00; p=0.77), time postinjury (OR: 0.88, p=0.23) and time of enrollment in the study (OR: 0.59, p<0.001) |
| Federoff et al.83 | ED | 64 | 17 | 14 | All CT lesion location variables measured | Logistic regression model with backward selection (p>0.05) | PSE at 1 m | χ2(6)=31.39, p=0.0001 | Left hemisphere (b: –2.84, p=0.04); |
| right hemisphere (b: 2.40, p=0.03); | |||||||||
| cortical (b:–3.67, p=0.01); | |||||||||
| frontal (b:–3.58, p=0.01); | |||||||||
| left anterior (b: 5.90, p=0.0003); | |||||||||
| parietal-occipital (b: 3.75, p=0.009) | |||||||||
| Gould et al.42 | At discharge | 122 | 40 | 7 | Not reported | Two logistic regression models—(1) preinjury variables; (2) injury-related variables. Significant variables were entered into a final regression model. | SCID-I at 12 m | Nagelkerke R2=0.20; correct classification rate: 70.7% | Preinjury counseling (OR: 2.34, p=0.073); |
| limb injury (OR: 4.07, p=0.009); | |||||||||
| depressive disorder at initial assessment (OR: 6.04, p=0.039) | |||||||||
| Levin et al.44 | 1 wk | 129 | 15 | 8 | Not reported | Logistic regression with backward selection (p>0.05) | SCID-I at 3 m | AUC=0.86 | Age (OR: 1.05; 95% CI: 1.00 to 1.1); |
| CES-D score at 1 wk (OR: 1.11; 95% CI: 1.04 to 1.17); abnormal CT scan (OR: 7.68; 95% CI: 1.36 to 43.48) | |||||||||
| Rapoport et al.45 | ED | 210 | 35 | 11 | Significant differences in univariable analyses | Hierarchical logistic regression model with time postinjury as covariate | SCID-I at 49 d | Nagelkerke R2=0.18 | Age (OR: 0.99, SE: 0.05, p>0.05); preinjury depression (OR: 0.28, SE: 0.67, p>0.05); substance abuse (OR: 0.25, SE: 0.67, p<0.05); time postinjury (OR: 1.00, SE: 0.001, p>0.05); gender (OR: 0.50, SE: 0.52, p>0.05); employment (OR: 0.49, SE: 0.71, p>0.05); education (OR: 0.52; SE: 0.48, p>0.05), family history of depression (OR: 0.28, SE=0.67, p>0.05); medical history (OR: 1.49, SE: 0.55, p>0.05); focal CT abnormalities (OR: 0.77, SE: 0.55, p>0.05); mechanism of injury (OR: 1.66, SE: 1.62, p>0.05) |
| Whelan-Goodinson et al.52 | ED | 100 | 46 | 13 | Significant in univariable analyses | Logistic regression model | SCID-I at 0.5 to 5 y | χ2(6)=29.10, p<0.001, Nagelkerke R2=0.35; correct classification absent depression: 80.4%; correct classification presence depression: 67.4%; overall correct classification: 74.2% | Gender (B=0.48; p=0.10); pain (B=–0.97, p=0.06); postinjury unemployment (B=0.48; p=0.39); preinjury depression (B=1.87; p=0.01); years of education (B=1.87; p=0.01); time postinjury (B=0.32, p=0.06) |
| PTSD | |||||||||
| Alway et al.37 | ED | 203 | 27 | 5 | Not reported | Multivariable random-effects logistic regression model adjusting for time postinjury | SCID-I at different follow-up points, 3 m to 5 y | Not reported | Age (OR: 0.99; 95% CI: 0.95 to 1.03); female gender (OR: 0.31; 95% CI: 0.05 to 2.08); years of education (OR: 1.06; 95% CI: 0.80 to 1.42); preinjury psychiatric disorder (OR: 0.84; 95% CI: 0.23 to 3.15); PTA (days; OR: 0.98; 95% CI: 0.95 to 1.02) |
| Ashman et al.54 | Unknown | 188 | 30; 18; 21c | 3 | Not reported | Linear random- effects longitudinal model | SCID-I at 3 m to 4 y | Not reported | Age (OR: 0.98; p=0.22), time postinjury (OR: 1.07, p=0.74), and time of enrollment in the study (OR: 0.59, p=0.003) |
| Caspi et al.50 | 2.9 y postinjury | 120 | 22 | 4 | Not reported | Logistic regression model adjusted for co-occurring depressive (BDI) and anxiety (BAI) symptoms | SCID-I at 3 y | Goodness of fit: 83.42, p<0.001; Nagelkerke R2=0.42, p<0.001 | Memory for the traumatic event (OR: 2.8; 95% CI: 1.8 to 8.9); male gender (OR: 0.5, p>0.05); history of psychiatric illness (OR: 0.5, p>0.05), age (OR: 1.2, p>0.05) |
| Gil et al.35 | 1 m postinjury | 120 | 17 | 16 | Significant in univariable analyses | Logistic regression model with variables that had shown significant association in univariable analyses | SCID-I at 6 m | Nagelkerke R2=0.38, p<0.001 | Memory of traumatic event (OR: 2.2, 95% CI: 1.0 to 10.1); |
| acute posttraumatic symptoms (CAPS; OR: 5.3; 95% CI: 1.1 to 9.3); acute posttraumatic symptoms (PSS; OR: 5.2; 95% CI: 1.0 to 9.4); depressive symptoms (1 wk; OR: 5.1; 95% CI: 1.0 to 9.2); | |||||||||
| anxiety symptoms (1 wk; OR: 4.9; 95% CI: 1.0 to 9.1), history of psychiatric disorders (OR: 3.7; 95% CI: 1.1 to 8.9) | |||||||||
Discussion
Conclusions
Acknowledgments
Supplementary Material
- View/Download
- 481.25 KB
References
Information & Authors
Information
Published In
History
Keywords
Authors
Funding Information
Metrics & Citations
Metrics
Citations
Export Citations
If you have the appropriate software installed, you can download article citation data to the citation manager of your choice. Simply select your manager software from the list below and click Download.
For more information or tips please see 'Downloading to a citation manager' in the Help menu.
View Options
View options
PDF/EPUB
View PDF/EPUBLogin options
Already a subscriber? Access your subscription through your login credentials or your institution for full access to this article.
Personal login Institutional Login Open Athens loginNot a subscriber?
PsychiatryOnline subscription options offer access to the DSM-5-TR® library, books, journals, CME, and patient resources. This all-in-one virtual library provides psychiatrists and mental health professionals with key resources for diagnosis, treatment, research, and professional development.
Need more help? PsychiatryOnline Customer Service may be reached by emailing [email protected] or by calling 800-368-5777 (in the U.S.) or 703-907-7322 (outside the U.S.).