Toxic leukoencephalopathy (TL) is a disorder of brain white matter caused by exposure to leukotoxic agents. Formally described at the turn of the 21st century,
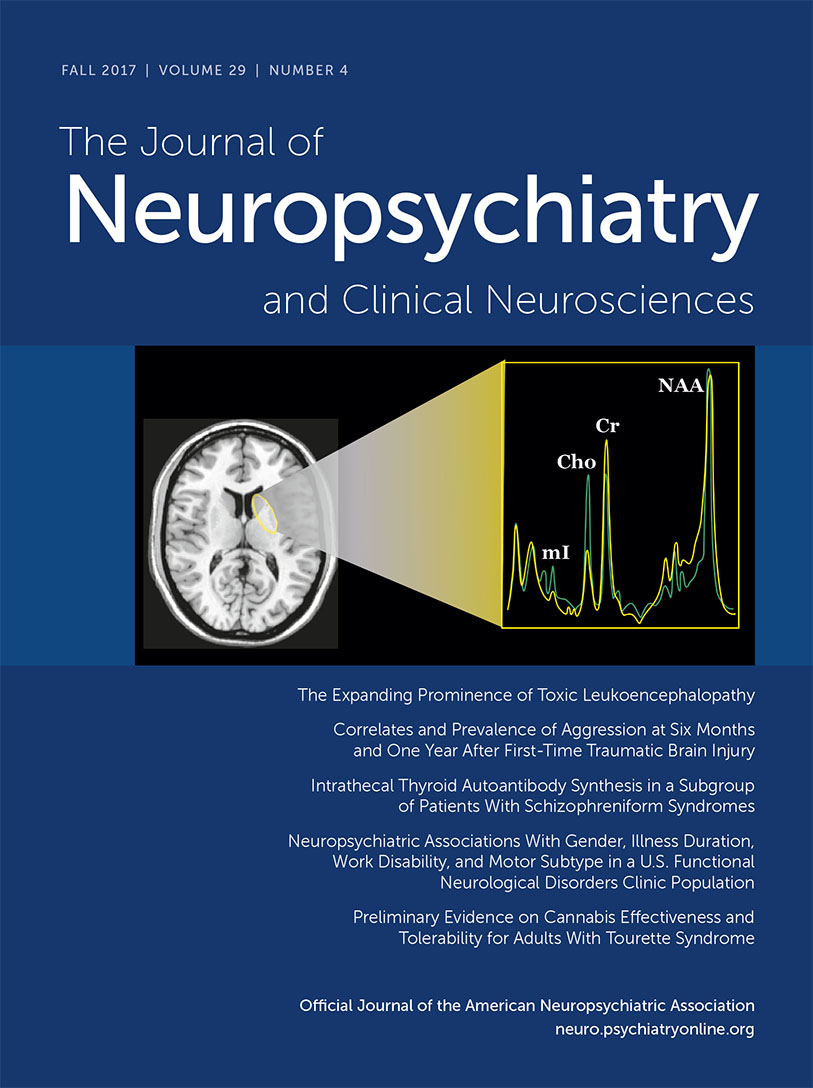
1 TL has become increasingly evident to clinicians since the early 1980s because of the advent of magnetic resonance imaging (MRI), which provided unprecedented capacity to view the brain white matter in vivo.
2 Before the application of MRI, toxic disorders of the brain were recognized neuropathologically but could not be reliably localized to specific brain regions premortem; in contrast, the detailed depiction of white matter afforded by MRI revealed a host of leukotoxic syndromes during life that had previously been obscure.
1 This trend continues today as MRI and its derivative technique, diffusion tensor imaging (DTI
3), are widely employed, and an expanding spectrum of leukotoxins is now being encountered in clinical practice. The neurobehavioral consequences of TL range from mild, transient cognitive dysfunction to stupor, coma, and death, highlighting the great diversity of clinical presentations and outcomes. Moreover, toxic injury to the white matter may have important neurobehavioral implications long after the exposure occurs.
The concept of TL also offers a useful avenue to understanding how white matter contributes to the higher functions of the brain. White matter-behavior relationships can be readily analyzed in individuals with leukotoxic exposure. Whereas neuropathological documentation of toxic white matter injury remains the most secure method to establish the leukotoxicity of a given agent, neuroimaging is far more practicable in most cases and adds critical information in exposed individuals. As clinical and research reports in this area accumulate, the propensity of TL to impact cognitive function in a wide variety of clinical settings is increasingly clear. The study of TL thus broadens the understanding of specific leukotoxic syndromes while also enhancing our knowledge of the role of white matter in cognition.
This focused review offers an update on TL, highlighting key developments with special relevance to clinical care and white matter-behavior relationships. Whereas well-recognized leukotoxins are included in this account, new white matter toxins are regularly being identified, and this field continues to evolve rapidly as MRI and DTI are applied to the study of known or suspected clinical neurotoxic disorders.
Background
Leukotoxicity from a variety of white matter insults has long been appreciated, and radiation, cancer chemotherapy, and other causes of white matter toxicity were recognized before the MRI era. The syndrome of TL, however, began to be investigated formally in the early 1980s with the first MRI demonstration of leukotoxic injury, most notably the dramatic effects exerted by toluene abuse on the cerebral and cerebellar white matter.
4–8Toluene is the major solvent in spray paint, and this legal and inexpensive product is one source of a common form of substance misuse known as inhalant abuse. Study of inhalant abusers exposed to heavy and prolonged inhaled levels of toluene disclosed a striking clinical syndrome of dementia, ataxia, cranial nerve signs, and corticospinal dysfunction in association with widespread cerebral and cerebellar white matter disease on MRI.
4,5 Dementia was the most disabling feature of this syndrome,
4 and detailed neuropsychological testing demonstrated that the degree of cognitive dysfunction was correlated with the extent of leukoencephalopathy on MRI.
6 As autopsy data from exposed individuals became available, widespread white matter pathology with prominent myelin loss became evident,
7,8 and the absence of significant cortical or subcortical gray matter pathology led to the conclusion that selective toxic injury to white matter could produce profound cognitive loss, including dementia.
4–8 Indeed, the toxic effect of toluene on white matter was a major impetus leading to the proposal of white matter dementia as a distinct category of dementing illness.
9 As time progressed, subsequent clinical
10 and neuropathological studies
11 confirmed the significance of white matter injury as a cause of cognitive dysfunction and dementia in toluene abusers.
Later, as a more comprehensive understanding of leukotoxicity was acquired, it became clear that four categories of white matter injury can be usefully delineated: radiation, therapeutic drugs, drugs of abuse, and environmental toxins (
Table 1). These categories include many agents that can be encountered at any age and in many clinical settings, and can produce a wide range of neurobehavioral, neuroimaging, and neuropathological severity.
1 As a general rule, these syndromes reflect the impact of diffuse white matter involvement, as leukotoxins tend to damage their target wherever it is found. Whereas the pathophysiology of leukotoxic injury is not well understood in most cases, white matter is vulnerable to toxic injury because of the many sites of toxicity offered by the roughly 135,000 km of myelinated axons in the brain,
12 the relatively low vascular perfusion of white matter,
13 and the high metabolic demand of oligodendrocytes as they function to maintain the myelin sheath.
13 The young and old are particularly at risk, largely related to the normal developmental trajectory of brain myelination, by which white matter reaches its maximal volume in midlife but is less well developed—and hence more susceptible to injury—early and late in life.
13 Another key factor is the lipophilicity of many toxic compounds enabling their entry into the lipid-rich brain,
12 which is particularly relevant to the growing problem of substance abuse. With these principles in mind, the four categories of leukotoxic agents will be discussed in turn, with updates on recent developments and implications for future investigation.
Radiation
Cranial irradiation is commonly used for the treatment of cancer, both within and outside the brain, and leukoencephalopathy has come to be appreciated as a major complication of cerebral radiotherapy.
14 Indeed, radiation delivered to the brain is likely the most familiar cerebral white matter toxin. This form of toxicity is generally recognized to occur in one of three patterns, as recognized by Sheline almost four decades ago: 1) acute encephalopathy related to blood-brain barrier breakdown and patchy, reversible white matter edema; 2) an early delayed syndrome (up to 6 months postirradiation) with widespread white matter edema and demyelination; and 3) a late delayed syndrome (6 months to several years after irradiation) featuring widespread demyelinative necrosis with loss of both myelin and axons.
15 In the past, one of these syndromes could be expected in more than 50% of treated patients, but with newer treatment protocols, involving total radiation doses of no more than 60 Gy,
14 these complications have become less common. White matter injury from radiation nevertheless remains important; whereas the acute and early delayed syndromes—manifested by characteristic features of confusion and somnolence, respectively—are typically reversible, the late delayed syndrome typically produces progressive dementia and in some cases death.
14,15The relationship between radiation leukoencephalopathy and cognitive impairment has become clarified with recent studies, and the contribution of white matter damage has gained increasing support.
14–18 The neuropathology of radiation injury is thought to involve widespread cerebral hemispheric white matter damage of varying severity,
16 and the major nonneoplastic targets of radiation are thought to be vascular endothelial cells and oligodendrocytes,
14 damage to both of which can plausibly result in white matter damage. Consistent with these observations, neuropsychological study of irradiated patients has disclosed prominent deficits in processing speed, executive function, and attention, with sparing of language,
17 consistent with the profile of white matter dementia.
9 While the simultaneous effects of cancer chemotherapy often complicate the study of radiation injury, a recent prospective neuroimaging study found that primary central nervous system (CNS) lymphoma patients treated with both radiation and methotrexate had more extensive white matter damage and greater deficits in attention, executive function, motor speed, and memory than those treated with methotrexate alone.
18 White matter injury, however, may not be the only route to cognitive loss from radiation, as hippocampal injury has been observed in animal models and postulated to impact declarative memory function in humans.
14 Whereas combined white matter and hippocampal toxicity remains conceivable, clinical studies have generally demonstrated a retrieval rather than an encoding deficit,
19–21 a pattern more consistent with white matter injury.
14,17–21 White matter injury from radiation is thus without question, but more study is needed to clarify the range of radiation effects on the brain and cognition.
Therapeutic Drugs
A large number of therapeutic drugs can lead to leukoencephalopathy (
Table 1). The majority of these drugs are used for the treatment of cancer, arising either within the brain or outside the CNS. Many such agents can cause this problem, but one notable exception is temozolomide, commonly used for the treatment of low-grade gliomas.
14 Higher doses and intrathecal and intraventricular administration of leukotoxic drugs are associated with more extensive white matter injury.
14 As with radiation, cancer chemotherapeutic drugs can exert acute and chronic effects on the white matter.
14 Well-known to neurologists is the reversible posterior leukoencephalopathy syndrome, related to many anticancer drugs, which is thought to result from transient white matter edema.
14 Chronic effects on cognition are also recognized, and whereas the popular term “chemobrain” for these effects has promulgated uncertainty about the legitimacy of this syndrome, cognitive loss and leukotoxicity from cancer chemotherapy has increasing support from clinical,
14 neuropsychological,
22 neuroimaging,
14,23 and neuropathological
24 studies indicating that TL can occur as a result of treatment with these drugs. MRI has disclosed an increased burden of white matter hyperintensities in patients so treated,
14 and still more compelling is the emergence of DTI findings suggesting that loss of microstructural white matter integrity can produce cognitive dysfunction in these patients.
23 The pattern of cognitive deficits closely resembles that of radiation leukoencephalopathy, with slowed processing speed, executive dysfunction, and poor concentration being most apparent, and, like radiation, cancer chemotherapeutic drugs are thought to produce mainly retrieval rather than encoding deficits in declarative memory.
22 As with radiation, toxic effects on the hippocampus have been suspected from study of animal models,
14 but the profile of cognitive deficits in these intoxications, similar to radiation leukoencephalopathy, is consistent with that of white matter dementia.
9 Further study is needed to elucidate the extent to which gray matter involvement results from cancer chemotherapy.
Not surprisingly, because both radiation and cancer chemotherapy exert prominent effects on white matter, and the two modalities are often used together, additive leukotoxicity is widely acknowledged. Although no comparative study is available to document this synergy, the toxic effects of combined radiotherapy and chemotherapy seem to be more pronounced than with either modality alone.
14,18 The most striking example of this conjoined leukotoxicity is disseminated necrotizing leukoencephalopathy that produces a fulminant course and death associated with multifocal coagulative necrosis in the cerebral white matter.
25Other therapeutic drugs occasionally cause TL, including the immunosuppressive medications cyclosporine
26 and tacrolimus,
27 and the antimicrobials amphotericin B,
28 hexachlorophene,
29 and metronidazole.
30 Cognitive dysfunction occurs with these intoxications, but details regarding the pattern and severity of impairment, neuroimaging characteristics, neuropathological features, and pathogenesis are limited by the small number of cases.
Drugs of Abuse
Far more common than the syndromes of white matter toxicity resulting from therapeutic intent is TL consequent to substance abuse. As reviewed above, the work on toluene abuse in inhalant abusers led to the first description of TL,
1 and was crucial for the emerging understanding of white matter dementia.
9 Toluene was for a time the only leukotoxin that was imageable in vivo, and its widespread effects on white matter stood as an instructive model of TL. Since then, however, a wide variety of other abusable substances have been identified with MRI to exert toxic effects on white matter. As with radiation and chemotherapy, some understanding of white matter toxicity in substance abuse had been achieved before the advent of MRI, but the capacity to view the white matter in life using large numbers of exposed individuals proved to be pivotal. In this era of increasing substance abuse, the injury to white matter that can follow exposure to many licit and illicit substances represents an alarming complication.
To begin, it is important to emphasize that study of this area is fraught with methodological challenges. Substance-specific effects on the brain are difficult to differentiate from the effects of other drugs or adulterants, and lifestyle variables such as malnutrition, infections, and systemic diseases are common in drug abusers.
31 Moreover, neuropathology is rarely available, and when cases have been studied, brains often display combined effects of multiple substances and comorbid disorders, such as metabolic encephalopathy and traumatic brain injury. A recent review of the neuropathology of drug abuse acknowledged these problems, and concluded that interacting toxic, vascular, and hypoxic effects are typically found, with additional evidence of inflammation in the white matter suggested by the presence of activated microglia.
31 While it is clear that much remains to be learned, one common theme is that abusable substances generally gain ready access to the brain by virtue of their high lipid solubility.
32 This lipophilicity clearly plays a central role in the pathogenesis of toluene leukoencephalopathy,
8 and, to invoke another example, it accounts for the predilection of marijuana for the white matter, where endocannabinoid receptors are abundant.
33 Thus it is not surprising that TL related to abusable drugs is being increasingly recognized. A brief review of recent observations in this area follows.
A very commonly abused substance is ethanol. Alcohol is of course well known to cause toxic injury of the brain, peripheral nervous system, and muscles, and traditional teaching emphasizes the role of thiamine deficiency in the pathogenesis of cognitive impairment. It is clear, however, from neuropathological study that white matter volume loss is the most common sequel of long-standing heavy alcohol abuse, even without thiamine deficiency.
34 Thiamine deficiency may produce further reduction in white matter volume, but damage from alcohol alone is sufficient to produce toxic injury.
34 Confirming these neuropathological observations, a meta-analysis of 19 MRI volumetric studies including more than 1,300 individuals with alcohol use disorder found significant reduction in white matter volume compared with controls.
35 Intriguingly, some support was also found for recovery of white matter volume and cognitive function with sustained abstinence,
35 suggesting that alcohol leukotoxicity may be potentially reversible. A good outcome with abstinence is not always possible, however, and severe and irreversible dementia is usually seen in Marchiafava-Bignami disease, a rare complication of chronic alcoholism featuring atrophy and necrosis of the corpus callosum and other white matter tracts.
36Among the most significant toxic chemical exposures worldwide is tobacco smoke, but study of its toxic effects must contend with more than 4,700 compounds inhaled in the act of cigarette smoking.
37 Nicotine, the primary constituent of tobacco smoke leading to long-term use and addiction, improves attention, working memory, and executive function acutely, but most studies of chronic smokers find lower cognition, and some find a higher risk of Alzheimer’s disease (AD) and vascular dementia (VaD).
37 The mechanisms of neurotoxicity are unclear, but oxidative stress, inflammation, and vascular disease have been proposed in the pathogenesis of AD as well as VaD.
37 Injury to both gray and white matter has been suspected, but white matter involvement is more obvious because most MRI studies have found increased burden of white matter hyperintensities in smokers, likely via vascular effects.
37 Changes in white matter microstructure have also been found with DTI, and, interestingly, increased fractional anisotropy (FA) has been consistently noted in young smokers, while decreased FA has been found in older smokers.
38 These paradoxical findings may be reconciled by acknowledging likely vascular injury from tobacco smoke in older persons while postulating the additional factor of a promyelinative effect of nicotine in adolescence.
38A wide range of commonly abused drugs has been observed to produce MRI white matter hyperintensity or DTI microstructural changes in association with acute or chronic exposure. The literature in this area includes several case reports with brain MRI documentation, and systematic clinical study of leukotoxicity has also appeared. TL has been observed in association with the benzodiazepine alprazolam,
39 heroin,
40 morphine,
41 fentanyl,
42 opiate addiction,
43 cocaine,
44 amphetamines,
45 methamphetamine,
46 methylenedioxymethamphetamine (MDMA),
47 and psylocibin.
48 The potential hazard to white matter posed by these drugs is underscored by the frequency of their abuse; amphetamines, for example, are the most commonly abused prescription drugs by adolescents and young adults, and second only to marijuana in popularity as an illicit drug in these age groups,
45 while opiate addiction has recently been estimated to affect some 2.5 million adults in the United States.
49 In none of these intoxications, however, is the mechanism of white matter injury well understood. To illustrate the challenge of elucidating the pathogenesis of leukotoxicity, a detailed neuropathological report of spongiform leukoencephalopathy related to heroin inhalation via the practice of “chasing the dragon” appeared in 1982.
50 Vacuolating myelinopathy with oligodendroglial damage was observed at autopsy, but the pathophysiology of leukotoxic injury in this disorder was not established and remains elusive today. While the entry of all these substances into the white matter is likely explained in large part by their high lipophilicity,
32 the mechanisms by which they produce injury are complex and likely variable.
31An abusable substance deserving more focused attention because of its widespread popularity is marijuana. The most commonly used illicit drug on earth, marijuana recently accounted for about 75% of all illegal drug use in the United States
51; with recent legalization in many areas, this substance is now becoming more commonly consumed without restriction. Among the many controversies surrounding marijuana is what constitutes abuse, and, indeed, many medicinal uses of this drug are being explored. Hazards such as acute intoxication, dependence, psychosis, pulmonary injury, and driving risk, however, suggest that this drug is not benign, and adverse cognitive effects have been increasingly examined.
51The active ingredient of marijuana causing euphoria is delta-9-tetrahydrocannabinol (THC), but
Cannabis sativa contains more than 60 other cannabinoids and at least 400 other compounds,
51 rendering study of neurotoxicity challenging. However, because THC is highly lipophilic,
33 and endocannabinoid receptors are abundant in white matter,
33,51 the development of leukotoxicity can plausibly be hypothesized.
Volumetric MRI studies have been inconsistent in associating white matter volume loss with marijuana,
52 but microstructural white matter changes identified with DTI have been more informative. In young cannabis users (18–20 years old at baseline) who were studied with DTI, 2-year follow-up showed that greater cannabis use produced lower FA and higher radial diffusivity (RD) in several association tracts and the corpus callosum, and was associated with lower verbal learning as measured by the Rey Auditory Verbal Learning Test.
52 Similarly, in a large DTI study of 466 adults (mean age: 29 years) from the Human Connectome Project, earlier marijuana use was associated with decreased coherence in the right superior longitudinal fasciculus, lateral prefrontal white matter, and corpus callosum; voxel-based morphometry (VBM) analysis in the same cohort showed no effect on cortical volumes.
53 Moreover, other investigators found no VBM differences among marijuana users in the hippocampus, amygdala, nucleus accumbens, and cerebellum,
54 further suggesting that the toxic effects of marijuana may be largely or exclusively confined to the white matter. Although the adverse cognitive effects of marijuana remain controversial, evidence is mounting that both acute and chronic exposure to cannabinoids impairs cognition, mainly in the domains of attention and memory, and that these effects are especially pronounced in adolescents.
55,56 In this light, the accumulating evidence that young marijuana users may develop both lower white matter integrity and impaired cognitive function underscores the likelihood of a special vulnerability of the adolescent brain to toxic white matter injury.
55,56Environmental Toxins
A number of environmental toxins display a predilection for the white matter. These agents represent a diverse group with obscure mechanisms of leukotoxicity, and it is likely that many other agents in the environment are capable of similar effects. Among the best known of these insults is carbon monoxide (CO), exposure to which results from incomplete combustion of hydrocarbons, and which produces tissue hypoxia because it binds to hemoglobin with 200 times the affinity of oxygen.
57 Inadequately oxygenated blood leads to anoxic anoxia, which in turn produces acute effects on consciousness related to global brain dysfunction. Beyond its immediate neurotoxic effects, however, CO poisoning is one of the most clearly established antecedents to delayed posthypoxic leukoencephalopathy (DPHL), a syndrome characterized by lethargy, confusion, and cognitive loss in association with confluent white matter hyperintensity on MRI that appears 2–40 days after the acute syndrome resolves.
58,59 Autopsy studies of DPHL have shown severe diffuse demyelination, with preservation of axons.
58,59 Acute CO poisoning prominently injures the globus pallidus, which likely contributes to the parkinsonism often seen in patients with DPHL.
57 A key challenge for clinicians is being aware of the delay between CO poisoning and the development of DPHL. Whereas the pathophysiology explaining this hiatus is not well understood, hypotheses include 1) inhibition of cytochrome oxidase with impaired aerobic respiration and diminished myelin turnover, 2) delayed apoptosis of oligodendrocytes related to hypoxic-ischemic glutamate excitotoxicity, 3) inflammatory myelinopathy related to delayed microglial activation, and 4) pseudodeficiency of aryl sulfatase A predisposing to leukotoxicity.
59 Although some patients have persisting cognitive dysfunction, many will improve substantially within 3–6 months with supportive care, in keeping with the neuropathology of preserved axons despite diffuse demyelination.
58,59Rare cases of fatal carbon tetrachloride
60 and arsenic
61 poisoning have been reported. In these patients, acute exposure was followed by rapid cognitive decline advancing to coma and death, with autopsy findings of widespread hemorrhagic white matter necrosis. Far more common is lead poisoning, which has recently been implicated in leukotoxicity. Exposure to lead remains a significant public health problem, despite the banning of lead from gasoline in the late 1970s, both in adults and children. Both organic (tetraethyl and tetramethyl) and inorganic lead are toxic, although the former more readily reaches the brain because of its higher lipophilicity. A study of former organolead workers found that peak tibia lead concentration was associated with increasing white matter lesion grade on MRI and progressive cognitive decline.
62 Exposure in early life may also be deleterious, as young adults studied with DTI were found to have widespread FA declines in white matter that were associated with mean childhood blood levels.
63 Moreover, observations that organic lead not only affects white matter but may also lower total gray matter and brain volume, and produces neurofibrillary tangles in animal studies,
64 raise intriguing questions about the possible links between lead leukotoxicity and neurodegenerative disease.
Pesticides constitute another group of leukotoxic agents, as they share strong lipophilicity with many other white matter toxins.
65 One such agent is paradichlorobenzene, a hydrocarbon similar to toluene found in mothballs and toilet cakes. As in inhalant abusers exposed to high levels of toluene,
4–8,10,11 ingestion of paradichlorobenzene can produce TL. A woman with mental illness who had been chronically ingesting this compound orally was observed to develop dementia and widespread MRI white matter changes similar to those induced by toluene.
66 Another pesticide noted to be capable of causing acute TL is chlorfenapyr, a pyrrole used for mosquitoes resistant to dichlorodiphenyldichloroethane (DDT).
67 Similar toxic effects on white matter have been seen with sodium monofluoroacetate, a rodenticide employed to control coyotes in the U.S. and possums in New Zealand.
68 As pesticides are resistant to degradation and exhibit high bioaccumulation,
65 these cases of acute TL raise the possibility that less striking but potentially important long-term effects on white matter may develop. The half-life of dichlorodiphenyldichloroethylene (DDE), the metabolite of DDT, is 8–10 years,
69 and storage in adipose tissue leads to continual leaching of DDE into the bloodstream and ongoing delivery to the lipid-rich brain.
70 A large prospective study found that occupational exposure to organophosphate and organochlorine pesticides was associated with an increased risk of dementia and AD.
71 Moreover, a group of major organochlorines—DDT, DDE, β-hexachlorocyclohexane, transnonachlor, oxychlordane, and heptachlor—has been associated with lower cognition in 644 nondemented elders.
70 It has also been shown that elevated serum DDE is associated with increased AD risk and lower Mini-Mental State Examination (MMSE) score, especially in individuals harboring an apolipoprotein (APOE) ε4 allele, and both DDT and DDE increase amyloid precursor protein (APP) levels in cell culture.
69 Taken together, these data suggest the possibility that TL may be a preliminary disorder or pathogenic contributor to dementia, including AD.
Finally, another area of potentially far-reaching importance with respect to environmental white matter injury is air pollution. As with lead toxicity, neurodegenerative pathology may follow early white matter injury related to polluted air. Similar to the problems encountered with tobacco smoke and marijuana, however, air pollution presents major obstacles to neuroscientific study because of its diverse array of potential toxins. Polluted air is a complex mixture of particulates, gases, organic compounds, and metals capable of assaulting the CNS and producing an array of adverse effects.
72 The many components of air pollution are thought to reach the brain directly via the respiratory tract or the olfactory system. Most concerning for central neurotoxicity is particulate matter, which is generally classified as coarse (2.5–10
μm in diameter), fine (0.1–2.5
μm), and ultrafine (<0.1
μm).
71 Fine and ultrafine particles pass through the lungs and the olfactory system, and these particles are thought to convey a variety of adsorbed metals and other potentially toxic compounds into the brain via a “Trojan horse” effect.
72 The toxic effects of the various constituents of air pollution on the brain are not well understood, but evidence exists for the importance of neuroinflammation, oxidative stress, cerebrovascular disease, and neurodegeneration,
72 and leukotoxicity may be central to all.
As a first observation, older adults living in areas with high concentrations of fine particulate matter have been found to make significantly more errors on tests of working memory and orientation.
73 Dementia has also been linked with air pollution, and a large population-based Canadian cohort study found that living close to heavy traffic was associated with a higher incidence of dementia but not Parkinson’s disease or multiple sclerosis.
74 Moreover, a recent review found that almost all epidemiological studies on this issue have reported at least one adverse association between air pollution and a dementia-related outcome.
75 Whereas both white and gray matter pathology related to air pollution may be implicated in the etiopathogenesis of cognitive dysfunction, provocative volumetric MRI evidence from the Women’s Health Initiative Memory Study recently documented that older women with greater exposure to fine particulate matter had smaller white matter but not gray matter volumes.
76 Subsequent MRI analysis from the same group of subjects using VBM found that particulate matter exposure was associated with both white and gray matter volume loss, but that the former involved all lobes of the cerebrum, whereas the latter was confined to the frontal cortex.
77White matter pathology resulting from air pollution could occur via several pathophysiological processes. First, neuroinflammation may be triggered by proinflammatory effects of particulate matter that generate activated microglia,
72 and it is relevant in this regard that microglia, the resident immune cells of the brain, are significantly more abundant in white matter than in gray matter.
78 Thus, inflammatory effects may initially be more pronounced in the white matter, establishing a foundation for more extensive inflammatory injury in cortical and other gray matter regions as the process advances. Next, oxidative stress is a common pathophysiological process in aging and dementia, and could be initiated or exacerbated by ozone, a gaseous component of air pollution that is known to generate reactive oxygen species.
72 Furthermore, iron, a metal present in air pollution, is also associated with oxidative stress,
79 and iron-rich nanoparticles (magnetite) have been found in the frontal cortices of people exposed to air pollution.
80 White matter was not examined in this study,
80 but iron is the most abundant element in the brain, oligodendrocytes have the highest iron content of any brain cells, and 70% of brain iron is associated with white matter.
81 Third, cerebrovascular disease has been related to air pollution,
82 and frontal lobe white matter has been shown to be a selective target of ischemia related to air pollution in both children and dogs exposed to highly polluted air.
83 In addition, white matter pathology may be induced indirectly by air pollution that does not enter the brain, as cerebrovascular disease stemming from air pollution may produce an increased burden of white matter hyperintensities.
75 Finally, neurodegeneration in the brain could be a later result of leukotoxicity from air pollution, as amyloid plaques have been found in humans and animals with prior exposure.
72,83A pathogenetic progression implied by these observations is that brain myelin is affected first, and the characteristic neuropathology of AD appears later as a result of a homeostatic response of the brain that eventually leads to amyloid toxicity in the cortex and dementia as the capacity for effective brain repair is overwhelmed.
13 Clinical support for this sequence of events has recently appeared from epidemiological research showing that among more than 95,000 older Taiwanese individuals followed prospectively for 10 years, a 211% increased risk of AD was found per increase of 10.91 ppb in ozone exposure, and a 138% increased risk of AD was found per increase of 4.34% µg/m3 of fine or ultrafine particulate matter exposure.
84Prevention, Treatment, and Prognosis
The importance of preventing TL needs little emphasis, as it is clear that avoiding or minimizing leukotoxic insult(s) is a high priority. In recent years, this dictum has been successfully followed in the treatment of cancer, as reduction in the incidence of late-delayed radiation leukoencephalopathy has been noted with improved safety of radiation protocols.
14 Other iatrogenic causes of TL can be similarly addressed with cautious use of potentially leukotoxic medications. More challenging in many cases is the prevention of illicit or recreational substance abuse, and of exposure to environmental agents capable of inducing TL. Drug abuse counseling programs for adolescents and young adults, improved education to reduce leukotoxin exposure, and public policy aimed at establishing and maintaining safe levels of hazardous environmental agents can all play a crucial role.
The treatment of TL most critically revolves around elimination or reduction of toxic exposure as soon as possible, and provision of supportive care as indicated.
1 Indeed, treatment can begin only after the prompt recognition of a leukotoxic disorder, as opposed to some other cause of white matter involvement. In general, treatment of these disorders is not standardized, but specific therapies can occasionally be useful, such as corticosteroids for the acute leukoencephalopathy reaction after brain irradiation,
14 or the use of drugs such as donepezil or methylphenidate for lasting cognitive dysfunction due to radiation leukoencephalopathy.
22 Details of these interventions are beyond the scope of this review, and few data are available on the outcome of specific treatments. However, some optimism in this area is justified from the recent recognition of the phenomenon of white matter plasticity through the mechanism of activity-dependent myelination.
85 That is, in patients free of ongoing toxic exposure who have preserved axons, the exploitation of activity-dependent myelination by rehabilitative or other measures may help enhance restoration of normal white matter structure and function regardless of the specific leukotoxic exposure.
The prognosis of TL is quite variable, and depends on many factors, including the extent and duration of exposure, patient age, the integrity of hepatic and renal function responsible for rendering toxic compounds nontoxic, and comorbid medical and neurologic problems.
12 Among the better studied leukotoxins is alcohol,
34 and the possibility of restitution of white matter volume and cognitive improvement with sustained abstinence
35 offers hope that other causes of TL can be associated with similar positive outcomes. Prognostic information is variable regarding other leukotoxins, but evidence for some degree of recovery has been found after abstinence from toluene abuse.
86 In addition, a recent 15-year follow-up study of another form of inhalant abuse—gasoline sniffing—found that cognitive function returned to normal in those abusers who were abstinent.
87 In this study, abusers who had additional lead encephalopathy did not fare as well,
87 suggesting that additive leukotoxicity results in more lasting cognitive impairment. At the neuropathological level, damage to myelin is often transient, portending a good outcome, and, as a general rule, axonal damage is associated with a worse prognosis, similar to other white matter disorders, including traumatic brain injury, multiple sclerosis, human immunodeficiency virus (HIV) infection, and subcortical ischemic vascular dementia.
88White Matter-Behavior Relationships
As was delineated in its initial description,
1 TL can be classified along a spectrum of clinical, neuroimaging, and neuropathological severity. The categories of mild, moderate, and severe involvement
1 are still relevant, and reflect the variable impact of leukotoxic injury. Using the example of toluene leukoencephalopathy, TL can securely be conceptualized as a syndrome of diffuse white matter involvement in which the level of exposure generally predicts the extent of injury and the degree of neurobehavioral dysfunction.
86Whereas the original description of TL necessarily highlighted the more obvious examples of leukotoxicity, recent findings have led to the recognition of more subtle presentations of the syndrome as it has become clear that the normal-appearing white matter may harbor microstructural lesions that can only be assessed with techniques such as DTI. The emerging appreciation that conventional MRI may be insensitive to leukotoxicity at the microstructural level has helped extend the scope of TL and call attention to less overt clinical manifestations. Thus, whereas white matter dementia can be the result of TL,
9 and a fatal outcome can also be encountered in certain intoxications,
14,25 the majority of cases seen clinically are likely to be less fulminant, and in many individuals it is unclear whether leukotoxic injury has occurred at all. To illustrate the uncertainty involved in distinguishing between genuine TL and its absence, the phenomenon of chemobrain (also known as “chemo fog”) in patients who have received cancer chemotherapy has garnered considerable support from DTI,
23 in contrast to the previously reported “chronic painters’ syndrome” in workers exposed to organic solvents
89 that remains unconfirmed, even with autopsy study of exposed individuals.
90 This point is crucial, as the cognitive significance of mild white matter involvement remains incompletely understood despite the large numbers of patients who present with neuroimaging evidence implicating this component of the brain.
Much investigation lies ahead in clarifying the threshold at which toxic white matter involvement produces neurobehavioral manifestations, but this issue may be usefully addressed by invoking the concept of mild cognitive dysfunction (MCD),
91 first inspired by the study of insidious white matter pathology in systemic lupus erythematosus,
92 and intended to capture the early cognitive dysfunction associated with microstructural white matter disease. At this point, MCD is purely hypothetical, and is proposed as a research topic to distinguish the intermediate stage of cognitive dysfunction related to mild white matter involvement from both normal cognition and white matter dementia. Standardized use of the term MCD in the setting of microstructural leukotoxicity may assist in clarifying the impact of white matter toxins on cognition at an early stage when recovery is more likely, much as the concept of mild cognitive impairment has informed the study of early neurodegenerative dementia. Regardless of how this investigation proceeds, however, the work on TL has added a plethora of evidence that “corticocentric myopia”
93 with respect to the cerebral organization of cognition and emotion is to be avoided.
Long-Term Implications
The major clinical focus of TL presently involves the diagnosis and treatment of acute toxic syndromes, which can represent a wide range of symptoms and signs, as well as neurologic emergencies because of a potentially fatal outcome. These acute syndromes are being increasingly recognized by the widespread use of MRI, and more leukotoxins with the potential for this complication are likely to appear. However, the long-term outcome of individuals exposed to leukotoxins, particularly those with repeated or chronic exposures, is a topic also meriting attention. As reviewed above, evidence from the study of tobacco smoke, lead toxicity, and air pollution is beginning to suggest the possibility that long-term cognitive sequelae may result not only from lasting white matter injury but also from neurodegenerative disease that may be initiated or enhanced by leukotoxicity. Simply stated, degenerative gray matter disease may have its origin in early white matter pathology.
The most important implication of this line of reasoning is the possible contribution of TL to the pathogenesis of AD. The continuing challenge posed by this disease—and the absence of effective disease-modifying treatment—serves as a powerful motivator for considering new approaches to pathogenesis, and the myelin model of AD stands as one such effort.
13 In this context, TL may prove to be crucial. As is well known after several decades of work in the field, the amyloid hypothesis of AD dominates thinking about the pathogenesis of this very common disease.
94 In this scenario, amyloid β42 and its oligomers are deposited in the cerebral cortex, and then lead to a cascade of hyperphosphorylation of tau and subsequent neurodegeneration that culminates in dementia. Much research effort has been expended in elaborating this idea, and the majority of medications recently investigated as potential treatments for AD have involved some mechanism of action designed to prevent or reduce brain amyloid burden. Yet none of these efforts have thus far proven successful,
95 and even the presumed toxic nature of amyloid may require renewed assessment. In this discouraging situation, the field of AD may need to turn to other ideas regarding pathogenesis, and early injury to white matter, from intoxication such as described above, or other acquired insults such as vascular disease or traumatic brain injury, may prove useful.
13,96 Indeed, a fresh look at deleterious environmental factors may serve to reinvigorate the field of AD and refocus research clinical efforts on events that occur well before amyloid and its oligomers lead to the development of cortical dysfunction and dementia.
13,96Additional perspective on this topic can be gained by considering that environmental agents may also have positive effects on white matter, with secondary benefits related to the reduction of dementia risk. The commonly consumed substance caffeine serves as an example of this principle. Epidemiological studies have suggested a beneficial effect of caffeine on cognitive function in the elderly, the prevalence of white matter hyperintensities, and AD risk.
Women over 65 who consumed more than 300 mg caffeine per day had slower decline in verbal retrieval,
97 and lower MRI white matter lesion volume.
98 A review of the effect of caffeine on AD risk found that many, although not all, cross-sectional and longitudinal studies support a protective effect of caffeine on dementia and AD in older women, but with no dose-response relationship.
99 More work on these questions is clearly needed, but the notion that toxic injury to white matter may have a counterpart in environmental agents having a beneficial influence further supports the importance of considering white matter in the pathogenesis of dementia and AD.
Summary
Since its initial description as a clinical syndrome, TL has become more widely appreciated as a cause of acute and chronic neurobehavioral dysfunction. Improved recognition of the syndrome is no doubt related in large measure to the increasingly routine use of MRI in known or suspected leukotoxicity, enabling the application of a neuroimaging modality well suited to the identification of cerebral white matter disorders. Additional information is rapidly being gathered with the use of DTI, which allows a more granular visualization of normal-appearing white matter that may in fact be damaged. As experience has grown in this area of neurotoxicology, the importance of cognitive impairment and dementia as major sequelae of toxic white matter disorders
1,9 has been abundantly confirmed, and more subtle clinical manifestations are being better understood.
Whereas the recognition of acute TL has led to improved understanding and management of toxic white matter injury, the long-term sequelae of these insults may have equal if not more importance. Emerging data concerning the relationship of toxic white matter disease to the pathogenesis of dementia, particularly with respect to the role of leukotoxins present in many drugs of abuse and environment agents, suggest that medical and public policy interventions to enhance prevention may be of great significance, possibly even with respect to AD.
One aspect of this field deserving special emphasis is the relationship between white and gray matter involvement. The syndrome of toluene leukoencephalopathy offered a clear example of selective white matter pathology consequent to toxic exposure, but often toxic brain injury involves an admixture of white and gray matter pathology that complicates analysis.
100 One promising approach to this conundrum is considering the effect of toxins on the small strands of myelin within the cortex—the lines of Baillarger—and the lesser tracts coursing within and between the deep gray matter nuclei of the brain, which could explain why a putative leukotoxin appears to exert its effects on gray as well as white matter.
100 Further study with highly sensitive high field strength MRI promises to provide answers to this and other emerging questions.
In conclusion, the study of TL has steadily grown since the initial description of the syndrome, opening up new avenues of clinical and research interest with broad neurobehavioral relevance. Toxic white matter disease has proven to be a rich source of steadily accumulating information with a host of potentially transformative implications that are just coming into focus. The coming years will doubtless witness continued advances in this field, both in the realm of clinical practice and in the understanding of the role played by white matter in normal cognition.