Posttraumatic stress disorder (PTSD) is characterized by an often disabling constellation of persistent symptoms following a traumatic life experience. Symptoms include intrusive re-experiencing of the trauma via flashbacks or nightmares, emotional dysregulation, hyperarousal, and avoidant behaviors. Trauma-focused cognitive-behavioral therapy (CBT), a mainstay of PTSD treatment, often combines exposure therapy with cognitive therapy (
1). The cognitive component is aimed at challenging maladaptive trauma-related appraisals and to teach patients to think more realistically about the trauma and their symptoms. Exposure therapy is based on the theory that avoidance of negative affective states interferes with extinction learning, a process mediated by interactions between the amygdala, dorsal anterior cingulate cortex (dACC), and ventromedial prefrontal cortex (vmPFC), whereby learned threat associations are updated and extinguished when the previously learned response is not reinforced (
2). The effects of the cognitive component of trauma-focused CBT presumably depend on prefrontal regions, such as the dorsolateral prefrontal cortex (dlPFC) and dorsomedial prefrontal cortex (dmPFC), which are involved in higher order cognitive operations (
3).
Despite its apparent efficacy, response to trauma-focused CBT is incomplete, with as many as 60% of patients in some trials still meeting criteria for PTSD diagnosis following treatment (
4). Skills training in affect and interpersonal regulation (STAIR) is a particular form of trauma-focused CBT with demonstrated benefit in PTSD. When a STAIR protocol was combined with standardized exposure therapy (STAIR/exposure), full remission (Clinician-Administered PTSD Scale [CAPS] score <20) (
5) was achieved in 27% of patients, with 61% of patients no longer meeting criteria for PTSD diagnosis compared with 33% of those treated with exposure therapy alone (
6). Although individuals in the STAIR/exposure group experienced more improvement than those in exposure therapy alone, more than a third of patients still met criteria for PTSD following combined treatment. Although most patients benefit from treatment, the degree of improvement is variable. A better understanding of who is likely to benefit from particular forms of treatment may help guide treatment selection for individual patients and can lead to improved understanding of the differential mechanisms by which these treatments work.
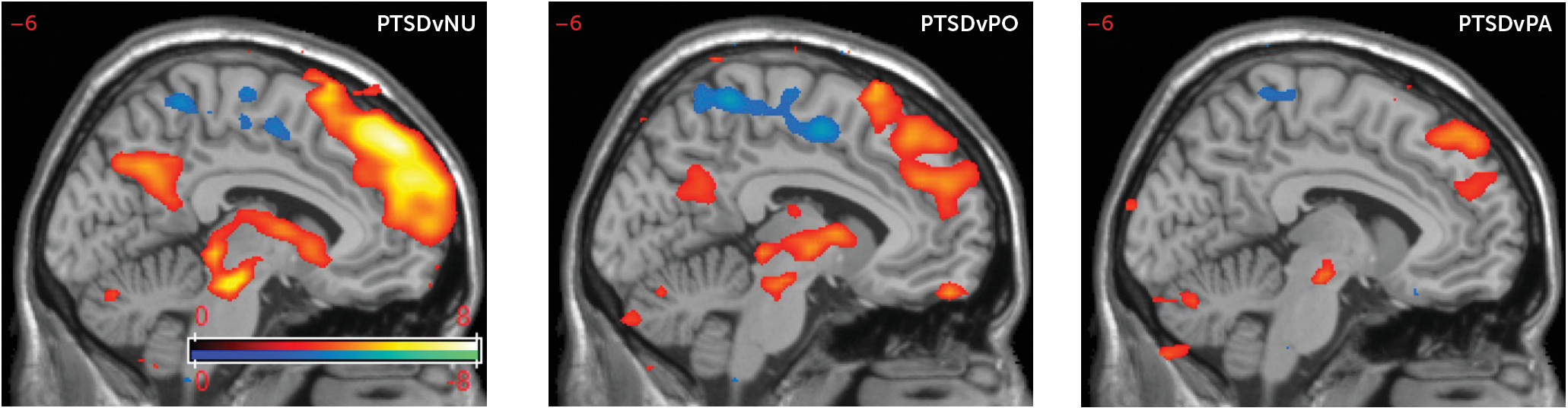
Functional neuroimaging studies have revealed differences in pretreatment brain function that are associated with subsequent CBT response, although findings may depend in part on the nature of the particular task used. Studies comparing pretreatment neural responses to emotionally negative images versus matched neutral or positive images have shown that greater activations in the amygdala (
7,
8) and dACC (
9,
10) correlate with poorer response to treatment. However, greater dACC was associated with better treatment response when it was observed in response to anticipation of negative versus positive images, in contrast to the opposite effect during image viewing (
9). Fonzo and colleagues (
8) found that when participants viewed faces depicting expressions associated with threat and fear, compared with neutral facial expressions, greater dACC activation (as well as greater activation in other frontal regions and in the anterior insula) was associated with better treatment response, an effect apparently opposite that shown by Aupperle and colleagues (
9). An opposite effect on amygdala activation in response to facial expressions associated with threat and fear compared with neutral expressions was also demonstrated in a population of adolescent girls with PTSD (
11), where CBT nonresponders demonstrated less differential amygdala activation. However, it was noted that this reflected greater activation in response to neutral stimuli among nonresponders, suggesting an overactive threat response to neutral stimuli. Studies using behavioral inhibition tasks have shown that greater activation in the dorsal striatum, prefrontal networks (
12), and inferior parietal lobule (
13) was associated with better response to treatment. In general, these studies have been interpreted as demonstrating that greater activation in emotion-responsive regions prior to treatment indicates poorer prognosis, whereas greater activation in brain areas involved in cognitive control and emotion regulation indicates better prognosis.
All of the above studies used standard emotion or cognitive tasks to probe the relevant circuitry. To our knowledge, trauma-specific stimuli have not been used in the context of an activation task for the purpose of identifying neural circuitry associated with PTSD treatment response. By way of their semantic content, visually presented trauma-specific words can convey themes that are highly personally and emotionally relevant to individuals with PTSD while controlling for low-level visual features. Trauma-related words can elicit early amygdala hyperactivation in patients with PTSD to a degree not seen with nontrauma-related emotionally negative words (
14). We hypothesized initially that amygdala activation would correlate negatively with treatment response, whereas activation in higher-order frontal lobe regions involved in emotion regulation (such as the vmPFC, dACC, and dlPFC) would correlate positively with treatment response. Thus, we sought to investigate the relationship between trauma-related brain activation and subsequent response to trauma-focused CBT. Significant correlations in these specific brain regions were not found in our analyses. However, we conducted a whole-brain analysis to address a more exploratory hypothesis: that brain activations specifically associated with reading trauma-related words, even when outside of regions typically associated with PTSD, can have relevance for how the brain processes trauma-related content during CBT and can therefore have bearing on CBT success. Certain neural responses to trauma-related content may facilitate better response to CBT, whereas others may interfere. We therefore sought to identify trauma-word-related brain activations that correlated with subsequent response to treatment.
Discussion
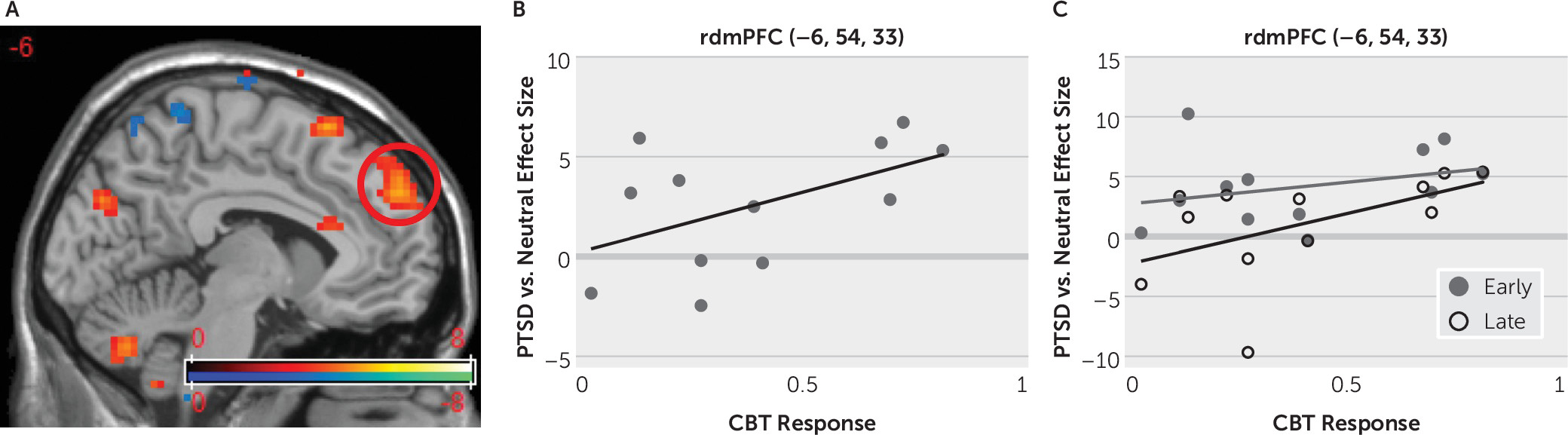
While the dACC (among other regions) has been previously highlighted in the literature on PTSD treatment response, activations in the dmPFC have received little attention as mediators of CBT response. Here, we showed that stronger activation in the rostral dmPFC in response to the reading of trauma-related words prior to treatment with CBT correlated with better response to treatment.
The portions of the medial prefrontal cortex that are dorsal and rostral to the anterior cingulate cortex, comprising the medial aspects of Brodmann’s areas 6, 8, 9, and 10, are often referred to as the dmPFC or medial frontal gyrus. The dmPFC can be further subdivided into regions with distinct functional associations. The most posterior portions of the dmPFC are concerned with motor functions and include the supplementary motor area (SMA) and pre-SMA. Anterior to this region is the mid-dmPFC, which is involved in internal monitoring of action, is particularly sensitive to error or conflict, and is involved in the regulation of behavior by monitoring the value of potential future actions (
16). Our results point toward a region of the dmPFC anterior to the mid-dmPFC, referred to here as the rdmPFC, which encompasses the medial portions of Brodmann’s areas 9 and 10 and is most closely linked with social cognition. This area has not been closely associated with emotion down-regulation as have other areas of the prefrontal cortex, such as the vmPFC, which makes strong connections with the amygdala and other limbic regions and is implicated in emotion regulation, particularly in the context of extinction of a learned threat response (
2,
17).
Although there are few direct connections between the dmPFC and amygdala, the dmPFC has been invoked (along with other brain areas such as the dorsolateral PFC and dACC) in reappraisal, a method of emotion regulation whereby a deliberate effort is made to alter the emotional interpretation of an emotionally laden stimulus. However, meta-analyses have suggested that it is primarily the mid-dmPFC rather than the rdmPFC that subserves this function (
18–
21). Why, then, might activation in the rdmPFC in response to reading trauma-related words correlate with a better response to subsequent CBT? We propose that differences in the degree of activation in this region among patients with PTSD may reflect an individual’s capacity for introspection and emotional self-awareness, psychological characteristics likely to mediate treatment response.
Among all PTSD patients in our sample about to undergo CBT, the rdmPFC was activated in response to trauma-related words but not in response to neutral words at the group level. Positive words and panic disorder-related words were activated in this region more than neutral words but less than trauma-related words. Taken together, these findings suggest that the rdmPFC may respond more strongly to personally relevant emotion stimuli. Although the stimuli were standardized across participants and were not specific to an individual’s personal history, they were chosen to reflect the experiences and preoccupations of patients with PTSD related to sexual and/or physical trauma, a history common to all of the participants in this study. The panic disorder-related words would be expected to be less personally relevant to this population. The particular relevance of the PTSD-related words may evoke stronger self-reflection compared with the other categories of stimuli.
Previous studies have demonstrated that the rdmPFC is activated by a variety of types of emotion and nonemotion tasks that involve mentalizing, or the meta-representation of one’s own or another’s mental processes or attributes (
16). For example, while viewing affectively charged photographs, the rdmPFC was activated when individuals reflected on their own feelings or on the feelings of the central character in the picture but not when asked to make a determination about whether the same pictures were taken outdoors or indoors (
22,
23). In a task in which participants were asked to either up-regulate or down-regulate their negative emotions in response to aversive images, the rdmPFC was activated with up-regulation but not with down-regulation (
24), again arguing against a direct role for this region in down-regulation of negative emotion. The activation in the rdmPFC in response to up-regulation of negative emotion in that study may have been due to the self-focused method by which half of the participants were taught in order to increase negative emotion: they were instructed to imagine themselves in the negative situation depicted in the picture. By contrast, the method by which they were taught to decrease negative emotion involved viewing the image from a more detached perspective, in which self-referential processes are expected to be less engaged. Thus, the effect of that task on the rdmPFC may have related more to the differing degree of self-examination between the two tasks rather than on the directionality of emotional self-regulation The rdmPFC demonstrates greater activity when individuals make judgments about self-attributes (mental or otherwise) compared with impersonal semantic judgments (
25) or judgments about the accuracy of impersonal factual statements (
26), further supporting a role for this region in self-referential processing. The rdmPFC also tends to be relatively active during the resting state (
27,
28), a finding that has been attributed to the types of self-generated mental activities that occur spontaneously under unconstrained resting conditions, many of which are likely introspective or self-referential (
29). Whitfield-Gabrieli and colleagues (
30) found an overlap in the rdmPFC between the self-referential network and the resting-state default-mode network.
The rdmPFC is also activated by tasks that require participants to make inferences about the attributes (
25) and mental states (
31,
32) of other people, and even of dogs (
33), suggesting a role for this region in social cognition. Taken together, the previous literature suggests that the rdmPFC is involved with meta-representation of one’s own mind or the minds of others and supports cognitive functions such as self-examination, introspection, and awareness of one’s emotional state. In fact, patients with alexithymia, a condition characterized by difficulty identifying and describing one’s own feelings and emotions, demonstrated reduced activation in the rdmPFC in response to a theory-of-mind task (
34).
The STAIR treatment module, which precedes the exposure module, aims to help patients become more aware of their emotional responses during emotional events and recall of traumatic memories (
35). During the STAIR phase of therapy, patients practice skills, including identifying and labeling feeling states and identifying and altering interpersonal schemas (
36), to enhance their capacity to use exposure therapy. It is possible, based on the evidence reviewed above, that the rdmPFC supports an individual’s capacity to practice such skills. Some research indicates that treatments that capitalize on patients’ strengths produce better outcomes (
37). Thus, patients who already have the ability to reflect on their emotions may benefit more from therapies that include self-reflective exercises, and this may be an avenue for future investigation. It remains to be seen whether individuals who have less reflective capacity can benefit more from a therapy that teaches them these skills as opposed to therapies that use more concrete behavioral strategies that may be more consistent with current skills or preferences.
Individuals differ in their ability to reflect upon their own emotions, and these intrinsic characteristics could inform the type of psychotherapy recommended. We might predict that these differences in abilities would be supported by differences in the mediating functional neuroanatomy under relevant probe conditions. Ultimately, it is hoped that functional neuroimaging at the individual level, along with psychological profiling, will be clinically useful for the design or selection of an individualized psychotherapy program.
A previous study found that amygdala BOLD responses to these linguistic stimuli in PTSD patients compared with healthy control subjects change from the early part of the task to the late part of the task, highlighting variable degrees of habituation or sensitization in patients and in healthy control subjects, depending on the stimulus type (
14). Because neural processes engaged by the stimuli change over time as the individual gains experience with the task and as the stimulus effects build, examining effects of experiment time on the BOLD responses can provide further insight into the nature of these processes. Interestingly, examination of the effects of experiment time on rdmPFC activation reveals that the correlation with treatment response is largely driven by the second half of the task. During the first half of the task, there was activation in the rdmPFC, even among poor responders, but they were less able than the stronger responders to sustain this response during the latter part of the task, and thus the rdmPFC activation during the late portion of the task demonstrated a stronger correlation with treatment response. This finding could potentially be explained by a tendency of the poorer responders (but not the stronger responders) to be unable to sustain their emotional engagement and self-reflection throughout the scanning session as a result of either fatigue or a tendency to dissociate under the stress of the repeated exposure to the emotionally distressing stimuli.
Limitations to this study include the small sample size and the fixed-effects analysis, which may limit the generalizability of the findings beyond the particular group studied. In particular, this study included only female participants with PTSD symptoms related to sexual or physical assault. It is unclear whether these findings will generalize to men or to PTSD related to other types of trauma. The lack of a control group comprised of individuals who did not undergo CBT makes it difficult to demonstrate the extent to which improvements in symptom scores were a result of treatment, but the efficacy of STAIR when combined with exposure therapy has been previously shown to be effective compared with exposure without STAIR in a randomized controlled trial (
6). Although we surmise that the rdmPFC effect can be explained by an intrinsic capacity among the strong responders toward introspection and self-reflection in the context of negative emotion, we did not assess this behavioral characteristic in our participants. Future studies might use scales such as the Self-Consciousness Scale (
38), the Self-Reflection and Insight Scale (
39), or the Toronto Alexithymia Scale (
40), to examine the extent to which these behavioral measures correlate with treatment response or rdmPFC activation.