Posttraumatic stress disorder (PTSD) may develop after severe or prolonged life-threatening events, such as those caused by war, accidents, and other traumas (e.g., fires, assault, near-drowning) (
12). Persons with PTSD often relive their traumatic event in flashbacks and/or nightmares (
13,
14). Individuals with PTSD also may experience severe anxiety when exposed to scenarios reminiscent of the original trauma and often avoid anything (mentally or physically) that reminds them of the trauma they experienced (
12). Additional symptoms of PTSD include persistent alertness and mental hyperarousal, insomnia, irritability, hypervigilance, and low concentration, as well as reckless and self-destructive behaviors (e.g., illicit drug use, risky sexual behaviors, deliberate self-harm) (
12–
14). In PTSD, the trauma-related episodes are typically followed by distressing physiological responses that result in cognitive and behavioral avoidance, a coping mechanism aimed at reducing psychological distress and physiological hyperarousal (
15). However, this avoidance only reinforces fear and thwarts adaptive processing of traumatic memories, thus perpetuating PTSD symptoms (
15,
16).
Caring for persons with PTSD, particularly military servicemembers deployed during Operation Enduring Freedom and Operation Iraqi Freedom, has created challenges for existing healthcare systems (
17–
19). These challenges have recently been compounded by the COVID-19 pandemic, including the need to adapt management approaches to mental health symptoms such as fear, anxiety, depression, avoidance, and PTSD to pandemic-related healthcare deliver constraints (
20). Accordingly, there is a need for improved assessments and evidence-based treatments that effectively reduce PTSD-associated psychological distress and functional disability.
PSYCHOTHERAPY INTERVENTIONS FOR PTSD
Exposure therapy is an effective treatment for PTSD (
16). Exposure therapy decreases PTSD symptoms through imaginal exposure (i.e., vividly imaging the feared object, situation, or activity) aimed at helping individuals overcome, rather than avoid, fear- and psychological distress-inducing stimuli (
21,
22). In principle, imaginal exposure potentiates inhibitory learning processes and decreases the distress associated with traumatic memories by facilitating the development of adaptive associations with them, thereby rendering those memories harmless and tolerable (
15).
Among other psychological treatments for PTSD are trauma-focused cognitive-behavioral therapy (TF-CBT) interventions. These therapeutic approaches selectively target the memories, feelings, and thoughts of the traumatic events. Prolonged exposure (PE) and Cognitive Processing Therapy (CPT) are well recognized interventions among the TF-CBT treatments for PTSD (
22–
24). PE is a specific form of TF-CBT that focuses on teaching patients to cope with their trauma-related memories, feelings, and situations by approaching them slowly but progressively (
16). A recent study assessed exposure therapy sessions in 61 combat veterans of Iraq/Afghanistan and concluded that the PE group results demonstrated the most significant reductions in PTSD symptoms, as compared with cognitive processing therapy. That said, some patients either continue experiencing severe PTSD symptoms after receiving these treatments course or do not respond adequately to them (
25). Thus, new therapies employing improved and advanced methodologies are needed.
EXTENDED REALITY (XR) FOR EXPOSURE THERAPIES
The advent of the XR platform (e.g., virtual reality [VR], augmented reality, and mixed reality) provides an alternative approach to traditional psychological interventions for the delivery and study of treatments for a wide range of mental health conditions, including PTSD (
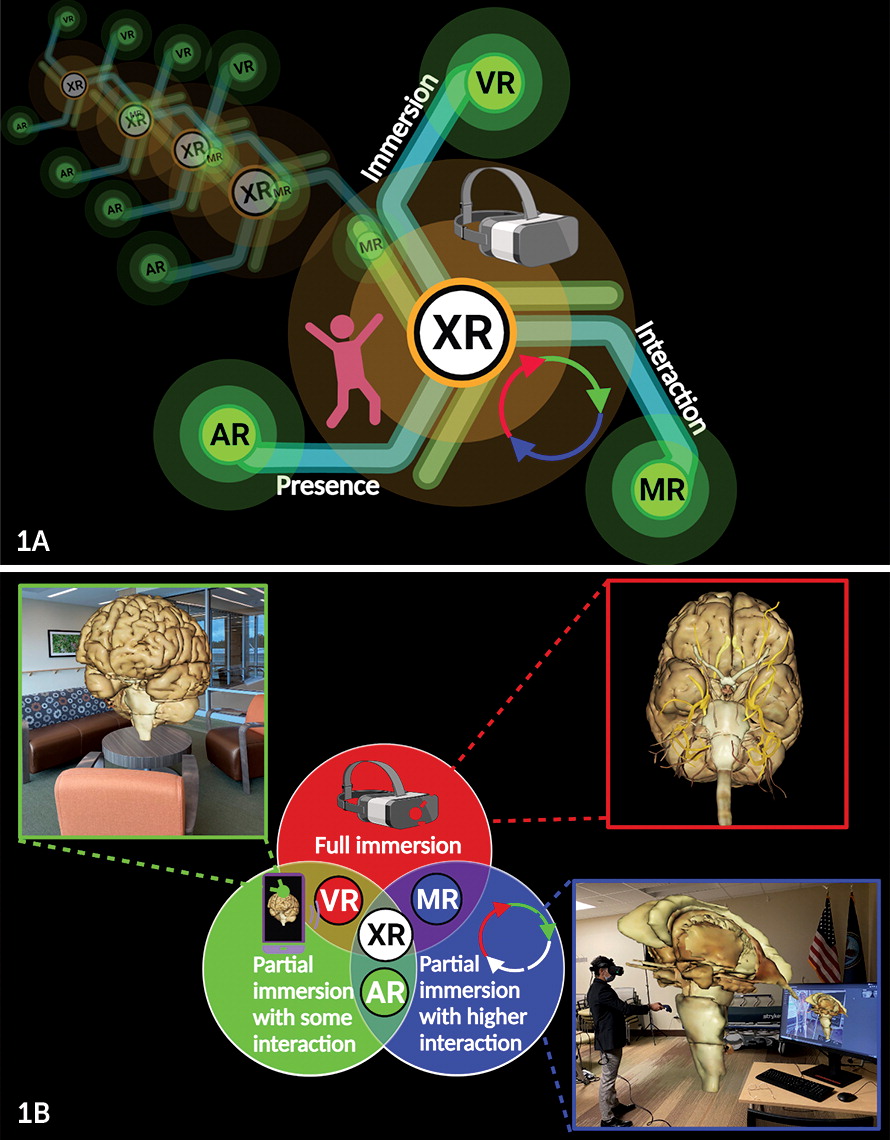
26). Extended reality is an emerging imaging paradigm in which users can experience varying levels of immersion, interaction and presence within the digital world (
Figure 1A) (
1,
27). It provides an innovative method for delivering exposure therapies (
26).
During a VR session, the user experiences a full immersion into a digital environment, the experience of which is facilitated by a head-mounted display (HMD) that provides sensory input (i.e., images, sound) (
3). In augmented reality, the user is partially immersed into an artificial environment but can interact with the real world, as well as with virtual elements in the digital world concurrently (
4). Mixed reality poses as a subclass of VR, combining real and virtual milieus along a “virtuality continuum,” seamlessly integrating real-world and artificial digital scenes with a superior level of connectivity and higher computer-user interactions (
Figure 1B) (
3,
5).
Several studies have demonstrated that VR exposure (VRE) therapy is different from a standard VR experience (i.e., amusement). VRE is a systematic psychotherapeutic immersion paradigm that uses multisensory VR to increase the patient’s experiential engagement during treatment sessions. It is an effective intervention for PTSD symptoms across varied populations, including combat soldiers after military trauma (
12,
26,
28–
31). Virtual reality systems evoking multisensorial (auditory, visual, tactile, etc.) neural stimulation may hold the key for increasing the activation of trauma memory during exposure therapy (
26,
32). Trauma-associated sensory elements such as image renderings, sounds, and even odor cues could suppress avoidance, assisting PTSD sufferers conquer their suppressed emotions and fear (
15).
VRE trauma-relevant elements can mitigate avoidance by increasing emotional and sensory engagement (due to multisensorial activation), while reducing the probability of undesirable neural activation (
33,
34). The periodic therapeutic activation of the trauma memory facilitates the conversion of new information to be encoded, while decreasing memory-associated anxiety and fear processes (
35). Immersive XR paradigms can help individuals feel more comfortable facing stressful scenarios “virtually” rather than in real life, thereby learning new behaviors transferable to real world challenges (
36). Another advantage is the added treatment-controlled conditions, where therapists can regulate the immersive experience during VRE therapy sessions (i.e., by adjusting intensity of exposure) (
2).
In 2011, Reger et al. (
28) reported results from a pilot study on the effectiveness of VRE treating PTSD in active-duty soldiers. Soldiers treated with VRE immersion therapies reported a statistically significant decrease in PTSD symptoms. The role of VRE in increasing emotional engagement and reducing avoidance was demonstrated in an elegant study by Costanzo et al. (
37). The results from this investigation indicated that experiencing a standardized combat-related VR immersion heightened arousal in recently returning combat-exposed service members with PTSD compared with combat-exposed service members without PTSD. More recently, a study by Katz et al. (
38) indicated that VRE engagement is linked to higher physiological habituation to trauma-relevant stimuli, compared with habituation in the standard PE condition. Taken together, these findings add to the growing body of evidence validating the concept of VRE therapies as interventional methodologies with potentially higher engagement attributes compared with traditional exposure therapies (
34). The exact neurophysiological mechanisms by which VRE mitigates avoidance in PTSD are not clearly understood. However, an interesting concept to consider is whether lowering the symptom of avoidance using virtual immersion could be a predictor for reduction in reexperiencing symptoms. Engaging in VRE experiences may potentiate further emotional processing, thus hampering (or lowering) the reexperiencing of and the reactivity to trauma-related memories (
34).
MULTISENSORIAL ELEMENTS OF XR
XR technologies, including VR represent a versatile and innovative cybernetic platform with significant applicability to the clinical neurosciences. Concurrent with these medical and technological advances, clinical VR, a category of virtual interventions fosters innovative mental health procedures and new therapeutic interventions applicable at varied clinical fields including discipline-specific (i.e., medicine, psychology), and expanding to interdisciplinary, multidisciplinary, and transdisciplinary levels (
39–
49). XR treatments provide higher levels of immersion, interaction, and presence. While all of these are important elements of this treatment approach, increased immersion (i.e., profound cognitive involvement in which a user is isolated from the real world) and presence (i.e., evoking the illusion of being present) have been linked to efficacy of VRE, including both improved clinical outcomes and also sustained effects over time (
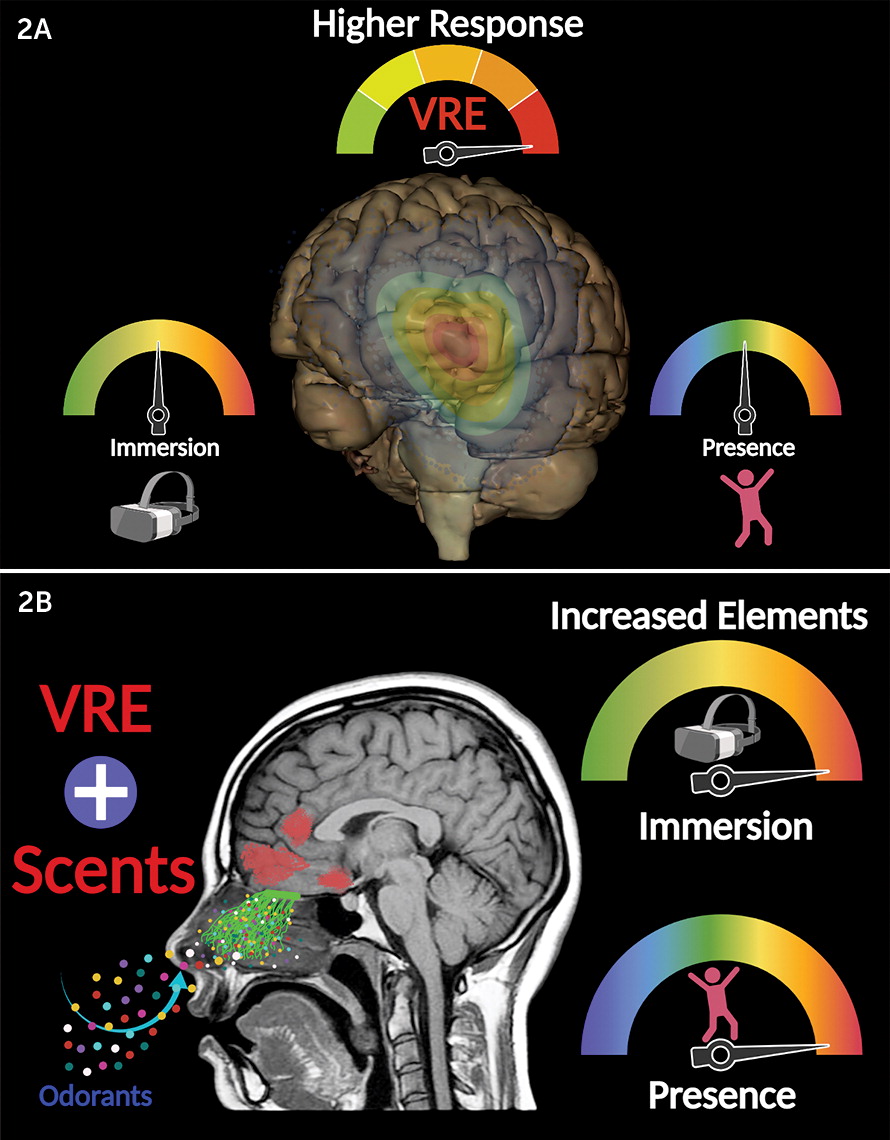
Figure 2A) (
2).
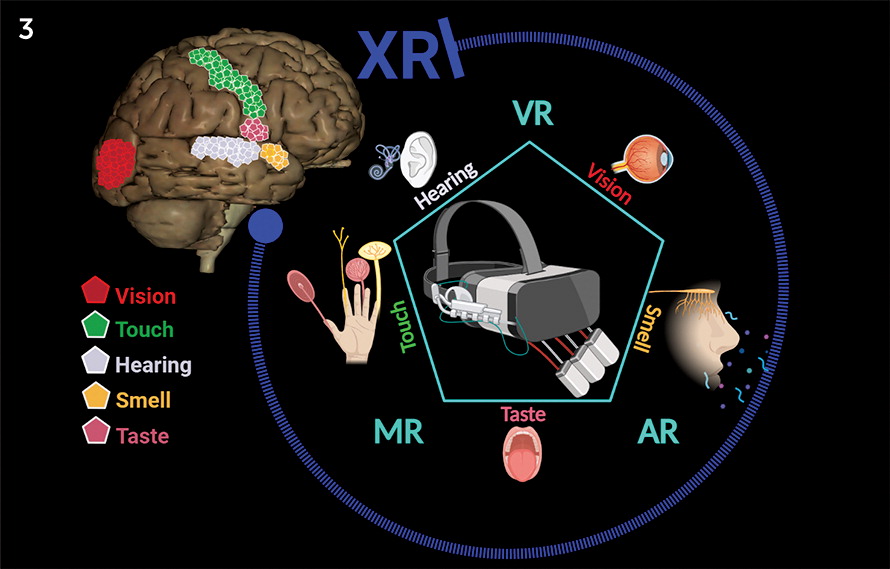
Human interactions in the real-world environment are naturally multisensorial (i.e., stimulating the senses of touch, sight, hearing, smell and taste simultaneously) (
11). Generating a multisensorial virtual paradigm is an essential requisite in the rendering of an immersive replica of the real world (
6). To date, most VR experiences (i.e., entertainment, tourism, marketing) primarily stimulate the audiovisual centers (
6,
11,
50). In the clinical domain, VRE treatment has predominantly focused on the visual and auditory senses (
6). However, some authors have argued the need for olfactory integration into VRE for the treatment of PTSD (
6,
7,
51). The mediation of olfactory memories is processed within the orbitofrontal cortex, medial prefrontal cortex, amygdala and hippocampus (
8). These neuroanatomical structures are also implicated in learning and memory and constitute a foundational circuitry for PTSD (
7).
The amygdala performs a pivotal function in sensory integration of olfactory stimuli (i.e., odor-induced fear) (
7,
52). Coupling of a neutral (i.e., conditioned) stimulus to a fear-evoking (i.e., unconditioned) stimulus, inducing fear responses to the conditioned stimulus by itself, has served in probing the amygdala’s role in odor-induced fear behaviors (
52). In addition, other limbic structures such as the bed nucleus of the stria terminalis have been implicated in odor-evoked fear (
53). A recent randomized controlled trial demonstrated that VRE incorporating trauma-related odors, such as flammable gas (e.g., diesel), added to the mainstream visual and auditory stimuli, was effective in reducing PTSD symptoms in active duty military personnel (
54).
In humans, the physiologic mechanisms involved in aromatic processing is commonly emotional and visceral. Odor-evoked memories are more emotionally robust than memories triggered by other sensory stimuli (i.e., visual, auditory) (
55–
57). More importantly, the neurophysiological processing of odors in the brain is linked to PTSD neural pathways (amygdaloid-hippocampal complex and orbitofrontal cortex), the same neuroanatomical circuits regulating emotions, emotionally-evoked memories and related associations (
6–
9). An interesting study conducted by Munyan et al. (
10) indicated that odor-evoking VRE environments further increase the elements of immersion and presence, offering a higher real-world-like experience than VRE without scents (
Figure 2B). The advances in technology and the innovation of today’s HMDs support the capabilities to stimulate all five senses (
Figure 3) (
11). Olfactory stimulation can be achieved with “olfactory HMDs” that release a variety of scents or odorant combinations (
58,
59). An exemplary VRE study on combat-related PTSD (Iraq), utilized universal serial box (USB) olfactory display add-on gear capable of releasing eight different scents associated with the Iraq War. Odorants were disseminated to the participants using fans and a small air compressor. Positive outcomes were reported, including significant reduction of PTSD symptoms (
47).
GENERAL CONSIDERATIONS AND ACCESSIBILITY
Unequivocally, XR innovations have advanced significantly during the last decades, with improved add-on technologies, more affordable devices, and further realistic software. These improvements are making it possible for XR systems and their components (HMDs, controllers, eye-tracking devices, etc.) to reach a wide-range of multidisciplinary users, including healthcare providers and patients (
1). From a clinical and research standpoint, immersive virtual environments can be highly controllable spaces that facilitate research studies and clinical interventions, considering that almost every element of the virtual milieu can be regulated (
18). Furthermore, artificial virtual environments are particularly nimble, allowing the necessary adjustments following the adaptation processes as determined by the user’s specific cognitive, emotional and neurophysiological nuances (
60).
Nonetheless, XR technologies still have some drawbacks that pose important clinical restrictions that arise when considering the costs of the devices, such as hardware and software. Another limitation is the need for specialized technology skills and medical training to create and deliver clinically safe immersive experiences and to operate the XR system components (i.e., software, HMD, hand-controllers), as well as the potential side effects, such as cybersickness (
48,
61). XR-based therapeutic approaches should not be envisioned to become automated interventions for self-administration. On contrary, they require well trained clinicians to assure the appropriate care is provided, considering their intricacy and potential impact on behavioral health conditions (
18). XR hardware designs have additional limitations (i.e., most HMD lenses are either bulky and heavy, wired-tethered to computer systems, or have limited battery endurance) (
62). However, XR technology is rapidly advancing: performance of devices is exponentially improving, thus providing seamless immersions, improved human-machine integration, and more highly adaptive interactions (
63). In addition, the cost of HMDs and other XR devices is constantly decreasing as the popular demand and medical usage increase (
64).
In addition, the U.S. Food and Drug Administration Center for Devices and Radiological Health is engaging in medical XR regulatory science research. The medical XR program is one of 20 research lineups established to warrant patient access to innovative XR-based devices that are effective and safe. This program is intended to reduce the gap between XR technologies (e.g., design, development, evaluation) and their clinical integration. Government and other agencies are fostering a scientific culture in support of regulatory requirements and decisions on the technologies governing medical XR devices (
64).
CONCLUSIONS
PTSD is a highly distressing disorder characterized by extremely upsetting thoughts and intrusive traumatic memories. Experimentally, VRE immersion has proven to be effective as a therapeutic intervention by reducing the symptoms of PTSD across varied populations, including veterans. The therapeutic attributes of XR innovation rely on its immersive potential, capable of recreating real-world experiences at a digital multisensorial level, and integrating a seamless human-computer interface. Although XR technology is hastily advancing, it is not yet mainstream. Therefore, it is imperative to continue the technological advances, accompanied with XR system cost reductions to support the accessibility of these systems, and target a wider range of neuropsychiatric disorders.
The emotional distress among the returning troops from Iraq and Afghanistan, along with the PTSD resulting from living through the COVID-19 pandemic, is anticipated to generate additional mental health challenges in the coming years. To address these imminent needs, clinical VR technology research advances and VRE therapies may be considered suitable medical interventions.