A comprehensive report on the role of psychiatry in health system reform, delivered last month to the APA Board of Trustees, emphasized the importance of emerging models of integrated or collaborative care.
The extensive report—the executive summary alone is 38 pages—is the work of a special ad hoc work group on the role of psychiatry in health care, chaired by incoming APA President-elect Paul Summergrad, M.D. The report covers issues related to the rollout of the Affordable Care Act (ACA), but emphasizes that health care reform is broader than the ACA and includes multiple state, federal, and private patient-care delivery and payment initiatives.
Common themes going forward in both the public and private sectors, according to the report, are these:
•
Regardless of the adoption of particular clinical or reform models, the financial pressures for control of health care costs by federal, state, and employer payers will continue.
•
New models of care delivery (with varying degrees of evidence to support them) are under development and/or being deployed.
•
The triple aim of population health, measurement of quality and performance, and reduced cost of care will drive clinical system development.
•
How care is measured and monitored (quality and performance measures) will be increasingly codified.
•
Alternative payment methodologies will be developed and deployed.
•
Patient-centered principles of care including medical homes will become common.
Of particular importance to psychiatrists, other physicians, and policymakers is that there is considerable evidence that patients with psychiatric and substance use disorders suffer from high rates of medical comorbidity and markedly increased costs for their total medical care.
Population Health a Focus
So what might individual psychiatrists do to prepare?
“We should become familiar with these new models of integrated or collaborative care,” Summergrad told Psychiatric News. “We were asked by the Board to inventory developing models in the general-medical and public-sector settings and the evidence for their efficacy, which is what we focused on in our report.”
The forces converging around “integrated” or “collaborative” care are many including, most prominently, the pressure of budget deficits and increasing costs of care. More specifically, policymakers and some psychiatric pioneers in integrated care have focused on the high medical costs associated with general medical patients having comorbid psychiatric and substance use conditions.
But the movement toward integrated care is also driven by more global trends in care redesign, especially a focus on population health, measurement of outcomes, use of electronic records, and the “triple aim” in improving overall quality. The latter is a framework developed by the Institute for Healthcare Improvement for optimizing health system performance by simultaneously pursuing three goals or “aims”: improving the patient experience of care (including quality and satisfaction), improving the health of populations, and reducing the per capita cost of health care.
Integrated care was the theme of past APA President John Oldham, M.D.’s presidential year (2011-2012). Psychiatrist Jeremy Lazarus, M.D., who is president of the AMA, made integrated care a centerpiece of his presidential address last year (Psychiatric News, December 7, 2012).
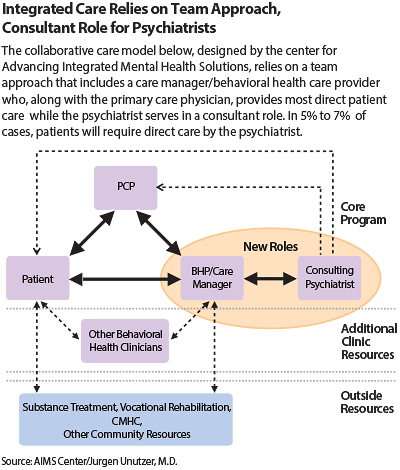
Psychiatric News has published numerous articles describing the growing consensus around integrated care. At APA’s 2012 Institute on Psychiatric Services in New York, Jurgen Unützer, M.D., of the AIM center at the University of Washington described innovative models of care that integrate psychiatric and general medical services and presented evidence that psychiatrists working in a consultative way with primary care can significantly improve mental health care for large populations of people in primary care, while also lowering overall health care costs.
For instance, one of the largest randomized, controlled trials of this model is the IMPACT study conducted by Unützer and colleagues at the University of Washington from 1998 to 2003. In the original IMPACT study and numerous replications, patients receiving collaborative care were found to have less depression, less physical pain, better functioning, and a higher quality of life.
There was also greater patient and provider satisfaction. Importantly, from a public-policy standpoint, IMPACT has lowered costs substantially for patients receiving the intervention through more efficient mental health treatment and lower use of inpatient care, pharmacy, and other outpatient services associated with comorbid medical conditions (Psychiatric News, November 2, 2012).
Unutzer’s work focused on the role of psychiatrists in overseeing depression care in primary care settings. The ad hoc Board work group found that additional research and study are needed in the care of individuals with psychiatric and substance use disorders in primary care settings and on integration of primary care physicians into public-sector mental health settings.
Systems Are Evolving
The report by the work group outlined a great number of recommendations regarding integrated care, including the following:
•
APA should support the value of integrated general medical and psychiatric care for patients with psychiatric illness in all treatment settings. This support should be based on best evidence regarding optimal care for all patients and care that is patient-centered and consistent with goals of the “Triple Aim.”
•
Particular attention should be paid to the distinct needs of patients of varying ages and in different care settings and, in particular, in the public sector.
•
APA will need a comprehensive inventory of changes across the country and a rapid response capacity to assist in federal and state advocacy and support its membership.
•
APA needs to produce a clear, simple set of statements for psychiatrists and their patients regarding integrated care; define the role of psychiatrists as team leaders and consultants; state how their role in integrated care will benefit patients; and clarify psychiatry’s role vis-à-vis other physicians, allied health practitioners, and other mental health clinicians.
The report emphasizes that psychiatrists, because of their medical expertise and extensive training with seriously ill psychiatric and medical patients, have distinctive expertise to integrate this care, working closely with primary care, specialty physicians, and nonphysician mental health clinicians. This expertise, the report notes, is borne out by the research evidence.
In an interview with Psychiatric News, Summergrad emphasized that while the general movement in health systems is toward greater collaboration between specialty care and primary care, the sheer scope of health system change makes it difficult to know exactly how systems will evolve in different regions of the country.
Also, there are many other unknowns that will require ongoing vigilance by APA and its district branches. “What is especially unclear is how care will be paid for in the future. Will it be through large integrated systems? Will fee-for-service reimbursement for specialists be replaced by global or bundled payment models? We recommended integrated financing models to allow the full and equitable reimbursement for our patients and for psychiatric physicians. Regardless of which models are adopted, the current efforts to secure parity need to continue,” he said. “I want to emphasize that we don’t presume to think traditional forms of psychiatric practice will all change—let alone disappear—but it is clear that in many settings closer integration between general medical care and psychiatry in primary care or in specialty mental health settings will be very important.” ■
APA has established a Work Group on Integrated Care, chaired by Lori Raney, M.D., medical director of the Axis Healthcare System in Durango, Colo. The Integrated Care Track at this year’s annual meeting will feature lectures, symposia, workshops, and other presentations. The schedule is posted at
http://psychnews.psychiatryonline.org/newsArticle.aspx?articleid=1653553. APA is also sponsoring an all-day program, “Clinical Updates in Primary Care Psychiatry: For Primary Care and Mental Health Providers,” on Friday, May 17, from 7:45 a.m. to 5 p.m., in the Moscone Convention Center. The registration fee is $299. More information is available by calling (888) 357-7924.