Brain Abnormalities Found in Patients With Chronic Fatigue
Using a series of sophisticated imaging techniques, researchers at Stanford University found distinct differences in the brain structure of people with chronic fatigue syndrome (CFS) compared with healthy subjects.
This work, published in Radiology, may make it easier to diagnose this still mysterious condition by revealing some of its underlying neurological processes.
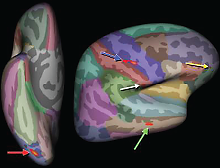
Michael Zeineh, M.D., Ph.D., and colleagues imaged 15 people with CFS and 14 matched healthy controls and found three intriguing disparities. First, MRI images revealed an overall reduction of white matter in CFS brains, suggestive of elevated inflammation and not entirely unexpected.
An advanced technique known as diffusion-tensor imaging then revealed two more unexpected abnormalities in a nerve tract called the right arcuate fasciculus. This nerve segment connects the brain’s frontal lobe and temporal lobe, and in CFS patients both the tract and the gray matter in the connected lobes was thicker than normal.
At the moment, the function of the right arcuate fasciculus is not well understood, though its counterpart on the left side of the brain connects two brain regions critical for language.
Zeineh M, Kang J, Atlas S, et al. Right arcuate fasciculus abnormality in chronic fatigue syndrome.
Radiology. Oct 29, 2014 [Epub ahead of print]
Brain Region Appears Smaller In Teens With History of Early Childhood Depression
A study published in JAMA Psychiatry shows that a key region of the brain involved in emotion may be smaller in size in youth who were diagnosed with depression as preschoolers, compared with their peers who were not diagnosed with depression.
Joan Luby, M.D., director of the Early Development Program at Washington University School of Medicine in St. Louis, and colleagues conducted a study in which approximately 130 youth with and without a previous diagnosis of major depressive disorder (MDD) were followed from preschool-aged years to adolescence to assess the psychiatric and long-term neuroanatomical consequences of the onset of MDD in early childhood.
The results showed that more than 55 percent of those with early childhood MDD displayed pathological guilt during their preschool years, compared with 20 percent in the nondepressed group. Using magnetic resonance imaging, the researchers found that the right anterior insula—involved in emotion and self-perception—was smaller in adolescents with a history of MDD and guilt during early childhood, compared with that of their counterparts without such medical history. The data also showed that adolescents with smaller insula were more prone to experiencing recurrent episodes of clinical depression as they aged.
The researchers noted that “excessive guilt and depression may put preschoolers on a developmental trajectory that contributes to problems with depression later in childhood and even throughout life.”
They concluded that the findings concerning this brain region “are consistent with mounting research in adult MDD, suggesting that insula function and structure may be a target biomarker for major depression.”
Belden A, Barch D, Oakberg T, et al. Anterior insula volume and guilt neurobehavioral markers of recurrence after early childhood major depressive disorder.
JAMA Psychiatry. November 12, 2014. [Epub ahead of print]
Areas With High Volumes of Tobacco Shops Have Local Teens Who Smoke More
Researchers from the universities of Edinburgh and Glasgow mapped tobacco retailers for every postal code in Scotland to examine how the number of tobacco-selling outlets in an area impacts local teenage smoking rates. More than 20,000 youth aged 13 to 15 were surveyed on their smoking behavior.
The results showed that teens living in neighborhoods with the most tobacco retailers were almost 50 percent more likely to take up smoking than those with no tobacco retailers nearby—regardless of socioeconomic status. In addition, youth living in areas with the highest density of retailers were 53 percent more likely to try smoking at least once.
The researchers noted that antismoking strategies among teenagers should include reducing the overall density of tobacco retailers. They concluded that limiting teenagers’ access to tobacco products is vital, “as long-term smoking usually begins in adolescence.”
Shortt N, Tisch C, Pearce J, et al. The density of tobacco retailers in home and school environments and relationship with adolescent smoking behaviours in Scotland. Tob Control. November 4, 2014. [Epub ahead of print]
Link Found Between Air Pollution, ADHD Symptoms in Children
Breathing air concentrated with polycyclic aromatic hydrocarbons (PAH)—a component of air pollution—during pregnancy may increase risk for attention deficit/hyperactivity disorder (ADHD)–related symptoms in offspring, researchers from the Mailman School of Public Health at Columbia University report.
The researchers followed 233 nonsmoking women who were pregnant while living in New York City, as well as their offspring from newborn to childhood to investigate if a link existed between maternal PAH exposure and ADHD in offspring. PAH exposure in mothers was measured from blood obtained at delivery.
Results showed that children who were born to mothers exposed to high levels of PAH during pregnancy were five times more likely to display a “higher-than-usual” number of symptoms that characterize ADHD by age 9, compared with children whose mothers did not have high PAH exposures.
Though the mechanism by which maternal PAH exposure during pregnancy increases the likelihood of ADHD-like symptoms in offspring is not fully understood, the researchers noted several possibilities, including DNA damage and interference with placental growth factors resulting in decreased exchange of oxygen and nutrients. The researchers stressed the need for more research to fully understand this relationship.
Perera F, Chang H, Tang D, et al. Early-life exposure to polycyclic aromatic hydrocarbons and ADHD behavior problems.
PLoS One. 2014; 9(11):e111670.
Extended Use of Combined Anticlotting/Antiplatelet Drugs May Raise Dementia Risk
Researchers from the Intermountain Medical Center in Utah examined more than 1,000 people with no history of stroke or dementia for up to 10 years to assess the risk for dementia associated with overtreatment of therapies that combine warfarin (an anticlotting drug) and antiplatelet medicines (such as aspirin) intended to prevent stroke.
The results, which were presented at last month’s American Heart Association Scientific Sessions in Chicago, showed that patients who were overtreated with the drug combo—indicated by abnormally slow blood clotting rates during routine testing—for more than 25 percent of the study’s duration were twice as likely to be diagnosed with dementia than patients who were overtreated less than 10 percent of time. The increase was higher than what researchers found in a previous study with warfarin alone.
“We have to consider that long-term exposure to anticlotting drugs such as warfarin, if not well controlled, can significantly increase bleeding risk,” said T. Jared Bunch, M.D., lead author of the study and director of electrophysiology at Intermountain. “This may result in micro bleeds in the brain that don’t cause symptoms right away, but accumulate over time, raising the risk of dementia.”
Bunch recommended that patients who are concerned that they are being overtreated with anticlotting drugs such as warfarin consult with their physicians about newer options of anticlotting agents that may better regulate clotting rates.
Thomas J Bunch T, May H, Bair T, et al. Percent time with a supratherapeutic Inr in atrial fibrillation patients using an antiplatelet agent is associated with long-term risk of dementia.
Circulation. 2014; 130: A13426.
Association Found Between Antipsychotic Efficacy and Schizophrenia Severity
Though antipsychotic medications have played a major role in the history of treatment for schizophrenia, not much is known about their effectiveness across a wide range of baseline symptom severities for the disorder. A study published in JAMA Psychiatry attempts to shed some light on the situation.
Researchers from Japan’s Kyoto University Graduate School of Medicine collected data on 611 individuals with acute schizophrenia and 475 individuals with predominantly negative symptoms of schizophrenia to examine the influence of baseline severity of schizophrenia on the efficacy of antipsychotic drugs. Studied antipsychotics included olanzapine, risperidone, and amisulpride, which were all compared with placebo. Reduction in symptoms was measured by the Positive and Negative Syndrome Scale (PANSS) and Scale for the Assessment of Negative Symptoms (SANS).
The analysis showed that the greater the severity at baseline, the greater the difference in scores on symptom scales between active and placebo after six weeks of treatment. In the acute schizophrenia cohort, the mean differences in scores between active and placebo on the PANSS were 9.5 points for patients who were mildly ill at baseline, 13.7 for moderately ill patients, and 24 for severely ill patients. In the treatment of those with predominantly negative symptoms, the mean differences on the SANS were 1.7 for moderately ill patients and 9.7 for severely ill patients.
“Toward the mildest end of the spectrum [for schizophrenia],” the researchers noted, “clinicians need to be aware that patients benefit less in terms of symptom improvement but may experience full adverse effects of antipsychotics. Clinicians also need to be aware that in addition to the treatment of active symptoms, which was the focus of this study, antipsychotics have another important action, namely to prevent relapses among patients in remission.”
Furukawa TA, Levine SZ, Tanaka S, et al. Initial severity of schizophrenia and efficacy of antipsychotics: participant-level meta-analysis of 6 placebo-controlled studies.
JAMA Psychiatry. November 5, 2014. [Epub ahead of print]
PTSD, Bipolar Disorder Linked to Delivery of Preterm Babies
A pair of new studies highlights the risk that mental illness can pose during pregnancy, showing that women with bipolar disorder or posttraumatic stress disorder (PTSD) are more likely to deliver preterm babies.
As published in the American Journal of Obstetrics and Gynecology, researchers at Women’s College Hospital and the Institute for Clinical Evaluative Sciences in Toronto compared health records of women who had given birth in Ontario from 2003 to 2011.
Compared with women without a history of mental illness, women with bipolar disorder were twice as likely to have a preterm birth, and they also had greater risks for having babies large for their gestational age or babies with congenital malformations.
A study from Stanford School of Medicine and the U.S. 0Department of Veterans Affairs identified a similar premature birth trend in a study of more than 16,000 births by veterans.
Women with PTSD had a 35 percent increased risk of having a spontaneous preterm birth. However, the risk was limited to women who had a PTSD diagnosis in the year prior to giving birth.
“This makes us hopeful that if you treat a mom who has active PTSD early in her pregnancy, her stress could be reduced, and the risk of giving birth prematurely might go down,” commented study author Ciaran Phibbs, Ph.D.
Elad M, Ray J, Vigod S. Perinatal outcomes among women with bipolar disorder: A population-based cohort study.
Am J Obstet Gyneco. Oct 14, 2014 [Epub ahead of print]. Shaw J, Asch St, Kimerling R, et al. Posttraumatic stress disorder and risk of spontaneous preterm birth.
Obstetrics & Gynecology.
Rare Genetic Condition May Protect Against Bipolar Disorder
A rare genetic dwarfism known as Ellis van-Creveld (EvC) syndrome appears to offer protection against bipolar disorder, much as sickle cell disease confers resistance to malaria.
This genetic connection resulted from more than 40 years of research in Old Order Amish families. Janice England, Ph.D., of the University of Miami Miller School of Medicine had been tracking a set of related families in which both EvC and bipolar disorder were prevalent, yet over several generations the two disorders never manifested together.
Statistical analysis confirmed the protective effect of the EvC gene, which is also located on chromosome 4, adjacent to a region previously associated with bipolar protection.
The function of the EvC gene isn’t yet known, but when mutated, it disrupts the activity of the sonic hedgehog (Shh) protein, thus offering a tangible target for further research.
Co-author Edward Ginns, M.D., Ph.D., of the University of Massachusetts Medical School cautioned that this discovery still leaves lots of questions. “The sonic hedgehog pathway involves more than a dozen other molecules and interacts with over 100 genes,” he said.
He noted that many drugs targeting the Shh pathway are in clinical trials for other conditions, so there may be some new options for affective disorders like bipolar disorder down the road.
The study was published online in Nature Molecular Psychiatry.
Ginns E, Galdzicka M, Elston R, et al. Disruption of sonic hedgehog signaling in Ellis-van Creveld dwarfism confers protection against bipolar affective disorder.
Mol Psychiatry. Oct 14, 2014 [Epub ahead of print]
Smoking Interferes With Cognitive Recovery During Alcohol Abstinence
A study involving 133 alcohol-dependent people undergoing treatment found that smoking interferes with neurocognitive recovery during their alcohol abstinence.
After eight months of alcohol abstinence, the 75 subjects who were active smokers showed poorer recovery than the 30 who never smoked on multiple measures of learning, memory, and processing speed. The 28 subjects who were former smokers fared a little better, but still performed worse on several tests. Alcohol-dependent people who had never smoked were not significantly different from 39 healthy control subjects on any measure, however.
The assessment of neurocognitive recovery also found that as a group, alcohol-dependent people in recovery showed the greatest improvements during the first month of abstinence, suggesting this might be a key time to stop smoking, if possible.
“Cigarette smoke contains a tremendous number of toxic compounds that affect multiple organs in the body, including the brain,” said lead study author Timothy Durazzo, Ph.D., of the University of California, San Francisco. He suggested that components of cigarette smoke that promote oxidative stress might be critical factors, as the brain is vulnerable to the free radicals produced by oxidative stress.
This study was published online in Alcoholism: Clinical and Experimental Research. ■
Durazzo T, Pennington D, Schmidt T, Meyerhoff D. Effects of cigarette smoking history on neurocognitive recovery over 8 months of abstinence in alcohol-dependent individuals.
Alcohol Clin Exp Res. Oct 21, 2014 [Epub ahead of print]