Maybe it is a clichȳ to say that someone who has gone off to war will return home “changed,” but it should not be a surprise.
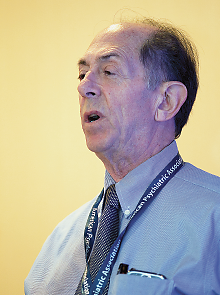
The adjustment back to life in the United States may be smoother for some and more difficult for others, like the soldiers that psychiatrist Marvin Oleshansky, M.D., sees at the U.S. Army’s Tripler Medical Center in Honolulu.
“I call that change ‘postdeployment stress disorder,’ ” he said. “They have sleep problems, road rage, family issues, drink a lot, and it’s not unusual for things to escalate to a dangerous level.”
The sanctioned form of violence that soldiers experience in training and combat can form the backdrop for violence on returning home, whether in the form of homicide, suicide, domestic violence, or sexual violence, said Oleshansky, who retired as a colonel from military service in 2001 and then worked as a civilian psychiatrist at Tripler until retiring again June 1.
Disturbing as such violence may be, it should not necessarily be equated with posttraumatic stress disorder (PTSD), Oleshansky emphasized in a presentation at APA’s annual meeting in New York in May.
“A lot of soldiers are surprised that they don’t have symptoms right away, so they don’t think they have PTSD,” he said. “Symptoms may be acute or they may be delayed or chronic or intermittent. Often there are periods of higher functioning, and then something leads to a relapse.”
Grief and mourning are often overlooked as keys to diagnosis and treatment. Loss of one’s friends and the resultant grief may be inevitable in war, but onset of PTSD symptoms may be delayed until something else triggers memories of previous losses, he pointed out. “Soldiers don’t understand why it starts later and not right away.”
Acute grief, especially if it is not mourned, can persist as complicated grief, a chronically debilitating condition, Oleshansky said. Then the stress of grief can precipitate the onset or exacerbation of existing emotional or physical problems, including those unmourned losses.
Noting that guilt is closely associated with grief, Oleshansky said that he tries to help his patients overcome the “hindsight bias” that torments them over what they might have done to prevent the deaths of others. To help correct irrational beliefs, he asks soldiers what they would have done differently had they known in advance what the outcomes of their actions would be.
“This is a critical approach in treating grief,” he said. “It sounds simplistic, but it’s surprisingly effective.”
Red flags in these discussions with soldiers crop up from many directions. Among these are older age at entry into military service, a high tempo of operations, financial and partner-related problems, and exposure to combat and random violence—all of these can increase the risk of character pathology.
“I can’t think of a soldier I’ve treated who wasn’t near a mortar explosion,” Oleshansky said. “And the fact that someone else died in the same explosion is a huge factor.”
To effectively treat soldiers who have experienced combat, a therapist needs to understand the soldier’s background and how various aspects of that history have contributed to his or her experiences.
“But it is hard to figure out when to ask: ‘What did you do? Did you shoot and kill people, including children?’ ” said Oleshansky. “If you ask too soon, they’ll think you’re callous, and if you’re a civilian, they’ll decide that you don’t know what you’re talking about. This is the hardest part of a clinical interview.”
In addition, he noted, alcohol use is a constant concern because it is socially sanctioned in the short term for symptom relief of anger or sleep problems, although it only perpetuates the soldier’s symptoms.
Any unresolved adverse childhood experiences may also be recalled by the stressors of the military experience and contribute to the distress that brings soldiers to treatment, he added. “If there’s one predictive factor, that would be it.”
Persistence is essential. “It’s not uncommon that you have to redo the therapeutic process,” he pointed out. “These individuals have very strong defenses, and they will find a way to undo what you accomplish in one session, but you stay with it.” ■