Reform of the nation’s mental health system is an urgent priority, and legislation pending in Congress would do much to help make reform a reality, maintain psychiatrists Lloyd Sederer, M.D., and Steven Sharfstein, M.D., in an editorial published online August 14 in JAMA Psychiatry.
“Legislative action is needed to support improvements in a mental health system widely regarded as flawed,” Sederer and Sharfstein wrote. “A bipartisan bill that increases voluntary and, when necessary, involuntary access to a variety of mental health services, values the judgments of clinicians and families, sensibly extends information heretofore limited by HIPAA (Health Insurance Portability and Accountability Act), and promotes public education about what to do when faced with acute mental illness could be a vital contribution to improving lives and reducing the far-too-common risk of violence by people with serious mental illness, to themselves and others, that aggrieves and frightens families and communities across the United States.”
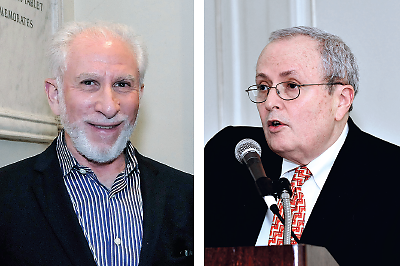
The editorial has received widespread attention. Sederer is medical director of the New York State Office of Mental Health and was director of APA’s Division of Clinical Services from 2000 to 2002. Sharfstein, who is CEO and medical director of the Sheppard Pratt Health System, was president of APA from 2005 to 2006.
The authors emphasized that there are two bills in Congress that would be aimed for the first time in 50 years at improving the U.S. mental health care system. They are the Helping Families in Mental Health Crisis Act (HR 3717), a bipartisan bill introduced by Rep. Timothy Murphy (R-Pa.); and the Strengthening Mental Health in Our Communities Act of 2014 (HR 4574), introduced by Rep. Ron Barber (D-Ariz.).
“There are substantial differences between these bills,” they noted. “Aspects of the Murphy bill have met with considerable opposition from some advocates (for its support of involuntary outpatient treatment and its proposal to change the federal agencies responsible for mental health). The Barber bill has been criticized for proposing too little. Efforts to find common ground between these two bills are under way.”
In an interview with Psychiatric News, Sharfstein said he believes the Murphy bill is the superior one. “In my view it tackles head-on some of the major impediments to access to care for a critical subset of individuals who are high cost and very difficult to retain in treatment, in large part because they don’t recognize they are sick,” he said. “We have gone too far in the direction of protecting civil liberties. The emphasis on outpatient commitment in the Murphy bill helps address that.”
Sharfstein said the Barber bill would put more money into the system but won’t fix other structural and systemic problems. “We have to have the right structure for the delivery of care,” he said. “Some of the neediest people who would have been institutionalized are now in the criminal justice system. This is an absolute disgrace. We need to provide incentives for people to be treated in the community and to avoid jail and prison.”
In their editorial, Sederer and Sharfstein said an essential first step in mental health system reform is to focus attention and resources on high-need, high-cost patients and retain them in treatment. “For some patients, safe and affordable housing will be a necessary first step toward recovery and accessibility to care,” they said. “It is important to make high-need, high-cost patients welcome in care and to engage and retain them in treatment so their conditions and lives come under control for their sake, for those who love them, and for the society that supports them.”
They also stated that diversion and alternatives to incarceration for people with mental illness, including addictions, should become overarching public-health goals of a new, responsive mental health system. “Jails are no place for people with serious illnesses of any kind, yet they have become the largest institution for people with mental disorders in this country,” they wrote.
The authors noted that Dade County, Fla., has been effective in diverting individuals with mental illness from jails and hospitals, using a partnership among police, the courts, and crisis services (Psychiatric News, November 19, 2010).
“Federal and state governments should prioritize the move of patients from the criminal justice system to the treatment system by focusing on available data that can show change, setting targets for improvement, and creating financial and regulatory incentives,” Sederer and Sharfstein urged. “Reducing the volume of people with serious mental illness in jails and prisons and increasing their numbers on the rolls of outpatient-oriented accountable care organizations or health homes (behavioral or primary care) are the best and most convincing ways to measure success in a reformed mental health care system.
“Continuously measuring outcomes, and continuing ongoing performance improvement built into standard care and service contracts, will suggest progress is being made,” they said. “Reliable measures of symptoms, function, and quality of life for mental and substance use disorders now exist. The scores on these measures change as a patient improves, much the same way that blood glucose and blood pressure levels improve to normal values as treatment becomes effective and a person begins recovery. Many mental health measures are simple, inexpensive checklists, not costly brain images or large panels of blood tests.” ■
“Fixing the Troubled Mental Health System” can be accessed
here.