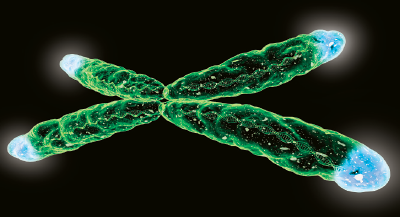
Humans have 46 chromosomes, each capped by genetic material known as telomeres. In addition to providing structural integrity—without them a chromosome would slowly deteriorate each time it replicates—telomeres have emerged as important markers of cell aging that can predict the risk of age-related diseases such as Alzheimer’s disease or diabetes.
A new study from a research group at Stanford University School of Medicine has now found that the length of telomeres may also predict antidepressant response in some people.
This finding, which was published January 5 in Translational Psychiatry, is a continuation of a recent clinical trial that found patients with insulin resistance who took the diabetes medication pioglitazone in addition to antidepressants for 12 weeks showed improvements in glucose metabolism and reported fewer depressive symptoms than those given placebo as an adjunctive therapy.
As part of the trial, 42 patients had their telomeres sequenced. At baseline, telomere length was not associated with the severity or chronicity of depression, but by the end of the study a trend did emerge.
After 12 weeks, those patients with longer telomeres (indicative of more structural integrity) showed greater improvements in their depressive symptoms when given adjunctive pioglitazone compared with patients with shorter telomeres—improvements that occurred regardless of the participant’s baseline metabolic profile, which ranged from insulin sensitive to pre-diabetes. This association was not seen in the patient group that received placebo.
“What is truly exciting about this finding is that the telomeres seem to be connected to the condition of depression and not the condition of diabetes,” said lead study author Natalie Rasgon, M.D., Ph.D., a professor of psychiatry and behavioral sciences at Stanford. (Elizabeth Blackburn, Ph.D., who shared the Nobel Prize for the discovery of telomeres, was also a coauthor on this study.)
“People think of pioglitazone as a diabetes drug, but it is also an anti-inflammatory agent, and I think that is the platform on which this drug is operating on to improve symptoms,” Rasgon told Psychiatric News. “As inflammation is a sign of metabolic dysfunction, one could view depression as an altered metabolic state in the brain.”
Rasgon’s team is now examining how allostatic load—measurements of the physiologic markers that represent the “wear and tear” of the body—relates to chronic depression and pioglitazone therapy.
Even as this work progresses, Rasgon noted that the current findings highlight the potential value of using telomere length as a biomarker to identify people with unremitted depression who would benefit from pioglitazone.
According to Rasgon, telomeres can be readily sequenced from blood cells, and the process does not require all the intricacies of sequencing specific genes.
This study was supported by a grant from the National Institute on Mental Health. ■
“Telomere Length as a Predictor of Response to Pioglitazone in Patients With Unremitted Depression: a Preliminary Study” can be accessed
here. An abstract of “Adjuvant Pioglitazone for Unremitted Depression: Clinical Correlates of Treatment Response” is available
here.