While there are many therapeutic options for treating psychiatric disorders that involve the improper or insufficient activity of brain cells, such as depression or schizophrenia, treatment can be more difficult in neurodegenerative disorders like Alzheimer’s in which cells die—one cannot repair what no longer exists.
One intriguing research avenue in the field of neurodegeneration involves transplanting new nerve cells into the brain. This still experimental therapy holds potential, but needs to overcome a pair of important hurdles: making enough viable neurons to transplant and ensuring survival once neurons are transplanted.
Advances in stem cell technology, notably the ability to generate large amounts of neurons from a patient’s skin cells, are addressing the former issue. A study published March 17 in Nature Communications may help with the latter.
Currently, the neuronal transplantation process is a simplistic affair—cultured cells in a liquid solution are injected into the brain with the hopes that they will graft onto some tissue and start growing.
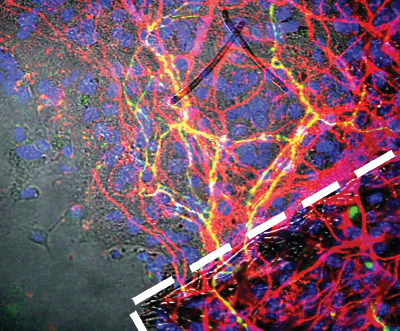
The survival rate of such transplanted cells has been very low. In this new study, a research team at Rutgers University increased the survival rate nearly 40-fold by placing the neurons on tiny organic scaffolds prior to their injection; these micro-scaffolds are 3-D structures that recreate a natural environment and enable the stem cells to begin branching out and making connections—forming synapses—with neighbors before the injection process, in short, helping “prime” the stem cells for their maturation.
Some work has been done in scaffolding already, seeding cells on gels and protein structures, but these designs have had shortcomings; notably, they can encourage stem cells to proliferate but not necessarily mature into neurons. This unchecked proliferation can increase the risk that transplanted cells will form tumors known as teratomas in the brain.
Prabhas Moghe, Ph.D., a distinguished professor of biomedical engineering and chemical engineering at Rutgers, worked with his colleagues to design a scaffold made from a polymer called poly(desaminotyrosyl tyrosine ethyl ester carbonate), or pDTEc, which was spun into a thick, weblike structure.
As Moghe noted in a press release, the spaces formed among the criss-crossing polymer fibers is a critical element. “If the scaffolds are too dense, the stem cell–derived neurons are unable to integrate into the scaffold; whereas if they are too sparse, then the network organization tends to be poor since they can’t sense the presence of their neighbors.”
After testing various combinations on slices of brain tissue, the team found an ideal configuration and tested it in living mice—with high success. In addition to the 40-fold increase in the survival of the injected cells, biochemical analysis revealed the presence of several proteins involved in the formation of neural synapses, suggesting the transplanted cells were not only growing but also becoming functional brain cells.
Moghe’s team is fine-tuning its scaffolding system to specifically develop dopamine-producing neurons for use as a Parkinson’s disease therapy, though there still is a good deal of work left before any human studies can begin. However, they believe that this approach could be adapted to apply to a wide range of brain disorders.
This study was supported by grants from the National Institute of Biomedical Imaging and Bioengineering, National Institute of Neurological Disorders and Stroke, National Institute on Alcohol Abuse and Alcoholism, and National Institute on Drug Abuse. ■
“Generation and Transplantation of Reprogrammed Human Neurons in the Brain Using 3D Microtopographic Scaffolds” can be accessed
here.