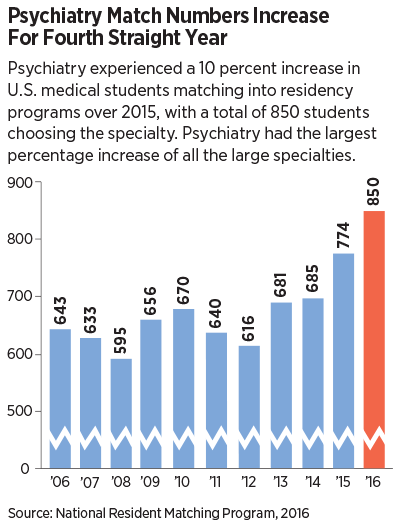
The number of U.S. senior allopathic medical students entering psychiatry through the National Resident Matching Program increased by 10 percent from 2015 to 2016, to a total of 850. This is the fourth consecutive year that psychiatry has seen an increase.
Psychiatry’s number and percentage increases exceeded those of family medicine and emergency medicine, and the percentage increase was greater than those of all other large specialties in the match.
APA Director of Education Tristan Gorrindo, M.D., welcomed the news. “We are seeing a growing interest in pursuing careers in psychiatry among medical students,” he told Psychiatric News. “Anecdotally, students starting psychiatry residencies tell us that they are drawn toward the combination of exciting new frontiers in neuroscience and the continued focus on the most humanistic parts of medicine. These elements together align with the reasons that many medical students chose careers in medicine.”
The annual match, in which the program choices of graduating medical students are paired with those of residency programs seeking trainees, is typically watched as an indicator of workforce size and makeup of the various medical specialties for the coming years.
Sidney Weissman, M.D., a former APA Trustee and past president of the American Association of Directors of Psychiatric Residency Programs (AADPRT), said increasing competition for residency slots is causing medical school students to interview for residencies in multiple specialties—a trend that he believes is helping to fuel psychiatry’s growing numbers.
“The pressure on students to find a residency position helps us,” he said. “Psychiatry did well in this year’s match as senior medical students aware of the limited number of residency positions in sought-after specialties are considering more options as they plan their medical careers. This response from an expanding pool of U.S. graduates will continue to the end of the decade and into the 20s. If we combine the number of osteopathic and allopathic graduates entering psychiatry this year, the number of U.S. graduates will approach 1,000.”
The Association of American Medical Colleges (AAMC) has predicted a shortage of up to 90,000 physicians in the future and called for an expansion of federal funding for residency slots.
In a statement released after this year’s match results, AAMC President and CEO Darrell G. Kirch, M.D., said American medical schools have increased their enrollments by nearly 30 percent to address the coming shortage.
“The nation’s medical schools and teaching hospitals have been doing all that they can to prepare for these expected shortages by expanding enrollments, creating innovative programs to make care more efficient, and training new M.D.s in teams with other health care professionals in a wide variety of settings to improve the health of their communities,” he said. “However, residency growth has not been able to keep up with expanding patient needs because of a 20-year cap on federal support.”
Medicare-funded residency positions have been capped since 1997. Nonetheless, an Institute of Medicine report in 2014 argues against the idea of a coming physician shortage and noted that a 17.5 percent increase in training slots in the last 10 years financed by other sources has not eased geographic shortages or improved the specialist mix. That report, written by a 21-member committee co-chaired by former CMS administrators Donald Berwick and Gail Wilensky, says that shortages are created by poor geographic distribution of physicians and lopsided ratios of primary care and specialty physicians and that recent research suggests the answers lie in new technology and innovations in health care delivery. ■
Data from the National Resident Matching Program can be accessed
here.