There is mounting evidence to suggest underlying connections linking infection, inflammation, and autoimmunity to a surprising number of neuropsychiatric disorders. At the 2016 BIO International Convention in June, a group of clinicians and researchers discussed the apparently rising incidence of these disorders and what can be done to better diagnose and treat them.
“We’re seeing a rapid increase in bipolar-like syndromes in pediatric patients,” Kiki Chang, M.D., a professor of psychiatry and behavioral sciences at Stanford University Medical Center, said during the panel discussion. Chang is a child psychiatrist at a specialty clinic in Stanford’s Pediatrics Department, which treats children with pediatric acute-onset neuropsychiatric syndrome (PANS).
Children with PANS have a combination of neuropsychiatric symptoms, including obsessive-compulsive behaviors, tics, irritability, anxiety, emotional lability, and aggression. The syndrome has a sudden onset, often overnight, and occurs primarily in boys, according to Chang.
One of the known causes of PANS is streptococcal infection. Some children develop antibodies that cross-react with neural proteins, which leads to inflammation in the basal ganglia and causes pediatric autoimmune neuropsychiatric disorder associated with streptococcal infections (PANDAS), a subset of PANS.
Most children with strep throat do not develop PANS or PANDAS, which has led some researchers to believe that those who do develop the syndrome may have genetic variations related to the immune system that render them more vulnerable, Chang said. If researchers are able to pinpoint these genetic variations, they may also uncover new clues about the mechanisms of certain neuropsychiatric and developmental disorders.
The panelists also discussed the role of immunological factors in neuropsychiatric disorders, including mood disorders, dementia, and autism.
“There is a surprising amount of information to support the association between inflammatory symptoms and, for example, autism, but it remains unclear whether the association is cause or effect,” said Dennis Wall, Ph.D., an associate professor of pediatrics at Stanford University School of Medicine.
Wall’s laboratory is sequencing the genomes of thousands of family members of children with autism and using bioinformatics tools to map a clearer picture of the genotypes and phenotypes of the disorder.
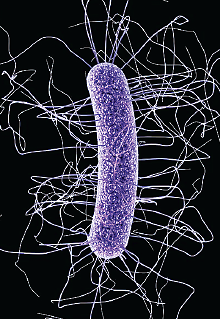
Among suspected environmental contributors to autism, the bacterial flora in the human gut, also known as microbiome, is garnering more attention of researchers, Wall noted. Scientists are only beginning to genotype the DNA of gut bacteria to understand the differences among individuals and the possible effects of abnormal gut microbiome on health. (Wall’s laboratory is sequencing the microbiome DNA of patients with autism in collaboration with the American Gut Project with the hope of identifying disease signatures.)
Panelist Jonas Korlach, Ph.D., the chief scientific officer of Pacific Biosciences, a company specialized in genomic sequencing, described a growing body of published cases of abnormal (e.g., lack of bacteria diversity and abundance) gut bacterial ecology in patients with autism. For example, he noted one study found using antibiotics to suppress Clostridium difficile infection in the gut was associated with behavioral improvements. Korlach, whose son has autism, recounted his search of tests for measuring metabolic and microbiome imbalances that may be the causes or contributors of his son’s autism. He believes that treating these imbalances may help to reduce autistic symptoms.
As a child psychiatrist, Chang has seen an uptick in not only the number but also the complexity of neuropsychiatric disorders in the clinic, he said. “They have ceased to fit into … nice little psychiatric [diagnostic] boxes anymore.” He pointed out that inflammation has only recently been recognized as a possible mechanism leading to neuropsychiatric disorders, but the concurrent and dramatic rise in the incidences of neurodevelopmental disorders and autoimmune diseases, particularly food allergies, should prompt more investigation. He also noted the high incidence of psychiatric comorbidities in patients with inflammatory and autoimmune diseases.
The panel all agreed that medical specialties need to break out of silos and diagnose and treat neuropsychiatric diseases from a whole-body perspective.
“I work directly with a rheumatologist … and infection disease [specialists],” said Chang. He pointed to personal experience in successfully treating children with neuropsychiatric disorders with anti-inflammatory, immunosuppressive, and antibiotic agents. “This is the next frontier.” ■