The human neural network may be infinitely complex, but researchers at Duke University have taken advantage of the much more simplified nervous system of the tiny worm Caenorhabditis elegans (300 neurons) to uncover a key neural circuit that controls the communication between the brain and the gut.
What’s more, they found that this circuit is regulated by a dopamine receptor analogous to the human dopamine receptor D1, the main target of most antipsychotics.
These findings, which were published August 12 in Current Biology, provide some important new details about the cross-talk between the brain and immune system, which impacts a wide range of diseases including schizophrenia, Crohn’s disease, Alzheimer’s, and Parkinson’s, to name but a few.
Lead author Alejandro Aballay, Ph.D., a professor of molecular genetics and microbiology at Duke School of Medicine, cautioned that the leap from C. elegans to humans is immense, but that someday drugs targeting the nervous system could be used to combat immune-related disorders.
Aballay and his graduate student Xiou Cao made the first connection in this gut-brain circuit after treating the worms with the dopamine blocker chlorpromazine and observing that the animals were more resistant to bacterial infection. Conversely, if the worms were given dopamine, they became slightly more susceptible to infection.
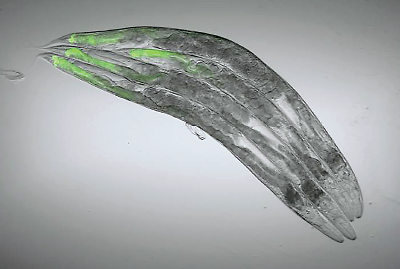
To gain a sense of how this resistance manifested, they used fluorescent bacteria, which enabled them to see that the digestive tracts of the worms given chlorpromazine had lower density of bacteria. This told the researchers that the drug didn’t confer some passive resistance to the pathogens, but rather triggered some active microbial killing mechanisms.
They next made various mutant strains, each lacking a specific dopamine receptor, and saw that only the strains lacking the DOP-4 receptor (the DP-1 analog) maintained their infection resistance.
With the receptor identified, Aballay and Cao then began to piece together the circuit by selectively destroying DOP-4–containing neurons to see which ones affected their bacterial resistance, much like going through each bulb in a string of Christmas lights to find defective ones.
Aballay believes that this circuit relays important information about the state of intestinal flora to ensure the brain doesn’t order any unnecessary inflammatory attacks.
“Humans have trillions of microorganisms in our guts, and we have to be careful when activating antimicrobial defenses so that we mainly target potentially harmful microbes without damaging our good bacteria—or even our own cells—in the process,” he said in a press release.
Dopamine-targeting medications might therefore be used to fine-tune this cross-talk when needed, for example, lowering activity to turn off an autoimmune response. He thinks it might be interesting to see what effects that currently available drugs—like chlorpromazine—might have. Perhaps at lower doses, they may still provide some immune benefits without triggering their neuropsychiatric activity.
This research was supported by grants from the National Institute of Allergy and Infectious Diseases and National Institute of General Medical Sciences. ■
An abstract of “Neural Inhibition of Dopaminergic Signaling Enhances Immunity in a Cell-Non-autonomous Manner” can be accessed
here.