Hope is a natural antidote to despair and demoralization experienced by psychiatric patients that can be encouraged and supported through brief psychothepeutic interventions in crisis situations, according to James L. Griffith, M.D.
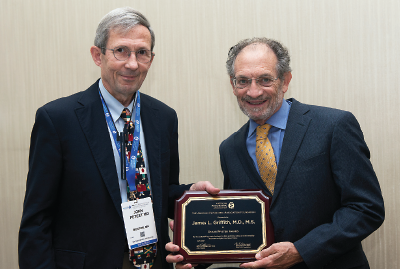
Griffith delivered APA’s 2017 Oskar Pfister Award Lecture last month at IPS: The Mental Health Services Conference in New Orleans. The Oskar Pfister Award was established in 1983 in memory of Oskar Pfister, an ordained minister who studied and used psychoanalytic principles in his work. The award honors outstanding contributions in the field of psychiatry and religion.
Griffith, who is chair of psychiatry at George Washington University (GWU) School of Medicine, described his work developing brief-intervention modules that help patients practice hope in demoralizing life situations and can be taught to trainees and other mental health clinicians.
“Despair from demoralization is a constant threat to patients with chronic mental illnesses, refugees fleeing persecution, elderly who are socially isolated, the medically disabled, and other marginalized or displaced people,” Griffith said.
He said the theoretical basis for his focus on demoralization draws on the work of Jerome Frank, M.D., and his daughter, Julia Frank, M.D., in their 1993 book, Persuasion and Healing: A Comparative Study of Psychotherapy, and of Kaethe Weingarten in the 2010 article in the journal Family Processes titled “Reasonable Hope: Construct, Clinical Applications and Support.” The Franks defined demoralization as “helplessness, hopelessness, confusion, and subjective incompetence” that people feel when sensing that they are failing their own or other’s expectations for coping.
Griffith emphasized that demoralization is a risk for many individuals who may or may not have symptoms of mental illness, but who are experiencing what he called “normal suffering” associated with poverty, loss of status due to job loss, loss of identity, or an uncertain future.
“As psychiatrists, we have skill sets for helping people who are undergoing normal suffering, not just symptoms of mental illness,” Griffith told attendees. “Hope is a common factor associated with change in patients who receive psychotherapy.”
Yet the reality of many individuals’ lives is one of ongoing stress and challenge; therefore, the modules developed by Griffith and colleagues treat hope as a practice—“something you do,” as in a spiritual practice, rather than “something you feel.”
Additionally, it was necessary for hope modules to be time efficient, user friendly for both clinicians and patients, and highly portable across different clinical settings, clinical problems, and patient populations.
Griffith said, “The challenge in developing hope modules came to be: ‘Can you in a single five- to 10-minute conversation accurately discern a person’s signature strength for hope-building and help that person to use that hope-building skill more effectively?’”
Griffith explained that 14 evidence-based hope practices were selected from the research literature in cognitive and social neuroscience, cognitive psychology, palliative care, and psychosomatic medicine. The modules were then created by packaging skill sets for assessment, formulation, and intervention to be used as a single, evidence-based hope practice.
These hope modules then could be inserted into different clinical encounters, and employed in a crisis situation without formal psychotherapeutic training, Griffith said.
A report in the July 27 Academic Psychiatry described the development of the modules as well as the eight-session “Hope Modules Seminar” that has evolved over the past five years as a second postgraduate year (PGY-2) seminar in the psychiatry residency program at GWU. The 75-minute sessions emphasize active learning methods rather than didactic lectures, according to the report.
Residents start by practicing assessments of their own hope-building competencies, then conduct assessments of demoralized patients identified during their clinical services on inpatient psychiatry units, partial hospital program, hospital emergency department, or other clinical services.
Residents are assessed at the end of seminars by clinical portfolios they prepare. Each resident provides clinical vignettes to demonstrate competency in each step of assessment, formulation, and intervention using hope modules with a demoralized patient who was medically or psychiatrically ill.
Anecdotal accounts indicate that residents have not only continued using their hope-module training beyond the PGY-2 year, but also expanded their scope of use. For example, one resident commented, “I have used hope modules in community clinics. This is a population that often lacks the opportunity to talk about and reflect on their own strengths and resiliencies. Case managers often talk with patients by dictating what they should and should not do. I realized that the way I talk with patients is very different due to the hope-module philosophy of eliciting strengths.”
At the IPS meeting, Griffith described several clinical vignettes in which the hope modules were employed to challenge the demoralizing life situations faced by patients. For instance, he described a suicidal patient in despair because her house was being foreclosed, and her dog—a companion of many years—had recently died. A second-year resident at GWU, with no formal training in psychotherapy, asked the patient, “In the past when you faced adversity, what did you do?” The patient recalled that when her father was on his deathbed, he told her she “was a strong fighter” and the “glue that held the family together.”
“In a rapid assessment, the resident recognized that her patient activated a core identity and relied upon attachment relationships with her children when responding to adversity,” Griffith said.
The resident then advised the patient to find a picture of her father and look at it whenever she felt despair, repeating his last words to her. The resident also advised the patient to reach out to her adult children. The patient did both, which initiated additional steps in which she, aided by her children, began coping with her challenging situation.
Griffith said that to design psychotherapeutic interventions that help people practice hope, they must be usable in the real-life conditions in which patients find themselves.
“Hope that is not grounded in reality can be harmful to people,” Griffith said. “The question is how to make hope sustainable when an individual’s reality is seemingly hopeless and secondary stressors are constant. Hope interventions must be usable under the often-chaotic conditions of refugee life, homelessness, poverty, or medical or psychiatric illness where a clinician may have only one or two conversations in settings ill-suited for psychotherapy.” ■
“Hope Modules: Brief Psychotherapeutic Interventions to Counter Demoralization From Daily Stressors of Chronic Illness” can be accessed
here.