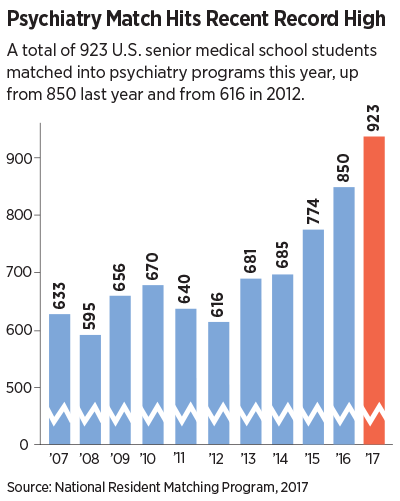
A total of 923 U.S. senior medical school students matched with a psychiatry residency in this year’s National Resident Matching Program (NRMP), up from 850 in 2016.
This year’s figure continues a steady increase in the number of seniors entering psychiatry in recent history. The number of medical school seniors choosing psychiatry grew from 483 in 2000 to 640 in 2010.
The match, in which the choices of graduating medical students are “matched” with those of residency programs, is typically watched as an indicator of workforce size and makeup in the various medical specialties for the coming year.
“This year’s match is good news for our profession and for our patients,” said APA President Maria A. Oquendo, M.D., Ph.D. “There is a shortage of psychiatrists—a drastic shortage in some areas—so of course it is good to see our numbers increasing. Our profession is becoming increasingly attractive to young physicians, promising exciting advances in brain science along with our traditional focus on the person behind the disease.”
APA CEO and Medical Director Saul Levin, M.D., M.P.A., said he believes the trend toward integrated care and advances in neuroscience have raised psychiatry’s profile as the medical profession that treats mind, brain, and body. “This makes our profession attractive to young doctors who want to treat the whole person,” he said. “We welcome new trainees to the profession and invite residents to explore membership in APA.”
What’s Behind the Increase?
In addition to the increasing appeal of the profession, this year’s high reflects many factors, including a larger pool of students entering the match. This year’s match pool was the largest in the history of the NRMP. A record high 35,969 U.S. and international medical school seniors and graduates vied for 31,757 positions, the most ever offered in the match. The number of available first-year (PGY-1) positions rose to 28,849—989 more than last year.
Psychiatry offered 1,495 first-year positions—111 more than in 2016—and filled all but four. The overall fill rate was 99.7 percent, and 61.7 percent were filled by U.S. seniors. Since 2012, the number of psychiatry positions has increased 378, or 34 percent, and the number of positions filled by U.S. allopathic seniors has increased by 307, according to NRMP.
Also possibly contributing to the increase is a trend in which students are applying to more than one specialty and many more training programs than in the past, a response to the perception of heightened competition. Psychiatry has increasingly become an option for students as a hedge against increased competitiveness in other fields.
Sidney Weissman, M.D., a past president of the American Association of Directors of Psychiatric Residency Training (AADPRT) who has closely followed workforce issues, told
Psychiatric News that some medical school seniors are applying to scores of programs, many more than did senior physicians who remember applying to a small handful. “All students feel the need to ensure that they match, so they are applying to multiple programs, including specialties they regard as a default—in the same way that applicants for undergraduate colleges have a ‘safe school.’ ” (
Psychiatric News, February 3).
Commenting on this year’s match results, Weissman said he believes the trend is likely to continue into the next decade. “Students recognize reduced training opportunities and heed the advice of medical school deans to apply to more than one specialty,” Weissman said. “The average applications for U.S. graduates this year exceeded 40 and for international medical graduates (IMGs), it is over 120. This has placed a great strain on the graduate medical education system’s ability to effectively assess every applicant adequately.”
Impact of Trump’s Executive Order Considered
Another issue that may profoundly affect residency programs is that of immigration and policies adopted by the Trump administration to curb immigration and travel from some countries. Weissman and others with whom Psychiatric News spoke agree it is unlikely this year’s match was affected by Trump’s policies.
But Jacob Sperber, M.D., vice chair for education and training and the psychiatry residency director at Nassau Uni-versity Medical Center, said an issue that does affect training directors and residents alike is when residents from other countries return to their country of origin—for holidays or other reasons—and take the chance of being held up or denied return. In an interview with Psychiatric News Sperber said that even prior to the Trump inauguration, some residents have encountered such difficulties, including residents returning from countries not among those listed in the recent revised Executive Order barring immigration from six countries.
Sperber characterized immigration services—including reentry into the U.S. of individuals who hold J-1 visas (the special visas held by many IMG residents)—as a bureaucracy rife with unexplained delays and denials. He said on at least three occasions he has had to write to congressional representatives from New York to help expedite the return of trainees who have been held up on reentry to the United States.
(Sperber chaired a workshop on the issue of immigration at last month’s meeting of AADPRT in San Francisco. Coverage of that workshop will appear in a future issue of Psychiatric News.)
Weissman said the issue could affect the ability of U.S. programs to attract IMGs to psychiatry in the future.
“For over 50 years the United States has relied on IMGs to fill many residency programs and subsequently practice medicine in the United States,” Weissman said. “Many IMGs after graduation serve as the major providers of health care in underserved and rural populations. The nation’s current political climate as it affects immigrants is of concern. If the United States is seen by many young physicians from around the world as not offering a receptive environment for immigrants they will not wish to immigrate here. U.S. health care at all levels will then suffer from the provision of medical care to research.” ■
Information about this year’s match can be accessed
here.