Clinicians typically avoid prescribing psychiatric medications that increase risk of dizziness or disorientation to people at high risk of bone fractures. A study published April 19 in JAMA Psychiatry suggests the risks of fractures among adults taking psychotropic medications may be broader and more significant than was previously appreciated.
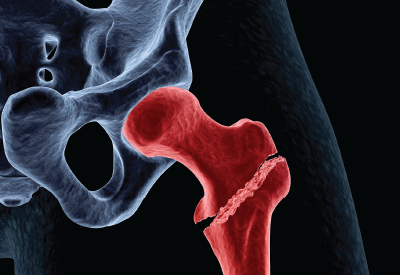
The researchers analyzed data on more than 65,000 adults in Manitoba, Canada, who had received a bone mineral density (BMD) scan. They found that the risk of a major osteoporotic fracture (MOF) was 1.43-fold higher in people taking selective serotonin reuptake inhibitors (SSRIs), 1.43-fold higher among people taking antipsychotics, and 1.15-fold higher among people taking benzodiazepines compared with people not taking these medications. Included MOFs were hip fractures, arm fractures, and vertebrae fractures.
When looking only at hip fractures, one of the most common causes of debility among seniors, the risks were higher still: 1.48-fold higher for SSRIs, 2.14-fold higher for antipsychotics, and 1.24-fold higher for benzodiazepines.
Lead study author James Bolton, M.D., an assistant professor of psychiatry at the University of Manitoba, told Psychiatric News that these results have clinical implications for both primary care and mental health providers.
“First, for general practitioners and other primary physicians, it’s important to recognize that these medications are associated with a significant risk of fracture, one that is not considered in the standard FRAX assessment,” he said. FRAX is a widely implemented evaluation tool that combines BMD scan data with other clinical assessments to measure a patient’s 10-year probability of having a bone fracture.
In fact, Bolton and colleagues quantified the degree that FRAX underestimated risk in people taking psychotropic medication by comparing the actual MOF outcomes in their study sample with the expected number based on average FRAX scores. They found that FRAX underestimated fracture risk by 36 percent among SSRI users, 60 percent among antipsychotic users, and 13 percent among benzodiazepine users.
“As for psychiatrists like myself, the data do suggest that a more refined approach to prescribing may be worthwhile for older adults, especially patients who have an elevated osteoporosis risk such as women,” Bolton said. (About 90 percent of the people in the FRAX study were women.)
When treating depression in older adults, for example, Bolton noted that tricyclic antidepressants did not increase fracture risk in adults, while other antidepressant classes increased overall MOF risks, but not the risk of hip fracture. Likewise, lithium was not associated with any fracture risk, while other mood stabilizers increased MOF risk, but not hip fracture risk.
Because of the way the study was designed, however, Bolton could not consider the mechanisms that underlie this increased fracture risk, which he said he believes is the next important question to ask. One plausible explanation is that these elevated risks reflect an increased rate of falls due to the side effects of psychotropic medication. However, some of the study findings seem to point to other explanations such as a direct effect of psychotropic medications on bone strength and density. For example, there was no association between fracture risk and age for any of the medications, and older age is associated with an increased risk for falls.
This study made use of the Manitoba Bone Density Program database and included adults aged 40 and older who received a bone scan between January 1, 1996, and March 28, 2013. The study cohort included 62,275 women and 6,455 men; of this group, 12,982 had a diagnosis of a mental disorder, 11,938 were using psychotropic medication, and 2,468 were taking multiple psychotropics.
The Manitoba Centre for Health Policy at the University of Manitoba supported this study. ■
An abstract of “Association of Mental Disorders and Related Medication Use With Risk for Major Osteoporotic Fractures” can be accessed
here.