Atrial Fibrillation Increases Risk of Dementia
A Swedish population study that followed individuals for nine years has found that atrial fibrillation is associated with an increased risk of dementia in older adults. This study, which was published in Neurology, also found that using anticoagulant drugs may prevent older patients with atrial fibrillation from developing dementia.
Researchers at the Karolinska Institutet in Stockholm and colleagues analyzed data from 2,685 older adults (average age of 73) who were part of the nine-year Swedish National Study on Aging and Care. All participants were dementia-free at baseline and 243 had atrial fibrillation. Over the nine-year period, an additional 279 participants developed atrial fibrillation and 399 developed dementia.
The researchers found that the presence of atrial fibrillation was significantly associated with faster cognitive decline over time (as assessed by the Mini-Mental State Examination). Atrial fibrillation was also linked with a 40 percent increased risk of any dementia. When assessing specific subtypes, atrial fibrillation was found to be associated with an increased risk of vascular and mixed dementia, but not Alzheimer’s disease.
Among people with atrial fibrillation, use of anticoagulant drugs was associated with a 60 percent decreased risk of dementia compared with patients not taking these drugs. In comparison, drugs to reduce platelet aggregation did not reduce dementia risk.
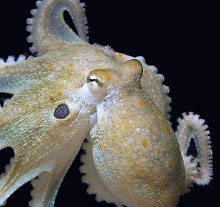
Octopus Study Highlights Evolutionary Conservation of Serotonin Transporter
The DNA sequence for a protein that transports serotonin into neurons appears to be the same in humans and octopuses, suggesting it was evolutionarily conserved across hundreds of millions of years, according to a study in Current Biology. What’s more, the study found serotonin-modulating drugs may have similar prosocial effects in both species.
The study was carried out by investigators at Johns Hopkins University and the Woods Hole Marine Biological Laboratory.
The investigators first examined the genetic sequence of the octopus’ serotonin transporter (the octopus genome was fully sequenced in 2015) and found that a key region known as TM6 was the same as in humans. This region is important as it binds to psychotropic compounds including MDMA (3,4-methylenedioxy-methamphetamine).
Interestingly, while the serotonin transporter gene was also found in other animal genomes, including fruit flies and nematodes, it was absent in all social insects, including ants and bees. This suggests that these species independently developed complex social structures using other chemical signals.
Next, the investigators tested how octopuses responded to serotonin-modulating drugs. They placed one octopus in the center of a three-chambered aquarium, which also housed a second octopus and an inanimate object in the side chambers. After the octopuses, which are normally solitary animals, were given MDMA, they spent considerably more time interacting with the other octopus than the inanimate object.
“Based on our ability to induce prosocial approach behaviors by manipulating serotonergic signaling, it is tempting to speculate that in octopuses, sociality is a latent state… and is manifested in response to MDMA treatment,” the authors wrote.
Researchers Develop Calculator to Predict Teen Smoking
Researchers at the University of Montreal and colleagues have developed a 12-item clinical scale that can identify youth most likely to start smoking.
The researchers compiled data from a longitudinal study of nearly 1,300 adolescents at 10 high schools in Montreal. As part of this study, the teens completed questionnaires that included questions about smoking, every three months for five years.
Of the 58 traits the researchers examined (including demographics, family smoking history, lifestyle, and personality traits), the team identified a list of 12 traits that showed the strongest association with starting smoking within one year: age, four stress-related traits (worries about loneliness, weight, health, or relationship with siblings), four substance-use traits (drinks alcohol, has friends who smoke, feels the need for cigarettes, finds it hard not to smoke when others are smoking), two self-esteem traits (feels he/she has something valuable to offer, has a positive attitude about oneself), and one depression-related trait (hopelessness).
The researchers then developed and tested a calculator using these variables. They found that youth with the highest scores had about a 78 percent risk they would begin smoking within one year.
“If the predictive ability is replicated in other settings, this tool can be used to help clinicians select who should be counseled and, because several items in the tool are amenable to prevention, how they should be counseled,” the investigators wrote.
This study was published in Pediatrics.
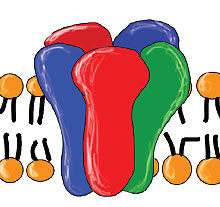
GABA Receptor Density Similar in People With, Without Autism
Some studies suggest that symptoms of autism spectrum disorder (ASD) are due to a deficiency of GABAA receptors in the brain, but few have examined receptors in patients who are medication-free.
A study published in Science Translational Medicine now suggests that adults with ASD do not have fewer GABAA receptors than those without ASD.
A team led by researchers at King’s College London took positron emission tomography (PET) scans of 27 medication-free adults with ASD and 31 controls. The participants were divided between two imaging sites (London and Stockholm), with each site using its own molecular tracer.
Both sites found no evidence of different GABAA receptor concentrations between people with ASD and controls. They also conducted brain scans of three different mouse models of ASD, none of which displayed lower GABAA receptor levels than control mice.
The researchers noted that people with ASD performed worse on a visual perception task, which is believed to involve GABA signaling.
“This raises the possibility that the GABAergic system may be dysregulated in ASD despite an intact GABAA receptor density in the brain,” the authors wrote. “For instance, it is possible that the synthesis or release of GABA is down-regulated in ASD, leading to impaired GABAergic signaling.”
Prescribing Errors Common in People With Parkinson’s
About 45 percent of Medicare beneficiaries with Parkinson’s disease and a clinical diagnosis of dementia were co-prescribed a high-potency anticholinergic medication and an acetylcholinesterase (ACE) inhibitor, according to a study in JAMA Neurology.
“Coadministration of a drug with high anticholinergic activity and an ACHEI [ACE inhibitor] represents a frank prescribing error because these drugs have opposing pharmacologic effects,” wrote authors from the University of Pennsylvania Perelman School of Medicine and colleagues.
They used available Medicare data to identify 268,407 adults with a diagnosis of Parkinson’s disease who had 12 consecutive months of inpatient, outpatient, and prescription drug coverage from January 1, 2014, through December 31, 2014. Among these patients, 73,093 were given a prescription for at least one antidementia medication during the study period, of which 64,017 received at least one ACE inhibitor.
Among patients prescribed an ACE inhibitor for dementia, the concurrent use of anticholinergics was high. Over 80 percent of the patients filled a prescription for an anticholinergic agent at least once during 2014; 68 percent had a concurrent prescription with a low-potency anticholinergic (such as codeine or the blood thinner warfarin); and 45 percent filled at least one concurrent prescription for a high-potency anticholinergic (such as the antipsychotics olanzapine and quetiapine).
Further analysis showed that this prescribing error was present across the United States, but southern and midwestern states had especially high rates of co-prescribing ACE inhibitors with strong anticholinergics. “These findings may serve as national and local targets for improving care quality and outcomes for persons with Parkinson’s disease,” the authors wrote. ■