The popularity of psychiatry as a specialty choice among medical school seniors—and competitiveness for residency slots—may be increasing, according to recent data from the National Resident Matching Program (NRMP).
Between 2014 and 2018, psychiatry residency programs saw a 65 percent increase in applications from U.S. seniors, said John Spollen, M.D., a professor of psychiatry at the University of Arkansas Medical School, who presented an analysis of the NRMP data at the September meeting of the Association for Academic Psychiatry in Milwaukee. Spollen’s analysis was part of a workshop at the meeting on “Evidence-based Recruitment and Advising for Future Psychiatrists.”
Meanwhile, the increase of senior applicants during the same period was just 8 percent. Moreover, in 2018 a total of 254 U.S. medical school seniors who applied to psychiatry did not match into any program.
“This year the rate for psychiatry [of unmatched applicants] was 13.7 percent, which was the highest among any specialty in medicine,” Spollen told Psychiatric News in an interview.
U.S. medical school seniors today are often applying to more than one specialty, and some applicants may have been applying to psychiatry as a backup. But Spollen also pointed out that of the 254 U.S. medical school seniors applying to psychiatry in 2018 who did not match into psychiatry, 146 had chosen only psychiatry.
Moreover, of the 1,236 U.S. senior applicants to psychiatry last year, only 87 had ranked psychiatry as a backup to another specialty, Spollen said.
The specialties with the next highest numbers of unmatched applicants who had applied to only one specialty were orthopedics (103 unmatched), obstetrics-gynecology (96 unmatched), emergency medicine (77 unmatched), and surgery (60 unmatched).
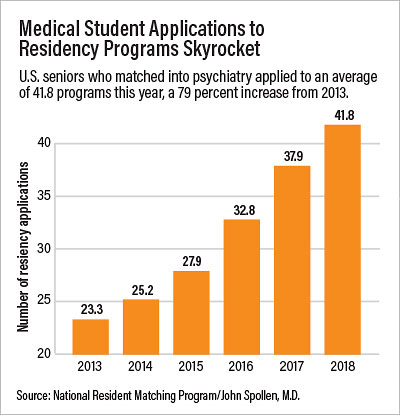
Like other specialties, psychiatry has experienced a dramatic increase in the number of programs to which medical students are applying. This year, students matching into psychiatry applied to an average of 41.8 programs—a stunning amount for senior psychiatrists who recall applying to only a handful of programs.
Spollen said it is possible that the heightened competitiveness of the match overall has simply spilled over into psychiatry, with medical school seniors with weaker applications being encouraged to choose between specialties historically regarded as easier to get into. It is also possible, however, that the new generation of medical school students is genuinely attracted to a psychiatry that is now more integrated into general medicine.
“Stigma of mental illness, and maybe of psychiatry as well, could be less among this generation of medical students,” Spollen suggested.
He added that “millennial” students value work-life balance and regard psychiatry as attractive on that score. In a report published last year in the American Journal of Psychiatry, Spollen and Mathew Goldenberg, M.D., found that among medical school students who hadn’t intended to go into psychiatry but decided to do so during medical school, the variable most highly associated with the switch was work-life balance.
“Recruitment efforts that emphasize psychiatrists’ high satisfaction with work-life balance and low rates of burnout may increase interest among those not initially considering psychiatry,” they wrote. “Discussing the regular work hours and reasonable on-call responsibilities that most practicing psychiatrists enjoy may help attract millennial students, whose values may differ from those of previous generations of physicians.”
The rising number of U.S. medical school seniors applying to psychiatry—if it continues—means psychiatry is becoming especially competitive for international medical graduates (IMGs) who have traditionally filled many of the U.S. residency slots. “Coincident with this surge in U.S. seniors matching into psychiatry is a 32 percent decrease in the numbers of IMGs matched into psychiatry over the same time period,” Spollen said. “My interpretation is that U.S. seniors are essentially pushing IMGs out of the psychiatry match. D.O. applicants matching into psychiatry also increased by 63 percent since 2014, and they likely next year will be a larger portion of the match than IMGs for the first time ever.”
Mark Rapaport, M.D., chair of the APA Council on Medical Education and Lifelong Learning, views the data suggesting increased popularity of psychiatry somewhat more cautiously.
“I’d really like to see this trend continue over a number of years,” he told Psychiatric News. “It’s quite possible that the profession really is more popular and will continue to be so. We have more effective psychotherapies, pharmacotherapies, and somatic therapies that we are able to give our patients. And the more we get away from fee-for-service payment arrangements, the greater respect we get within an organization or health system. I think if we see these numbers continue over a number of years, it might indicate a significant sea change.”
Spollen said he believes medical students and advisors should be aware that the profession is at least somewhat more competitive than before.
But applying to more programs is not necessarily the answer; rather, students should be advised to choose the programs they apply to more carefully based on their aptitudes and interests. “Students are going to have to be smarter about where they apply. The numbers of applications are less important than the types of programs a student applies to.” ■
“Stability of and Factors Related to Medical Student Specialty Choice of Psychiatry” can be accessed
here.