Are substance use disorders being underdiagnosed and undertreated by psychiatrists?
Between 2012 and 2015, psychiatrists diagnosed a substance use disorder (SUD) or prescribed a medication for it during 9 percent of office visits, according to an analysis published January 16 in Psychiatric Services in Advance.
Authors Tami L. Mark, Ph.D., M.B.A., and Angȳlica Meinhofer, Ph.D., of the Department of Behavioral Health and Criminal Justice at RTI International in Research Triangle, N.C., derived the 9 percent figure from an analysis of the National Ambulatory Medical Care Survey (NAMCS), a nationally representative survey conducted annually by the Centers for Disease Control and Prevention on visits to office-based physicians.
Noting that a separate database (the National Survey on Drug Use and Health) has indicated 20 percent of adults with mental illness also have a co-occurring substance use disorder, Mark and Meinhofer said that the NAMCS analysis suggests something critical: there may be a lot of individuals with an SUD that psychiatrists aren’t diagnosing and treating.
Physicians who participate in the NAMCS are asked to fill out information on the patients that they treat over a one-week period including their diagnoses and prescription medications.
“It is important to note that these data are not used for payment and do not identify the patient, so there is no reason that a psychiatrist would feel the need to under-code substance use disorders to avoid problems with insurance payment or to protect the patient from being stigmatized,” Mark said.
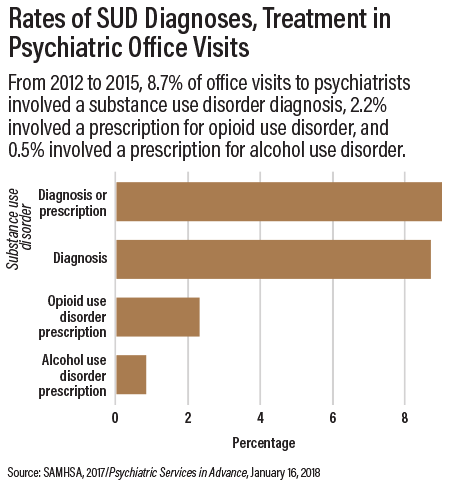
The NAMCS showed that 8.7 percent of office visits to psychiatrists involved an SUD diagnosis, 2.2 percent involved a prescription for opioid use disorder, and 0.5 percent involved a prescription for alcohol use disorder (see chart).
“We know a large portion of patients being treated by psychiatrists have both mental illnesses and untreated alcohol and drug problems,” Mark said. “We also know that integrated care is the best approach to treatment. Our study points to the need for more research and training to ensure that psychiatrists are identifying substance use disorders among their patients and are providing effective integrated care.”
Andrew Saxon, M.D., chair of the APA Council on Addiction Psychiatry, said these data should be a wake-up call. “Many substance use disorder specialty treatment programs do not have psychiatrists on staff to treat co-occurring psychiatric disorders,” he said. “If practicing psychiatrists are not treating these patients, who is?
“Psychiatrists may fail to do so because the training in medical school and even psychiatric residencies to learn to treat substance use disorders is inadequate and because patients with co-occurring disorders are more complex and take more time, yet the reimbursements for caring for these patients may be insufficient to compensate for the time and effort,” he said. “We can address this gap by improving our training programs and reimbursement schedules.”
Council co-chair John Renner, M.D., echoed those comments. “This report documents a major public health problem—namely, that psychiatrists, like most other physicians, are poorly trained to diagnose and treat substance use disorders,” he said.
Saxon and Renner noted that the American Association of Directors of Psychiatric Residency Training (AADPRT) is developing an initiative to improve residency training in assessment and treatment of people with substance use disorders.
However, at least one health services researcher questioned whether the figure of 20 percent can be extrapolated to the population that seeks psychiatric care. Mark Olfson, M.D., M.P.H., a professor of psychiatry at Columbia University Medical Center, noted that evidence from the NSDUH and the National Comorbidity Survey suggests that adults with SUDs are approximately half as likely as those with depression or more severe anxiety disorders to receive treatment from a psychiatrist.
Olfson said it may not be possible to draw inferences about clinical detection of substance use disorders on the basis of diagnostic records without an independent assessment of underlying clinical prevalence of various disorders.
“Although the findings are provocative and more can always be done to improve substance use treatment, the new results leave open the question of what proportion of psychiatric patients with substance use disorders are diagnosed and treated,” Olfson said. “As compared with people with other common mental disorders, those with substance use disorders are considerably less likely to recognize their problems, voluntarily seek help, and engage in treatment.” ■
“The Extent to Which Psychiatrists Diagnose and Treat Substance Use Disorders” can be accessed
here.