City dwellers in poorer, developing countries are not at greater risk of psychosis, a finding that counters multiple studies in wealthy, developed countries showing an association between “urbanicity” and psychosis. A report appearing in the July JAMA Psychiatry, however, suggests that the association between urbanicity and psychosis, rather than being a universal phenomenon, may be a feature of industrialized countries only.
Jordan E. DeVylder, Ph.D., an associate professor in the graduate school of social service at Fordham University, and a team of international researchers analyzed data from the World Health Organization (WHO) World Health Survey, which was conducted in 70 countries from May 2, 2002, through December 31, 2004. Data from a total of 42 countries were analyzed in the final sample, including 17 classified by WHO as “low-income countries” and 25 classified as “middle-income countries.”
A total of 215,682 respondents whose place of residence at the time of the survey was either “urban” or “rural” were included in the analysis.
Respondents were asked the following questions with answer options of “yes” or “no.”
During the last 12 months, have you experienced
•
a feeling that something strange and unexplainable was going on that other people would find hard to believe? (delusional mood)
•
a feeling that people were too interested in you or there was a plot to harm you? (delusions of reference and persecution)
•
a feeling that your thoughts were being directly interfered with or controlled by another person or your mind was being taken over by strange forces? (delusions of control)
•
an experience of seeing visions or hearing voices that others could not see or hear when you were not half asleep, dreaming, or under the influence of alcohol or drugs? (hallucinations)
Individuals who endorsed at least one of these four symptoms were considered to have had psychotic experiences.
Overall, no significant association of urban residence with psychotic experiences was found in either low-income or middle-income countries. The pooled odds ratio for the association between urbanicity and psychotic experiences for all countries was 0.99 (nonsignificant). Associations between urbanicity and psychotic experiences remained nonsignificant when examined separately in younger adults (aged 18 to 29 years) and those 30 years or older.
The researchers suggested that the results call for a re-interpretation of studies—mainly from wealthy, developed countries—showing an association between psychosis and city living. Specifically, it indicates that urbanicity has been a proxy for other variables unique to wealthy, developed countries.
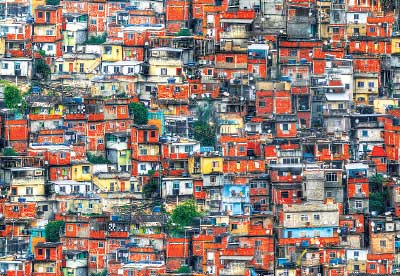
“Speculatively, urban-rural disparities in economic deprivation and social isolation in high-income countries may not be present or may be less evident in low- and middle-income countries,” they wrote. “Affluent members of society tend to populate suburban areas in high-income countries, which differs from developing countries. Furthermore, familial and social cohesion may remain stronger in urban areas of developing countries.”
In an editorial accompanying the study, John McGrath, M.D., Ph.D., a professor in the school of clinical medicine at Queensland Brain Institute in New Zealand, and two other authors noted that the new study upsets a long unquestioned hypothesis.
“Psychiatric epidemiology has a longstanding interest in understanding how the social environment influences mental health,” they wrote. “It felt good to implicate the social environment as a risk factor for schizophrenia; it helped ward off accusations of biological reductionism. If we could address social inequality and reduce discrimination against minority groups, reduce overcrowding, and improve neighborhood social capital, could we reduce the incidence of schizophrenia? It was a very appealing and comforting hypothesis.”
McGrath and colleagues concluded: “We now know that these differences appear consistently in high-income Nordic and northern European countries but vanish in low- and middle-income countries. If these findings are mediated by social adversity and neighborhood-level stressors, then the research community will need to revise and particularize hypotheses for some countries but not others. New hypotheses and targeted research investments are strongly needed in this field. This will be the challenge for the next generation of researchers.” ■
“Associations of Psychosis With Urbanicity in Low- and Middle-Income Countries” can be accessed
here. The editorial is posted
here.