Smoking cessation is an important public health goal for patients with severe mental illness such as schizophrenia. Available data show that smoking rates among people with schizophrenia are three times as high as in the general population, and smoking-related diseases such as heart disease are major causes of death in these patients.
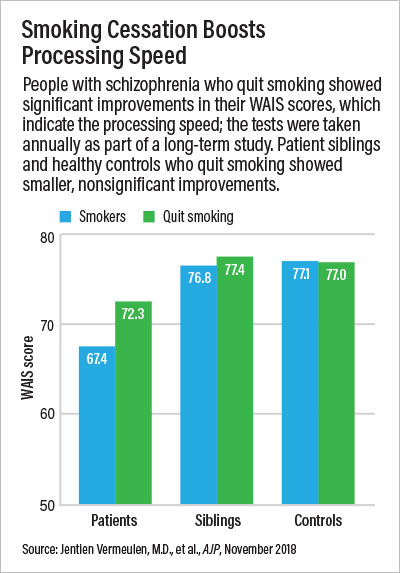
In addition to the long-term physical benefits of smoking cessation, a study published in American Journal of Psychiatry in November provides evidence that quitting smoking can lead to immediate cognitive improvements in patients with psychosis. Making use of population data on over 1,000 psychosis patients along with their siblings and control subjects, researchers found that people with psychosis who quit smoking performed mental tasks faster than they did when smoking.
These findings underscore the impact smoking has on both physical and mental health of patients with psychosis, according to lead study author Lentien Vermeulen, M.D., of the Amsterdam Institute for Addiction Research and colleagues. “[M]ore psychoeducation about the potential long-term negative effects of smoking on cognitive performance is necessary,” the researchers wrote.
The researchers analyzed data from the Genetic Risk and Outcome of Psychosis (GROUP) study, which followed patients with nonaffective psychosis (psychosis without an accompanying mood disorder), their unaffected siblings, and unrelated healthy controls over a six-year period. The goal of GROUP was to see how genes and the environment shape the progression of psychosis. As part the study, participants received cognitive tests at baseline and then three and six years later. The authors had complete cognitive data for 916 patients, 947 siblings, and 552 controls.
At baseline, two-thirds of the psychosis patients smoked, compared with 38.3 percent of the siblings and 25.2 percent of the controls. The authors identified a significant association between smoking and lower performance in tasks related to processing speed, working memory, and/or problem solving in all three groups. For processing speed and problem solving, the deficits were dose-dependent; that is, the more cigarettes smoked per day, the lower the average performance.
The authors did not identify any significant changes in cognition among participants who started smoking during the study period. This likely means that the cognitive deficits are a result of chronic nicotine exposure, they noted.
Assessments at follow-up visits showed that patients who quit smoking had significant improvements in processing speed compared with those who did not quit smoking. Interestingly, they noted, this association was not seen in siblings or control subjects.
“The data from Vermeulen et al. make a powerful argument for interventions aimed at smoking cessation in individuals with severe mental illness,” wrote Philip Harvey, Ph.D., a professor of psychiatry and behavioral sciences at the University of Miami Miller School of Medicine, in an accompanying editorial. “The rapid return of cognitive performance in quitters with severe mental illness, particularly in a domain [processing speed] with considerable functional relevance, is a strong argument for rapid benefits.”
Tony George, M.D., chief of the Addictions Division at the Centre for Addiction and Mental Health in Toronto told Psychiatric News that he likes to see big studies tackle the question of how smoking affects cognition in psychosis. “There aren’t that many researchers looking into this,” he said.
As for the results, though, he said he thinks the study design makes it difficult to definitively interpret the findings.
“One area the researchers did not control for in the smokers was time since the last cigarette,” he said. Smoking alters brain activity in a time-dependent manner, such that someone who just finished a cigarette will feel more alert and less cranky than someone who last smoked a few hours ago. Therefore, a smoker’s performance on cognitive tests can fluctuate greatly depending on their behavioral state, much more so than nonsmokers.
“Even if these findings are verified, I don’t know if it will have much impact [on therapy], as cognition is sort of an abstract concept,” George continued. People with severe mental illness are much like regular smokers, he said, and relatable incentives like “you will live longer” or “do you want to avoid more heart attacks” are more useful in getting them to change their behaviors.
The GROUP study is funded through the Geestkracht program of the Dutch Health Research Council, with additional support from several pharmaceutical companies, universities, and mental health care organizations in the Netherlands. ■
“Association Between Smoking Behavior and Cognitive Functioning in Patients With Psychosis, Siblings, and Healthy Control Subjects: Results From a Prospective 6-Year Follow-Up Study” can be accessed
here. “Cigarette Smoking, Cognitive Performance, and Severe Mental Illness: Quitting Smoking Really Does Seem to Matter” is available
here.