Aetna, one of the nation’s largest health insurers, agreed to a settlement last month with the Massachusetts Office of the Attorney General (AG) requiring the company to comply with state and federal laws by maintaining accurate, updated provider directories and network adequacy.
The legal action brought by Massachusetts AG Maura Healey alleged that the health insurer violated state law because of inaccurate and deceptive provider directories and inadequate provider networks. The legal action also alleged that Aetna violated state law by unfairly denying or impeding member coverage for substance use disorder treatments.
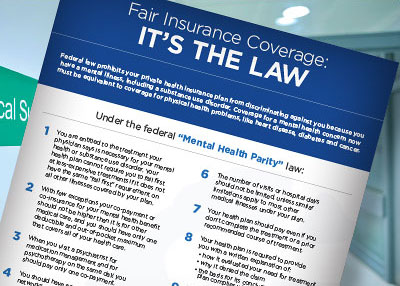
Since regulations regarding the Mental Health Parity and Addiction Equity Act (MHPAEA) were issued by the Centers for Medicare and Medicaid Services, APA has worked to educate attorneys general, insurance commissioners, consumers, state and federal legislators, and employers about MHPAEA requirements regarding network parity for mental and substance use disorders, both in consumer access and in provider payment.
APA has conducted “secret shopper” surveys in many states bringing to local authorities’ attention the fact that insurers frequently misrepresent the depth and breadth of their networks in violation of consumer protection laws. The surveys have also revealed that health plans violate mental health parity regulations by failing to pay psychiatrists the comparable rates for the same services as other physicians.
In 2016, for example, a team of researchers with the APA Foundation telephoned a randomly selected sample of psychiatrists publicly listed as network psychiatrists for the three largest health insurance carriers in Washington, D.C. They found that most of the network psychiatrists listed as practicing in the area either were not able to schedule an appointment or were not even reachable at the listed telephone numbers.
The analysis revealed that close to a quarter of the phone numbers for the listed psychiatrists were nonresponsive or were nonworking numbers. And only 15 percent of psychiatrists were able to schedule any appointment for callers; in one plan, only 4 percent were able to schedule an outpatient appointment.
The findings highlight a problem that has hindered access to care and the implementation of parity nationwide: the use by health plans of “narrow” or “phantom networks” that advertise to enrollees an ample selection of psychiatrists, but which in fact offer very few real options for timely care. In many cases, listed providers are not accepting new patients and others have moved out of the geographic area; in some reported cases, listed psychiatrists are retired from practice or deceased.
“Attorney General Healey is to be commended for acting on behalf of citizens in her state who need access to mental health and substance abuse treatment,” said APA CEO and Medical Director Saul Levin, M.D., M.P.A. “APA staff were invited and spoke to state attorneys general, state insurance commissioners, consumer groups, legislators, and employers to explain the importance of network adequacy. The settlement by Aetna with the Massachusetts AG office shows that those efforts are beginning to produce results.”
In the settlement, Aetna agreed to pay $75,000 to the commonwealth as a civil penalty and to cover attorneys’ fees and agreed to not engage in any unfair or deceptive acts or practices in violation of state law. The company further agreed to do the following:
•
Comply with state and federal laws by maintaining accurate and updated provider directories and network adequacy, outlining detailed and specific information to be included and action that must be taken.
•
Maintain an adequate behavioral health network in numbers and types of providers so that services are accessible to members without unreasonable delay, with specific, detailed information that must be listed in directories and requiring periodic audits of provider networks.
•
Conduct provider outreach quarterly to validate directory information and conduct monthly audits of its Behavioral Health Provider Directory.
•
Track and monitor member complaints related to provider directories, network adequacy, timely access to care, and out-of-network claim disputes and clearly provide notice to members that they may file complaints about provider network inadequacy to the state Division of Insurance.
•
Comply with state law by covering specific medically necessary substance use disorder services and not requiring members to obtain preauthorization for specific substance use disorder services.
As part of the settlement, the Massachusetts AG office will monitor Aetna’s fulfillment of the settlement. “Massachusetts patients face far too many barriers to receiving essential mental health and substance use treatment,” said AG Maura Healey in a statement. “With these commitments, Aetna is making it easier for patients to access the care they need.” ■
The settlement between Aetna and the Massachusetts Attorney General can be accessed
here.