Duloxetine’s Effects Partially Mediated By Gut Microbiome
Duloxetine and other antidepressants can change the composition of gut bacteria, and this alteration in microbial diversity is partially responsible for reducing depressive symptoms, according to a study in Translational Psychiatry.
Researchers at Israel’s Bar-Ilan University treated mice with one of five antidepressants (desipramine, duloxetine, escitalopram, fluoxetine, and venlafaxine) for 21 days and then analyzed the animals’ gut microbiome in comparison with control mice. They found that all the antidepressants except desipramine reduced the richness of the microbial communities. The levels of Ruminococcus and Adlercreutzia bacteria were in particular greatly reduced.
To test if this change in composition had any meaningful effects, the researchers performed behavioral tests on mice treated with duloxetine, a bacterial supplement (Ruminococcus flavefaciens or Adlercreutzia equolifaciens), or both. Though A. equolifaciens showed no effect, mice treated with duloxetine and R. flavefaciens exhibited more depressive behaviors than those treated with duloxetine alone.
However, mice given R. flavefaciens plus duloxetine also had less constipation than those given duloxetine alone. This suggests that duloxetine-triggered reduction of the R. flavefaciens gut population may contribute to both the medication’s therapeutic effect and one of its main side effects.
Maintenance Opioid Therapy Reduces Arrest Risk
A study published in Addiction reports that people with opioid use disorder (OUD) who maintain themselves on buprenorphine or methadone treatment have lower rates of arrest or incarceration. These findings provide some of the first evidence that OUD therapy has societal as well as health benefits.
Researchers at the University of Massachusetts and University of California, Los Angeles, assessed long-term follow-up data from a study that examined the effects of 24 weeks of buprenorphine or methadone therapy on liver function in patients with OUD. This analysis looked specifically at the 303 participants from California (179 on buprenorphine and 124 on methadone) since this was the only state with available criminal justice data. These participants received follow-up interviews about five years after study completion.
The participants who had stayed on buprenorphine or methadone treatment after the study ended were half as likely to have been arrested or incarcerated during the follow-up period compared with those who had stopped treatment. Participants who had taken methadone for the study but then switched to buprenorphine also had a reduced risk of arrest or incarceration, whereas participants who switched from buprenorphine to methadone had similar risks as participants who had stopped treatment.
“Clearly, more studies are needed to understand the characteristics of individuals who change medication types, predictors of medication changes, and why such changes are associated with differential criminal justice outcomes,” the researchers wrote.
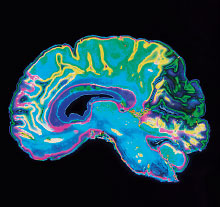
Behavior Dysregulation Shows Altered Brain Activity in Teens
Using neuroimaging, researchers have identified differences in brain structure and activity in adolescents with emotional and conduct problems compared with teens with no behavioral dysregulation. These findings, published in the Journal of the American Academy of Child & Adolescent Psychiatry, provide more insight into how childhood conduct problems manifest and may aid in diagnosing this condition.
University of Vermont investigators and colleagues analyzed MRI scans of more than 2,000 14-year-olds who were enrolled in the multinational IMAGEN study of adolescent development. IMAGEN participants had brain scans taken while completing a variety of behavioral tasks. They also completed the 25-item Strengths and Difficulties (SDS) Questionnaire, which assesses five behavioral domains: emotional symptoms, conduct problems, hyperactive behavior, peer problems, and prosocial behaviors.
The investigators found that children considered to be behaviorally dysregulated—elevated scores in all five SDS domains—had significantly reduced gray matter in their right orbitofrontal cortex (involved in decision making) compared with a matched set of teens with no elevated SDS scores. Teens with high behavioral dysregulation also displayed higher neural activity in this region when performing a task measuring inhibition, versus matched controls. No differences were found between the groups when performing facial recognition or reward-processing tasks.
The investigators cautioned that these findings come from a snapshot of these children at one time point. “[G]iven the neurodevelopmental changes under way at age 14, it is unknown if the neuroanatomical difference identified here persists throughout the lifespan,” they wrote.
New Animal Model Mimics Prodromal Schizophrenia
Researchers at the University of Queensland and colleagues have developed a rat model of schizophrenia that recreates one of the key abnormalities of this disorder: an increase in dopamine synthesis and release in the brain’s dorsal striatum (DS) region. The researchers noted that increased dopamine activity in the DS often corresponds with the transition from subclinical psychosis to clinical schizophrenia, so this new animal model would be valuable for studying this prodromal disease state.
This new model, termed Enhanced Dopamine in the Prodrome of Schizophrenia (EDiPS), was developed using special genetic constructs containing two key enzymes involved in the production of dopamine: GTP cyclohydrolase 1 and tyrosine hydroxylase. The researchers delivered these constructs directly into the animals’ substantia nigra brain region. Neurons in the substantia nigra project directly into the DS, so these constructs would trigger overexpression of dopamine and direct release into the DS. The researchers injected the constructs into the rats at 35 days of age, which is equivalent to human adolescence.
These animals displayed several traits that mimic the positive symptoms of schizophrenia, such as hyperactivity and impaired pre-pulse inhibition (the ability to lessen the effects of a strong stimulus like a loud sound by pre-exposing a subject to a less intense version of that stimulus). “Further work is necessary to identify whether EDiPS animals demonstrate any behaviours relevant to the negative symptoms or cognitive impairments seen in patients,” the researchers wrote.
This research was published in NPJ Schizophrenia.
Co-Occurring Psychosis Does Not Diminish Effects of Depression App
A depression-related mobile app known as FOCUS improves mood equally in depressed patients with or without co-occurring psychosis, reports a study in JMIR Mental Health. This study, led by investigators at the University of Washington in Seattle, also found that the diagnostic cause of depressive symptoms (major depression, bipolar disorder, or schizophrenia) did not affect the efficacy of the FOCUS app, nor did the use of antidepressant medications.
“Our findings go against current skepticism about the viability of computerized interventions for people with psychosis,” the investigators wrote. “FOCUS might be a useful intervention to address moderate to severe depressive symptoms among individuals with an array of mental illnesses.”
These findings come from an analysis of 82 adults with a range of mental illnesses who were in the active arm of a randomized, clinical study of FOCUS, a mobile intervention that targets various psychiatric symptoms, including mood, sleep problems, hearing voices, and social functioning. FOCUS was initially developed to support the treatment of schizophrenia, but this study explored its use with additional patient groups.
At the end of the 12-week study and six months later, the patients who used FOCUS showed statistically similar improvements in their Beck Depression Inventory II scores regardless of their initial diagnosis or presence of psychotic symptoms. The only difference uncovered by the investigators was that patients with mild depressive symptoms did not show much improvement, while those with moderate or severe symptoms did. ■