Prolonged exposure—a therapeutic approach that has people relive traumatic experiences in a controlled setting—is considered a first-choice treatment for posttraumatic stress disorder (PTSD). Yet people with PTSD who also have alcohol use disorder (AUD) are often not offered exposure therapy because of concerns that the stress of exposure therapy could cause these patients to increase their drinking.
A clinical study published April 24 in JAMA Psychiatry refutes this idea, demonstrating that veterans with both PTSD and AUD can tolerate and benefit from exposure therapy. In fact, exposure therapy outperformed the treatment these patients are frequently offered: coping skills therapy, an approach that teaches patients skills to manage their trauma and prevent drinking relapse.
This study included 119 veterans (107 men) with PTSD and AUD who were randomly assigned to receive 12 sessions of either integrated exposure therapy or integrated coping skills therapy (the “integrated” tag means the therapies focused on both PTSD and AUD symptom management). The participants were asked to attend at least one session a week but were allowed up to six months to finish their designated therapy.
The participants experienced an average of eight traumatic events during their life, including combat trauma, sexual trauma, serious illness, or exposure to a disaster. Many of the participants also misused other substances in addition to alcohol. As lead author Sonya Norman, Ph.D., a professor of psychiatry at the University of California, San Diego, and a staff psychologist at the Veterans Affairs San Diego Healthcare System, explained, this group is a good representation of a “complicated patient.”
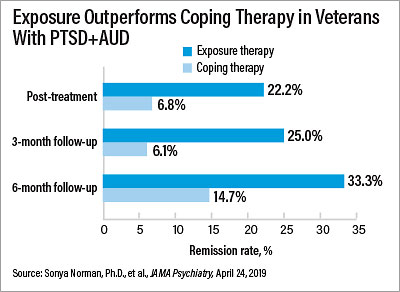
At the end of the study, participants in both treatment groups showed significant reductions in their PTSD severity (measured with the Clinician-Administered PTSD Scale for DSM-5, or CAPS-5). However, the prolonged exposure group had greater CAPS-5 reductions, with an average score of 25.8 (down from 43.2 at baseline) compared with 32.9 (down from 42.1) in the coping skills group. More veterans receiving exposure therapy also achieved PTSD remission (22.2% vs. 6.8% in the coping skills group), defined as a CAPS-5 score of less than 12 (see chart).
That 1 in 5 of the prolonged-exposure group achieved remission is encouraging, Norman said. “There was a time when therapists believed these severe cases of PTSD were akin to a chronic illness: Symptoms could be managed but you could not treat the underlying disorder. Now we know that we can effectively treat [these] patients.”
Both treatment groups also had similar reductions in alcohol use. Their total number of heavy drinking days (five or more drinks per day for men, four or more for women) decreased by more than half, and they doubled their number of days abstinent from any alcohol.
Though this study specifically addressed alcohol use, Norman thinks that integrated exposure therapy should work for any substance use problem. Many of the study participants were taking multiple substances and still improved, he said. “I’ve had people tell me that research studies with exposure therapy all involve perfect patients with one distinct traumatic event and no other medical problems and therefore it couldn’t work for real-world patients with complex problems,” she told Psychiatric News.
“I hope these findings help dispel that myth,” she continued.
This study was supported by a VA Clinical Science Research and Development Merit Grant with additional support via training fellowships through the VA Office of Academic Affiliation and the National Institute on Alcohol Abuse and Alcoholism. ■
“Efficacy of Integrated Exposure Therapy vs Integrated Coping Skills Therapy for Comorbid Posttraumatic Stress Disorder and Alcohol Use Disorder” is posted
here.