Elevated Acyl-Ghrelin May Point to Those At High Risk of PTSD
Adolescents exposed to trauma who develop posttraumatic stress disorder (PTSD) appear to have higher levels of the stress hormone acyl-ghrelin than those who do not develop PTSD, according to a study in JAMA Network Open.
Researchers at Khyber Medical University in Pakistan and the Icahn School of Medicine at Mount Sinai in New York assessed blood and saliva samples taken from 88 adolescents in Pakistan. Forty-nine of the participants had been exposed to a terror attack that resulted in personal injury or the death of someone close to them about four years before the trial. The other 39 participants had no terror-associated losses or injuries.
All participants were evaluated using the civilian version of the PTSD CheckList (PCL-C). Thirty-five adolescents in the group exposed to trauma met the criteria for PTSD compared with none of the adolescents in the trauma-free group. Average PCL-C scores were 19.7 among trauma-free adolescents, 38.7 among trauma-exposed adolescents without PTSD, and 55.0 among trauma-exposed adolescents with PTSD. Corresponding average levels of blood acyl-ghrelin in these groups were 75.1 pg/ml, 61.4 pg/ml, and 166.1 pg/ml, respectively.
The researchers found that adolescents with elevated acyl-ghrelin levels were about eight times as likely to develop PTSD following trauma. Though trauma-exposed adolescents with PTSD on average also had elevated levels of salivary cortisol (another stress hormone) compared with the other two groups, cortisol levels were not significantly associated with PTSD risk.
“It is unknown whether the adolescents who experienced severe trauma without PTSD never displayed trauma-associated elevation of acyl-ghrelin or whether acyl-ghrelin decreased over time since the initial trauma,” the researchers wrote. “It is also of interest to determine whether obesity, which dysregulates acyl-ghrelin, alters the role of acyl-ghrelin in stress and trauma.”
Discharge MH Appointment Increases Likelihood of Follow-up Care
Hospitalized psychiatric patients who had received an outpatient mental health appointment as part of a discharge plan are more likely to attend outpatient mental health services than those without an appointment. These findings appeared in a report in Journal of Clinical Psychiatry.
“Scheduling follow-up outpatient mental health appointments is a low-resource activity that should be considered an important target for hospital continuous quality improvement initiatives to improve discharge planning and increase rates of successful care transitions,” wrote the investigators from Columbia University Vagelos College of Physicians and Surgeons and colleagues.
Some previous reports have shown the value of pre-discharge scheduling, but the studies were either conducted at one center and/or did not rigorously control for differences between patients who did and did not receive outpatient scheduling. To address this gap, the investigators used administrative data to examine 15,520 inpatient psychiatric discharges across the state of New York between 2012 and 2013.
Of this group, 77% of patients had an outpatient appointment scheduled with a mental health provider as part of their discharge plan. Compared with patients without an appointment, those with an appointment were 1.69 times more likely to attend a mental health appointment within seven days of discharge and 1.65 times as likely to attend within 30 days of discharge. Even among patients with a lower likelihood of attending post-discharge care (for example, patients who were homeless and/or with substance use disorders), scheduling an aftercare appointment significantly increased the odds of an outpatient mental health visit, the authors noted.
Researchers Uncover Neurons That Induce Dissociation
Investigators at Stanford University have uncovered a brain circuit that may regulate dissociation—the feeling of being detached from one’s thoughts and emotions. Dissociation is a symptom of several psychiatric disorders but can also be induced by drugs such as ketamine.
The investigators used ketamine to induce a dissociative-like state in mice and then took brain scans of the animals. They observed that the drug infusion caused a group of neurons in a region called the retrosplenial cortex to produce a rhythmic electrical signal at a frequency of 3 hertz, or three cycles per second. Next, they used a tool called optogenetics (in which neuron activity can be controlled with light energy) to stimulate the retrosplenial neurons to reproduce the 3 hertz rhythm in a separate group of mice and found this stimulation led to the dissociative-like state in these mice as well.
To test if these neurons were also involved in producing dissociative effects in people, the investigators recorded electrical signals from the brain of a patient who experienced dissociation prior to seizures (a condition known as epilepsy with auras). During the dissociative aura prior to each seizure, the researchers found nerve cells in the brain region that corresponds to the retrosplenial cortex of mice fired at 3 hertz. When the investigators applied electrical stimulation to this region, the patient experienced the dissociative aura without any seizures.
“Future clinical work could include the exploration of whether electrically induced low-frequency rhythms… [in] healthy humans can cause dissociative states, and whether dissociative drugs—or dissociation-linked neuropsychiatric states including posttraumatic stress disorder and borderline personality disorder—involve these rhythms in humans,” the investigators wrote.
The findings were published in Nature.
Fatty Acid Binding Protein May Be Autism Biomarker
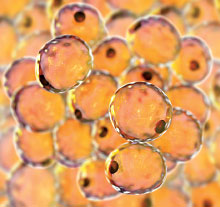
A protein called FABP4 (fatty acid binding protein 4) may help identify autism spectrum disorder (ASD) in young children, reports a study published in Brain Communications. The study was conducted by researchers at Japan’s RIKEN Center for Brain Science and colleagues.
The researchers hypothesized that FABP4, which chaperones fat molecules across different parts of a cell, might be involved in ASD since both low birth weight and obesity during infancy are considered risk factors for ASD. They analyzed the levels of FABP4 and other fat-related molecules from 102 children with ASD and 87 typically developing controls; the children were further divided into two subgroups: those aged 4 to 6 years and aged 7 to 12 years.
In the younger group, FABP4 levels were significantly lower in the children with ASD than typically developing controls. A follow-up analysis of samples from 21 children aged 2 to 4 with ASD and 25 typically developing controls produced similar results.
In contrast, FABP4 levels did not differ between the older group of children with ASD and their typically developing peers. Additionally, an analysis of postmortem brain tissue from people aged seven and older also revealed no differences in FABP4 expression between those with ASD and controls.
The fact that FABP4 levels only differed during an early stage of development suggests that altered FABP4 expression may not just be a byproduct of ASD, but perhaps a factor in the pathogenesis of this disorder, the researchers noted. ■