Researchers have composed a map of a brain circuit that may regulate manic behavior based on data from people who developed mania following a brain injury. This map can guide future research into bipolar disorder as well as help clinical investigators find new targets for therapies such as transcranial magnetic stimulation (TMS) to treat mania.
The findings, which were published in the Journal of Clinical Investigation, are the latest to showcase the potential of a technique known as lesion network mapping.
For decades researchers have attempted to pinpoint the origin of behavioral or cognitive problems in patients following damage to discrete regions in the brain. Before modern imaging tools became available, such lesion analysis provided valuable insight into traits such as language, learning, and memory. The study of H.M.—a man who was unable to develop short-term memories following a surgical procedure to alleviate seizures in the 1950s—is one of history’s most notable cases.
Still, lesion analysis has not provided definitive answers on where in the brain psychiatric symptoms originate.Accumulating patient data show that in many cases, damage to many seemingly unrelated brain regions can produce similar symptoms.
“What if it’s not the location of the lesion that’s important, but where that lesion is connected to in the vast neural highway?” asked Michael Fox, M.D., the director of the Center for Brain Circuit Therapeutics at Brigham and Women’s Hospital and an associate professor of neurology at Harvard Medical School.
It is a question that would have been difficult to answer in the past, but modern imaging tools including functional MRI (fMRI) have enabled researchers to construct wiring diagrams of brain activity, known as the human connectome. Such diagrams can be used to directly compare brain connections between people with and without a psychiatric disorder.
“Functional MRI comparisons can provide lots of [information on] correlations between bipolar symptoms and altered brain activity, but not causation,” he said. “A circuit with altered activity could be causing mania, but it could also be a compensatory response by the brain, or maybe even something unrelated.”
To determine the cause of mania, Fox proposed combining brain network mapping with the cause-and-effect data offered by symptom-inducing lesions.
In 2015, Fox and his lab first tested this approach—called lesion network analysis—using lesions that induced peduncular hallucinosis, a rare syndrome in which patients see vivid hallucinations in dark settings. They created a connectome map and then superimposed 23 lesions associated with peduncular hallucinosis on top. They found that 22 of the 23 lesions were part of brain circuits that shared the same node—a tiny region in the brain’s visual processing center.
The group has since developed lesion network maps for over 20 diverse symptoms.
For the current study, Fox, Albino Oliveira-Maia, M.D., Ph.D., of Portugal’s Champalimaud Research & Clinical Centre, and their teams collected scans of mania-inducing lesions from 56 different patients and mapped their connection profile relative to 569 lesions that did not lead to mania.
The mania lesions had little overlap in terms of physical location, though they were almost entirely on the brain’s right side (known to be associated with creativity). In terms of wiring, all the lesion locations were part of a large circuit that is associated with the brain’s limbic system—a center for memories and emotion regulation. More specifically, all the individual lesion maps were connected to three nodes in the right-front part of the brain.
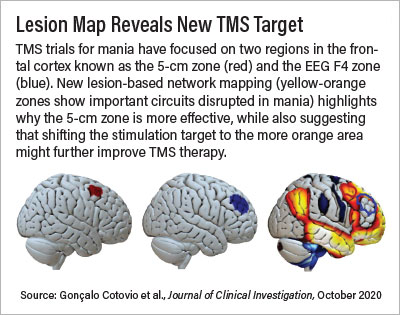
The findings reaffirm that current targets of TMS for mania are on the right track, Fox said. Studies suggest that stimulating the right-frontal region (the dorsolateral prefrontal cortex) may improve mania symptoms.
“The current target area is good, but our mapping suggests if you move the target a little more toward the midline of the brain, it might make it optimal,” Fox said.
Fox may not have to wait long to find out if his hunch is correct. Nolan Williams, M.D., an assistant professor of psychiatry at Stanford University and director of the Stanford Brain Stimulation Lab, was already preparing a clinical trial for TMS as a treatment for mania when he read Fox’s published findings. He quickly reached out to start a collaboration.
“Trying to stimulate someone with mania is difficult because their symptoms do not align optimally with conventional TMS methods,” Williams told Psychiatric News. In his forthcoming trial, Williams aims to overcome this difficulty by using a new approach he developed called SAINT, which provides short bursts of TMS over the course of several hours rather than one long stimulation that typically lasts 30 to 40 minutes. He is also enrolling patients with hypomania, which should reduce the potential of participants not completing their sessions due to their ongoing manic symptoms. Still, given the potential that the TMS stimulations may lack precision, it is important that the initial target be as optimal as possible, Williams said.
“That’s the beauty of Mike’s research,” said Williams, who has been a colleague of Fox’s for several years. “He’s a mapmaker who can tell you exactly which city [in the brain] you need to dial into for the best results.”
Fox noted his research has been made possible thanks to Harvard’s brain repository, which includes over 2,000 brains with focal lesions.
This study was supported by grants from the National Institutes of Health and Portugal’s Fundação para a Ciência e Tecnologia, with additional support from the Sidney R. Baer Jr. Foundation, the Nancy Lurie Marks Foundation, and the Mather’s Foundation. ■
“Mapping Mania Symptoms Based on Focal Brain Damage” is posted
here.