Combining clinical data from 68 separate studies, a research team has estimated the most effective dose for 19 different antipsychotic medications, including both oral and long-acting injectable (LAI) formulations. The researchers also calculated the dose equivalents of these 19 medications to guide physicians who may be considering switching patients from one antipsychotic to another. This meta-analysis was published in December 2019 in AJP in Advance.
The minimum and maximum effective doses of antipsychotic drugs are not well understood, wrote Stefan Leucht, M.D., of the Technical University of Munich and colleagues. Though approved medications are licensed within a specific range of doses, these amounts are usually calculated early in the drug development process and may not reflect the optimal range for patients.
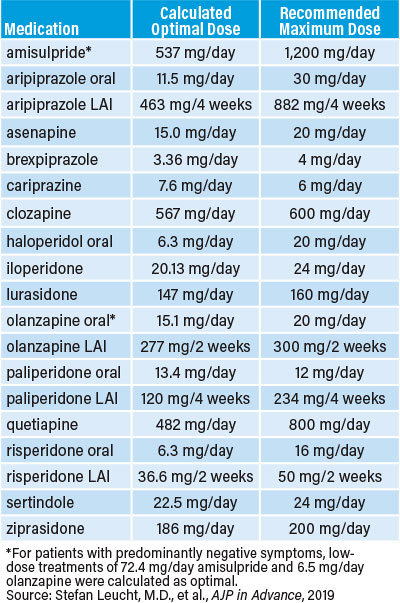
Leucht and colleagues identified clinical trials that compared multiple doses of the same antipsychotics relative to placebo in people with acute schizophrenia symptoms. They then calculated how well symptoms improved in those taking different doses of the following medications: amisulpride, aripiprazole (oral and LAI), asenapine, brexpiprazole, cariprazine, clozapine, haloperidol, iloperidone, lurasidone, olanzapine (oral and LAI), paliperidone (oral and LAI), quetiapine, risperidone (oral and LAI), sertindole, and ziprasidone.
he dose-response profiles for these 19 medications fell into two major classes. The first were antipsychotics whose effects plateaued or started dropping at higher tested doses, suggesting the optimal dose is within the currently licensed range. These medications included the following: amisulpride, oral and LAI aripiprazole, asenapine, brexpiprazole, cariprazine, haloperidol, oral olanzapine (when given to patients with predominantly negative symptoms), quetiapine, and oral and LAI risperidone.
In some instances, the most effective dose was well below the upper prescribing limits. For example, the most effective dose of oral risperidone—which is approved up to 16 mg/day—is 6.3 mg/day, according to the analysis.
“Clinicians often use relatively high doses of antipsychotics in practice,” Leucht told Psychiatric News. “Our analysis shows that for many antipsychotics such doses are not generally recommendable.”
For the other medications—including clozapine, iloperidone, lurasidone, oral olanzapine (in patients with predominantly positive symptoms), LAI olanzapine, oral and LAI paliperidone, sertindole, and ziprasidone—there was no indication that the dose-response was plateauing. The authors said that this finding suggests that doses above the licensed limit might be more effective.
Leucht cautioned that the dosing analysis considered only symptom improvements and that patients prescribed higher doses of these medications might experience worse side effects. Further controlled studies on dosing are needed to assess the risk-benefit profile of these antipsychotics at elevated doses, he said.
“Clinicians need to be aware that if they go beyond the officially licensed doses, they are applying the drug ‘off label’ and should be careful in this regard.”
Leucht also noted that the dose estimates for clozapine, haloperidol, LAI aripipazole, LAI olanzapine, and LAI risperidone were each based on a single dosing study, so the data should be interpreted with caution.
The researchers also calculated the dose equivalencies of the antipsychotics, using haloperidol, olanzapine, and risperidone as reference drugs (for example, 1 mg of risperidone = x amount of the other medications). These equivalencies can help physicians considering prescribing a different medication, but the researchers cautioned that physicians should look at the full profiles of each medication and not just rely on the conversion calculator. For example, 20 mg/day olanzapine corresponds to 8.25 mg/day risperidone, but an 8.25 mg/day dose of risperidone may be less effective than the optimal level of 6.3 mg/day.
“We stress that our results provide some guidance based on ‘average’ patients with chronic illness,” Leucht and colleagues wrote in the article. “The dose-response relationships in specific populations, such as first-episode patients, elderly patients (who need lower doses), and patients with treatment-resistant illness, are likely to be different.” Physicians should use these data as a starting point and then base individual dosing decisions on the properties of each medication, patient characteristics, and any other treatments that might influence antipsychotic response, they concluded.
The authors reported no funding information in the article. ■
“Dose-Response Meta-Analysis of Antipsychotic Drugs for Acute Schizophrenia” is posted
here.