Clozapine is considered the best option for people with treatment-resistant schizophrenia, but research has shown that this antipsychotic can also help people with aggression problems. A study appearing in the American Journal of Psychiatry now reports that clozapine may be especially effective at reducing aggression in patients with schizophrenia and co-occurring conduct disorder.
Conduct disorder, characterized by repetitive behaviors that violate other people’s rights, such as violence, theft, or property destruction, typically emerges in youth.
Menahem Krakowski, M.D., Ph.D., a research psychiatrist at the Nathan Kline Institute for Psychiatric Research in Orangeburg, N.Y., and colleagues examined data from 99 hospitalized schizophrenia patients aged 18 to 60. The study involved patients who were randomly assigned to receive clozapine, olanzapine, or haloperidol for 12 weeks. All participants had at least one clearly documented instance of verbal or physical aggression.
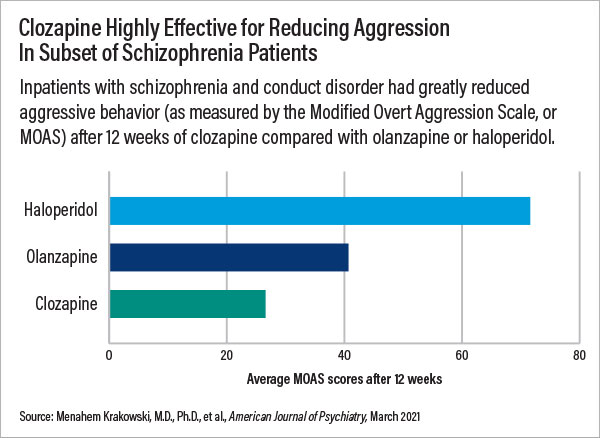
The researchers evaluated the patients’ aggression using the Modified Overt Aggression Scale (MOAS); this scale quantifies the number and severity of incidents involving verbal aggression, physical aggression against other people, and physical aggression against objects.
The researchers found that hospitalized patients with both schizophrenia and conduct disorder taking clozapine were nearly three times less likely to display aggressive behaviors than patients taking haloperidol. When specifically assessing physical aggression, clozapine was four times as effective as haloperidol.
The results also showed that clozapine was 1.5 times more effective than olanzapine at reducing any aggression, and about 1.7 times more effective at reducing physical aggression.
Krakowski told Psychiatric News he believes these findings should impact the clinical care of inpatients with schizophrenia: “Clinicians should do their best to identify the patient’s conduct history, and if conduct disorder is confirmed, they should seriously consider clozapine as the medication of choice.”
(APA’s recently revised Practice Guideline for the Treatment of Patients With Schizophrenia suggests that “patients with schizophrenia be treated with clozapine if the risk for aggressive behavior remains substantial despite other treatments.)
The findings in AJP were based on data collected in a clinical study that Krakowski ran from 1999 to 2004. The original study—which included 110 hospitalized adults with schizophrenia and documented instances of verbal or physical aggression—found that clozapine was about twice as effective as haloperidol and 1.3 times as effective as olanzapine at reducing any aggressive behaviors.
After several studies hinted that childhood conduct disorder may increase the risk of aggression, Krakowski decided to reexamine the data from the original trial to see if the presence of conduct disorder affected antipsychotic response.
Krakowski noted that other trials have explored how antipsychotics affect aggression or hostility, but these studies did not enroll patients based on their aggressive behaviors. “We were fortunate to get approval for a trial to specifically assess chronically ill patients with a documented history of problems,” he said. Given the challenges in conducting such studies, Krakowski and his team wanted to collect as much information as possible; they conducted exhaustive assessments and collected background information such as police reports to develop robust profiles of the participants.
After reviewing the patients’ historical information, Krakowski and colleagues were able to diagnose the presence or absence of childhood conduct disorder in 99 of the 110 patients from the original study: 53 with and 46 without conduct disorder.
During the 12-week study, the medication given significantly impacted the patients’ aggressive behaviors, but more so in patients with conduct disorder. Among patients with conduct disorder, average MOAS scores after 12 weeks were 71.6 in the haloperidol group, 40.7 in the olanzapine group, and 26.6 in the clozapine group. The average MOAS scores for patients with no conduct disorder who received haloperidol, olanzapine, and clozapine were 28.7, 24.9, and 15.0, respectively.
The improvements in schizophrenia symptoms were about the same in the patients with or without conduct disorder regardless of medication. “Thus, the reduced aggression in patients taking clozapine was not simply due to them experiencing fewer hallucinations or delusions,” Krakowski noted. He added that this finding was a little surprising, as numerous studies have shown clozapine is the most potent antipsychotic in terms of positive symptom improvement.
The current analysis and original clinical study were supported by grants from the National Institute of Mental Health. ■
“The Importance of Conduct Disorder in the Treatment of Violence in Schizophrenia: Efficacy of Clozapine Compared With Olanzapine and Haloperidol” is posted
here.
“Atypical Antipsychotic Agents in the Treatment of Violent Patients With Schizophrenia and Schizoaffective Disorder” is posted
here.
The American Psychiatric Association Practice Guideline for the Treatment of Patients With Schizophrenia, Third Edition, is posted
here.