One of the key questions in psychedelic medicine is quantifying how this class of drugs operates at the higher-order brain level. It is known that they activate serotonin 2A receptors, which eventually leads to states like increased empathy and out-of-body experiences. What happens in between?
As part of a wide-ranging talk on psychedelic neurobiology at this year’s Annual Meeting, Robin Carhart-Harris, Ph.D., the Ralph Metzner Distinguished Professor of Neurology and Psychiatry at the University of California, San Francisco (UCSF), postulated that psychedelics work by lowering a person’s confidence—but in a good way.
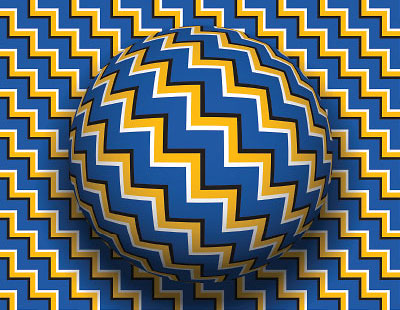
As Carhart-Harris, who is also the director of the Psychedelics Division at Neuroscape—UCSF’s new translational neuroscience center—explained, the brain creates a model of the world it inhabits based on prior experiences. This model is used to respond to stimuli, but at times the “priors” can conflict with the actual stimulus. Examples of this conflict are optical illusions that trick the brain into seeing motion that doesn’t exist.
Typically, the brain’s model of the world changes over time as new data keep pouring on. However, when some people are presented with new information that contradicts already held beliefs, the new information doesn’t penetrate. Carhart-Harris suggested this phenomenon, known as “canalization,” is a fundamental aspect of behavioral disorders. Canalization refers to the entrenchment of people’s models such that they resist new inputs. Indeed, most psychiatric illnesses have a component of cognitive or behavioral inflexibility: the self-defeating thoughts associated with depression, the cued fear responses associated with anxiety disorders, the repetitive behaviors of obsessive-compulsive disorders, to name a few. This may explain why psychedelic compounds have shown promise in the treatment of a wide range of disorders in preliminary studies—they can alter the brain’s precision weighting.
“Precision weighting is a measure of confidence assigned by the brain to these prior beliefs,” Carhart-Harris explained. The brain then builds its model world in a top-down manner, starting with the elements assigned with absolute certainty and moving on to elements with lower confidence.
Psychedelics disrupt that confidence such that the brain is forced to rely more on current stimuli and less on built-in beliefs, forcing the brain to build a model from the bottom up rather than top down. Carhart-Harris said it is akin to having your eyes closed for a while and then opening them in a new place.
This period of relaxed beliefs under psychedelics (or REBUS, as Carhart-Harris called it), is shaped by tremendous neural plasticity, effectively teeing up the brain for positive change via psychedelic-assisted psychotherapy.
But does opening this therapeutic window require patients to go on a “trip” and have all these mystical and spiritual experiences associated with psychedelics? A second psychedelic session hosted by Adrian Jacques Ambrose, M.D., M.P.H., and Michael Avissar, M.D., Ph.D., both assistant professors of psychiatry at Columbia University, discussed this question.
The idea that tripping is a critical element of the therapeutic process is one of the bedrocks of psychedelic medicine. Many human studies have validated this association, finding that participants who report more acute mystical experiences like a sense of being beyond time and space or feeling total tranquility tend to have better clinical responses, such as lowered depression or reduced drug cravings.
As Avissar pointed out, though, all this evidence is correlational and based on highly subjective measures of the psychedelic experience. No human work has shown these acute experiences are necessary for successful treatment.
Basic and translational research has suggested the opposite. Studies in rodents have firmly demonstrated that psychedelics can reduce fear in the animals even when the serotonin 2A receptor (the believed primary site of action for classic psychedelics) is being blocked by another compound. Other investigators have demonstrated that nonhallucinogenic analogs of psychedelic substances also exert beneficial effects in rodents.
But just as correlation is not causation, so too mice are not little humans, Avissar acknowledged. A head-to-head study in humans comparing an active psychedelic with an analog would seem ideal, but because of the pronounced effects of tripping, such a study cannot be blinded, and since subjects might have high expectations of receiving a psychedelic, the analog group could have skewed results. It might be possible to conduct separate experiments in which patients know what they are getting, but then objective biomarkers would be needed so results could be compared. Avissar noted that EEG readings might be a good biomarker since they are an affordable measure, are reproducible in individuals, and are direct reflections of brain activity.
Understanding the exact purpose of tripping has practical implications, Ambrose noted. The current model for psychedelic-assisted psychotherapy involves two therapists per patient and treatment sessions of up to eight hours. Being able to treat one patient a day is a significant barrier to access.
“We need to find out the core aspects of a psychedelic substance that must be preserved so it remains therapeutic but also scalable,” he said. ■