Although outpatients with major depressive disorder have a range of therapeutic options available, people who develop severe, treatment-resistant illness and require hospitalization have far fewer choices. For example, contrary to the entertainment industry’s depictions, only about 10% of inpatients with depression have access to electroconvulsive therapy (ECT), the gold standard of depression treatments. Fewer still have access to FDA-approved and highly effective treatments for depression such as transcranial magnetic stimulation (TMS).
Even if ECT and TMS devices were more readily available in inpatient settings, their use might be limited given that the average length of stay for psychiatric inpatients in the United States has shrunk to about 10 days. Both ECT and TMS require weeks of treatment for full effectiveness. The result of this paucity of treatment options is that many inpatients with major depression are caught in a revolving door of intake and discharge. Others—burdened by unrelenting suffering—die by suicide.
A new technology developed at Stanford University may fill this critical gap in inpatient care. Known as the Stanford Accelerated Intelligent Neuromodulation Therapy (SAINT), this technology makes use of a TMS protocol known as intermittent theta-burst stimulation (iTBS). iTBS, recently cleared by the FDA, can deliver therapeutic levels of magnetic stimulation in just three minutes, which is six to 10 times faster than conventional TMS. With these shortened treatment sessions, multiple treatments can be delivered each day. If these sessions are delivered at the optimal times, they will build on each other to amplify the antidepressant effect of the treatments. Based on studies of learning theory, we hypothesized that providing 10 sessions a day, 50 minutes apart, over five days would provide the best clinical outcomes.
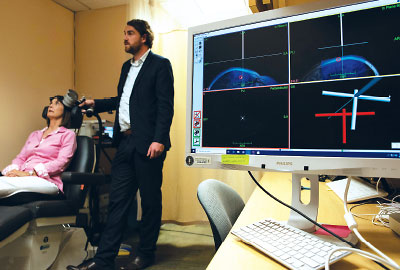
To enhance the therapy even further, each SAINT participant receives an eight-minute resting-state MRI scan to pinpoint the subregion within the left dorsolateral prefrontal cortex of the brain that would most likely respond to stimulation and relieve symptoms of depression.
The first open-label studies showed SAINT had rapid and robust effects in outpatients with treatment-resistant depression. Nineteen of the 21 participants who completed all 50 SAINT sessions achieved remission of their depression symptoms, and 60% remained in remission one month later. A follow-up randomized, controlled trial of SAINT in 30 outpatients has validated its antidepressant efficacy in outpatients. Seventy-eight percent of participants who received SAINT therapy achieved depression remission compared with 13% of participants who received a sham stimulation (see
related story).
Critically, we have completed some of our first inpatient assessments in a cohort of 12 adults with severe depression and demonstrated that SAINT can rapidly reduce depressive symptoms and suicidality in this population and maintain improvements over several weeks.
The suicidality findings are especially significant given the high risk of suicide among depressed individuals in the first 30 days following an inpatient discharge. Currently, there is no reliable method to predict which patients are at greatest risk of suicide, nor is there an intervention proven to reduce this risk prior to discharge (research has shown that regularly following up with patients after discharge can reduce suicidal behaviors). Nasal esketamine, which recently won FDA approval for treatment-resistant depression, is indicated for acute suicidality, but the effects last for only about 24 hours on average. Also, esketamine’s rapid-onset antidepressant effects are modest compared with those of SAINT. In our clinical studies, average patient scores on the Montgomery-Åsberg Depression Rating Scale (MADRS) dropped by 75% after five days; esketamine reduced MADRS scores by about 25% during the same time frame.
In addition to its rapid effects, high efficacy, and favorable safety profile, SAINT has the advantage of being easily staffed. Each daylong procedure can be overseen by a single trained technician, freeing up staff psychiatrists to manage other patients. In comparison, an ECT session typically requires an overseeing psychiatrist, an anesthesia provider, and one or more nurse assistants. In addition, although the time commitment over the five-day period required by SAINT requires individuals to take time off from work, this is not an issue for psychiatric inpatients.
Our group is in discussions with the FDA to market SAINT as a medical device. Although iTBS is already FDA approved, SAINT uses a different targeting, magnetic intensity, and dosing regimen than the cleared protocol. We have also received funding from the National Institutes of Health to start a randomized, controlled trial involving psychiatric inpatients who were admitted for acute suicidality.
Theta-burst stimulation is expensive, because in addition to the specialized magnetic device, a facility must also have a functional MRI for optimal therapy; however, I am confident that when factoring all the direct and indirect costs of inpatient psychiatric care, SAINT will prove cost-effective. This treatment can reduce the stay of most depressed patients to one week or less while minimizing relapse risk and future readmissions.
In the 1800s, asylums like the Salpêtrière in Paris were a model for providing humane long-term care to people with a range of neuropsychiatric maladies. As neurological science advanced over the next century, people with conditions like epilepsy or Parkinson’s disease began receiving disorder-specific care as outpatients instead of as residents of an asylum. A technology like SAINT might be the key to help inpatients with severe depression rapidly return to a life free from the symptoms of depression. ■
Disclosure Statement
Nolan Williams, M.D., is a named inventor on Stanford-owned intellectual property relating to accelerated TMS pulse pattern sequences and neuroimaging-based TMS targeting. He has served on scientific advisory boards for Otsuka, NeuraWell, Nooma, and Halo Neuroscience, and he has equity/stock options in Magnus Medical, NeuraWell, and Nooma.