Advocacy is the long game.
That was a message psychiatrist advocates delivered during an advocacy skills session at the annual meeting of the Academy of Consultation-Liaison Psychiatry in Miami on November 6.
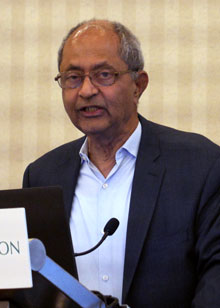
Moderated by past APA Trustee and former AMA President Patrice Harris, M.D., M.A., the session featured a panel of prominent APA members, including APA President Ramaswamy Viswanathan, M.D., Dr.Med.Sc., who shared their journeys and achievements as mental health advocates—sometimes realized after years or decades of work.
“We are in this for the long haul,” said past APA President Rebecca Brendel, M.D., J.D. who described her time as a law student at the University of Chicago in the 1990s working to pass a surrogate decision-making bill in Illinois. The
law passed in 1997, making Illinois just one of six states at the time with such a statute.
Passing a similar law in Brendel’s home state of Massachusetts has been an uphill struggle, one in which she is still engaged. “I’ve been to the state house now eight or nine years trying to get almost the very same bill passed,” said Brendel, associate professor of global health and psychiatry at Harvard Medical School and director of the Harvard Medical School Center for Bioethics. “Massachusetts is now one of the only states in the country that doesn’t have a surrogate decision-making bill.”
Speaking the day after the election of Donald Trump as president, panelists emphasized the need to adapt to new political realities. “Health and mental health are bipartisan issues,” Viswanathan said. “It doesn’t matter who is in power—we always find people on both sides of the aisle to work with.”
He reminded attendees that the Mental Health Parity and Addiction Equity Act was the result of years of advocacy by APA and other interested groups—and a bipartisan collaboration between Sen. Paul Wellstone, a Democrat from Minnesota, and Sen. Pete Domenici, a Republican from New Mexico. “It took a lot of effort and didn’t just happen overnight,” Viswanathan said.
Harris served as president of the AMA in 2019-2020, in the midst of the COVID-19 pandemic, and later chaired the AMA’s Opioid Task Force. She recalled that two decades ago New Mexico became the first state to pass a psychologist prescribing bill. When she and other members of the psychiatric delegation to the AMA later met with state lawmakers to learn how this had happened, they were told that psychiatrists had not made their opposition heard at the state and local levels.
Out of that experience grew the
AMA’s Scope of Practice Partnership, which brought together other specialties threatened by non-medical prescribing. “A lot of lessons learned,” Harris said. “Psychiatrists have to be involved in their state or county medical societies and work together at the AMA with the specialties that are most likely to be targeted with expanding scope of practice.”
Other speakers at the session included Michael J. Petersen, M.D., of the University of Wisconsin; Lee Tynes, M.D., chair of the APA Council on Healthcare Systems and Financing; Madeleine Becker, M.D., of the Marcus Institute of Integrative Medicine at Thomas Jefferson University Hospital; Kenneth Certa, M.D., also of Thomas Jefferson University Hospital; Anna Ratzliff, M.D., Ph.D., of the University of Washington; Myo Thwin Myint, M.D., of Tulane University; and Kristin Kroeger, APA’s chief of advocacy, policy and practice advancement.
For further reporting from the ACLP annual meeting, see upcoming editions of Psychiatric News. ■