Worldwide, suicide is one of the three leading causes of death among 15- to 44-year-olds. It is responsible for nearly half of all violent deaths and accounts for one million fatalities every year. Men outnumber women 4 to 1 in this regard. Moreover, there are 20 times as many suicide attempts as suicide completions (
1–3).
Mental disorder is a key correlate of suicide. Its prevalence has been evaluated at 80% to 100% among suicide completers (
4,
5). The most common diagnoses of completers include depression, substance abuse, personality disorder, and a substance use disorder that is comorbid with a mental disorder (
6,
7). Lifetime risk of suicide has been estimated at 3% to 4% among people with a common mental disorder such as depression (
8,
9) and at 4% to 5% among those with a severe and persistent mental disorder such as schizophrenia (
10–
12).
Because previous suicide attempts are another key correlate of suicide (
1,
2), health care systems can play a major role in suicide prevention (
13). Indeed, contacts with services are common in the year preceding suicide. A systematic review of suicide cases showed that although nearly 78% of completers had made at least one visit to a general practitioner, only about 32% had seen a mental health professional (
14). Similar but lower figures were reported for young adult completers in Quebec in the early 1990s (
15). Access to general practitioners is widespread in the publicly managed Canadian health care system. In 2006, 75% of the general population made at least one visit to a general practitioner (
16). Among these service users, one in five was diagnosed as having a mental disorder (
17). However, although contacts with services are common, few suicide completers seem to engage in adequate treatment (
14,
18). Moreover, poor coordination between primary care services, specialized medical services, and addiction services is a barrier to suicide prevention (
14).
Although research has identified predisposing factors in service utilization, few studies have focused on mental health service use in suicidal populations. Clinical guidelines recommend that individuals with a severe mental disorder such as schizophrenia should be in the care of specialized services (
19) and that those with a common mental disorder such as depression should be treated by primary care services, with more complex cases in shared care with specialized services (
20). These patterns of mental health-related service use were observed in Montreal in the general population (
21), but it is not known whether these patterns apply also to the population of hospitalized suicide attempters. Higher rates of contact with services have been observed among women compared with men, older adults compared with youths, and self-poisoners compared with those who attempt suicide by other means (
18,
22,
23). However, individuals with a substance use disorder tend to show lower rates of contact with services (
24–
26). Previous studies have examined contacts with services mostly in the general population or among suicide completers. Little attention has been paid to suicide attempters with specific common or severe mental disorders.
Against this backdrop, we sought to analyze patterns of mental health-related service utilization among persons with a severe mental disorder (schizophrenia) or a common mental disorder (depression) who were hospitalized in Montreal after attempting suicide. Our objectives were threefold: to compare profiles of service use between the two diagnostic groups in the 12 months before attempt, to identify factors influencing postattempt contact with services, and to compare diagnostic groups in terms of contact with services three months pre- and postattempt, with a particular focus on service utilization at the levels of primary care and specialized medicine.
Methods
Study design and data sources
The sampling frame for this retrospective cohort study consisted of the 1.8 million residents of Montreal, Canada's second largest city, located in the province of Quebec. As in the rest of Canada, the health and social services system in Quebec is publicly funded and offers citizens universal access to medically required care, hospital emergency services, hospitalization, outpatient general and specialized care, and general practitioners' clinics. There are no private hospitals. In addition, in Quebec, psychosocial services are available in local community health centers (CLSCs); these are considered primary care services, as are general practitioners' clinics. Thirteen different general hospitals and four specialized psychiatric hospitals are available to treat suicide attempters in Montreal. Individuals who visited hospital emergency departments and were treated on site without being hospitalized were not considered in this study.
Of all the Montrealers 15 years old or older diagnosed by a physician as having schizophrenia or depression during the study period (April 2002 to March 2005), 525 were hospitalized for attempting suicide and discharged during the index period (April 2003 to December 2004). If an individual was hospitalized more than once for attempting suicide during the index period, the first event was considered and designated as the index attempt.
Data were retrieved from the linked administrative databases of Montreal's Health and Social Services Agency. Corresponding data from the public sector were previously retrieved from Quebec's physician compensation database (RAMQ), the Quebec hospitalization discharge database (MED-ECHO), and the CLSC interventions database (I-CLSC). Medical insurance numbers were used to link data for a given individual from one database to another. These were available only for individuals in the Montreal area because the system had yet to be implemented in the rest of the province. The agency was granted permission by the Quebec Data Privacy Commission to use the data for service planning and research purposes. The medical insurance numbers were encrypted to ensure confidentiality. The study was approved by the Ethics Board of the Faculty of Medicine of the University of Montreal.
Measures
Mental health-related contact with services in the three months postattempt was the primary outcome investigated. This was defined as contact with any health care or psychosocial resource for mental health reasons (at least one contact versus none). Mental health-related contact with services in the three months preceding the attempt was defined similarly to the definition for the dependent variable (at least one contact versus none). Profiles of service use in the 12 months before the attempt were defined and classified hierarchically according to one of five levels of treatment settings, listed in ascending order (
21): general practitioners' clinics, hospital emergency services, CLSC, psychiatric outpatient care, and psychiatric inpatient care (hospitalization). Although profiles could include services obtained at more than one level, they were classified according to the highest level reached. Other independent variables included primary clinical diagnosis (schizophrenia versus depression), comorbid substance use disorder (yes versus no), method of attempt (self-poisoning versus other), sex (female versus male), and age.
Clinical diagnoses were classified according to the ICD-9: schizophrenia, codes 295.0–295.9, 297.0–297.9, and 298.0–298.9; depression, 296.1, 296.3, 300.4, and 311.0–311.9; and substance use disorders, 291.0–291.9, 292.0–292.9, 303.0–303.9, 304.0–304.9, and 305.0–305.9. Given that dual diagnoses were possible according to primary diagnosis (schizophrenia or depression, plus a secondary diagnosis of a substance use disorder), we applied a hierarchical algorithm to ensure that schizophrenia did not preclude depression but that depression precluded schizophrenia. We selected cases of hospitalized suicide attempters on the basis of self-inflicted external cause of injury E-codes (self-poisoning, E950–E952, versus other causes, E953–E959).
Statistical analysis
Chi square tests were carried out to compare service use profiles between the two diagnostic groups (schizophrenia versus depression) and mental health care contacts pre- and postattempt. Backward logistic regression analyses were conducted in order to predict at least one mental health-related contact with services in the three months postattempt after taking into account all previously defined independent variables. Interactions were tested. Only statistically significant variables were kept in the final model. The significance level was set at .05. The analyses were carried out with SPSS, version 15.
Results
Population characteristics
In this cohort of hospitalized suicide attempters (N=525) in Montreal who were discharged from a hospital during the 18-month index period, 330 (63%) were diagnosed as having depression and 195 (37%) as having schizophrenia, 281 (54%) were female and 244 (46%) were male, and the mean±SD age was 42.9±17.3 years. More than half of the cohort (N=329, 63%) had a concurrent substance use disorder. These characteristics did not differ significantly between the two diagnostic groups. Self-poisoning was more common in the depression group (N=257, 78%) than in the schizophrenia group (N=130, 67%, p=.005). Other methods of attempting suicide included cutting (9% versus 17%, respectively, for the depression and schizophrenia groups), leaping from great heights (2% versus 7%), hanging (4% versus 2%), and other (6% versus 7%). There was no statistically significant sex difference in terms of methods used. The mean length of the hospital stay for the index attempt was 17.4±30.7 days for the entire cohort, 23.3±36.1 days for the schizophrenia group, and 13.8±26.4 days for the depression group (p=.001).
Mental health care contacts
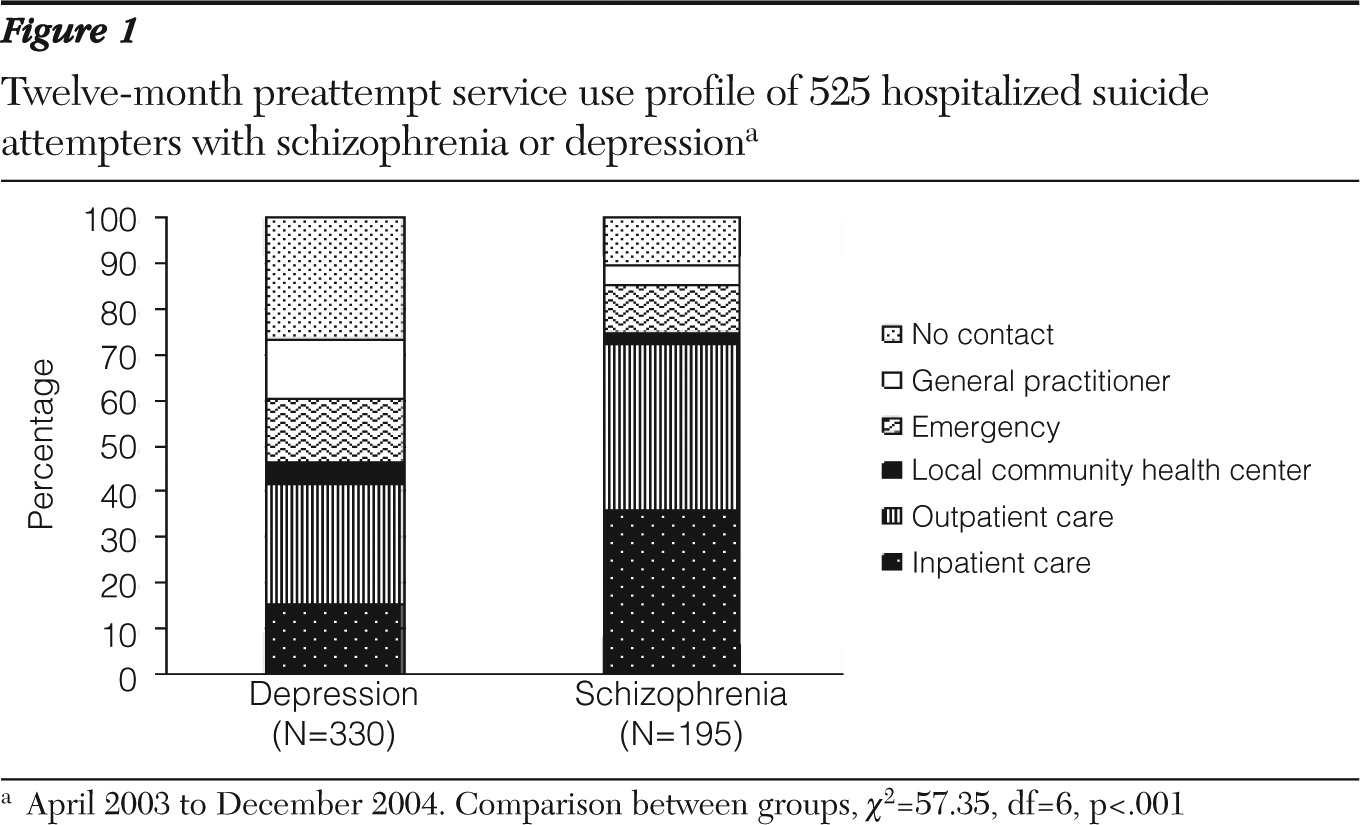
Figure 1 illustrates the relationship between the diagnoses of schizophrenia and depression and service use profiles. Clearly, the profiles were statistically different between the two groups in the 12 months preceding the suicide attempt. Whereas both groups were in contact mostly with specialized services, persons in the depression group had lower rates of contact with services than those in the schizophrenia group.
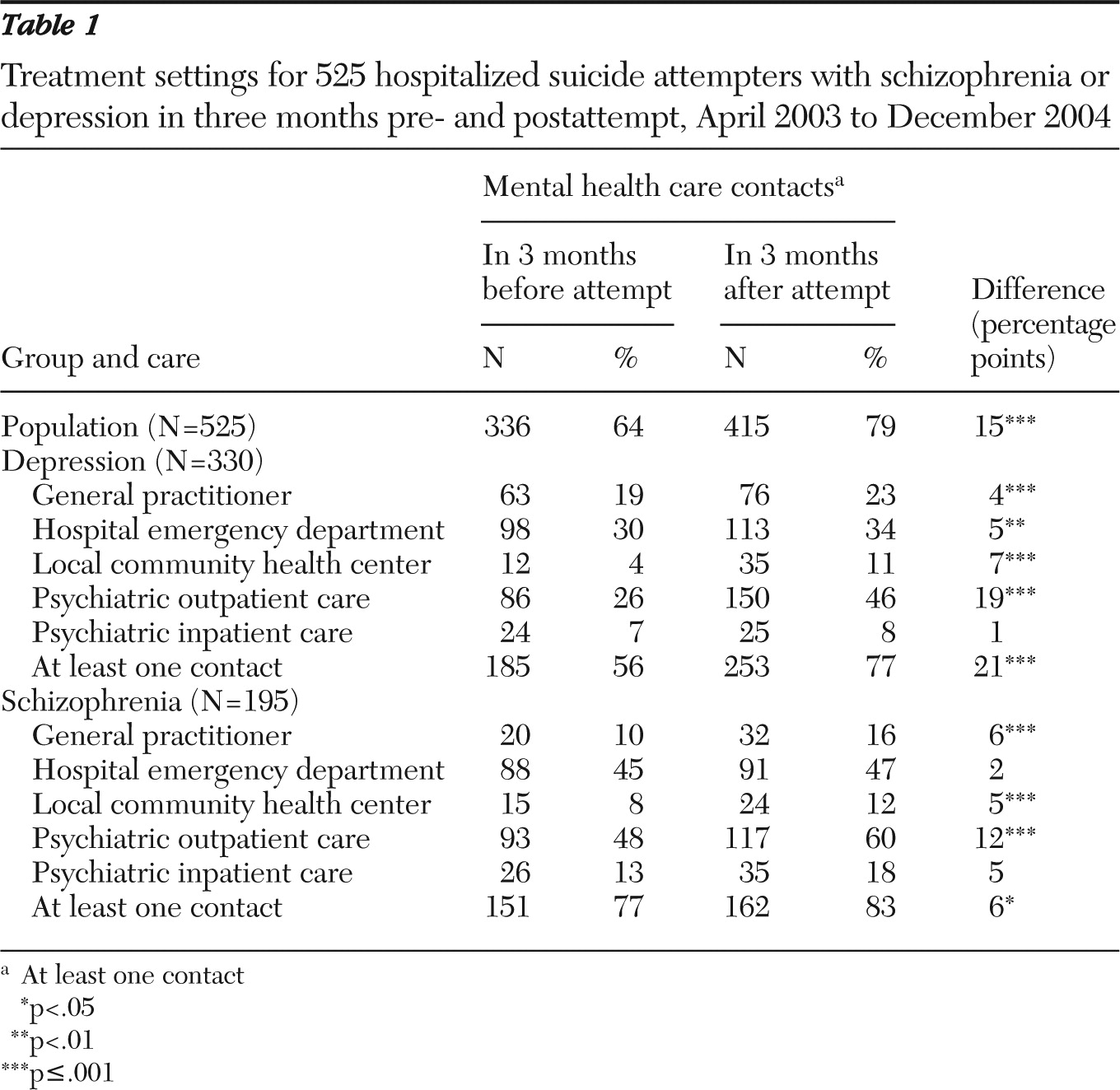
Table 1 indicates contact with various services for mental health reasons in the three months pre- and postattempt. In both groups, aftercare was provided mainly by psychiatric outpatient clinics. The rate of contact for the depression group was 20% higher before and after the attempt. Although rates of contact with services were higher in the schizophrenia group than in the depression group, the increasing rates of contact with services was higher in the depression group than in the schizophrenia group (21% versus 6%).
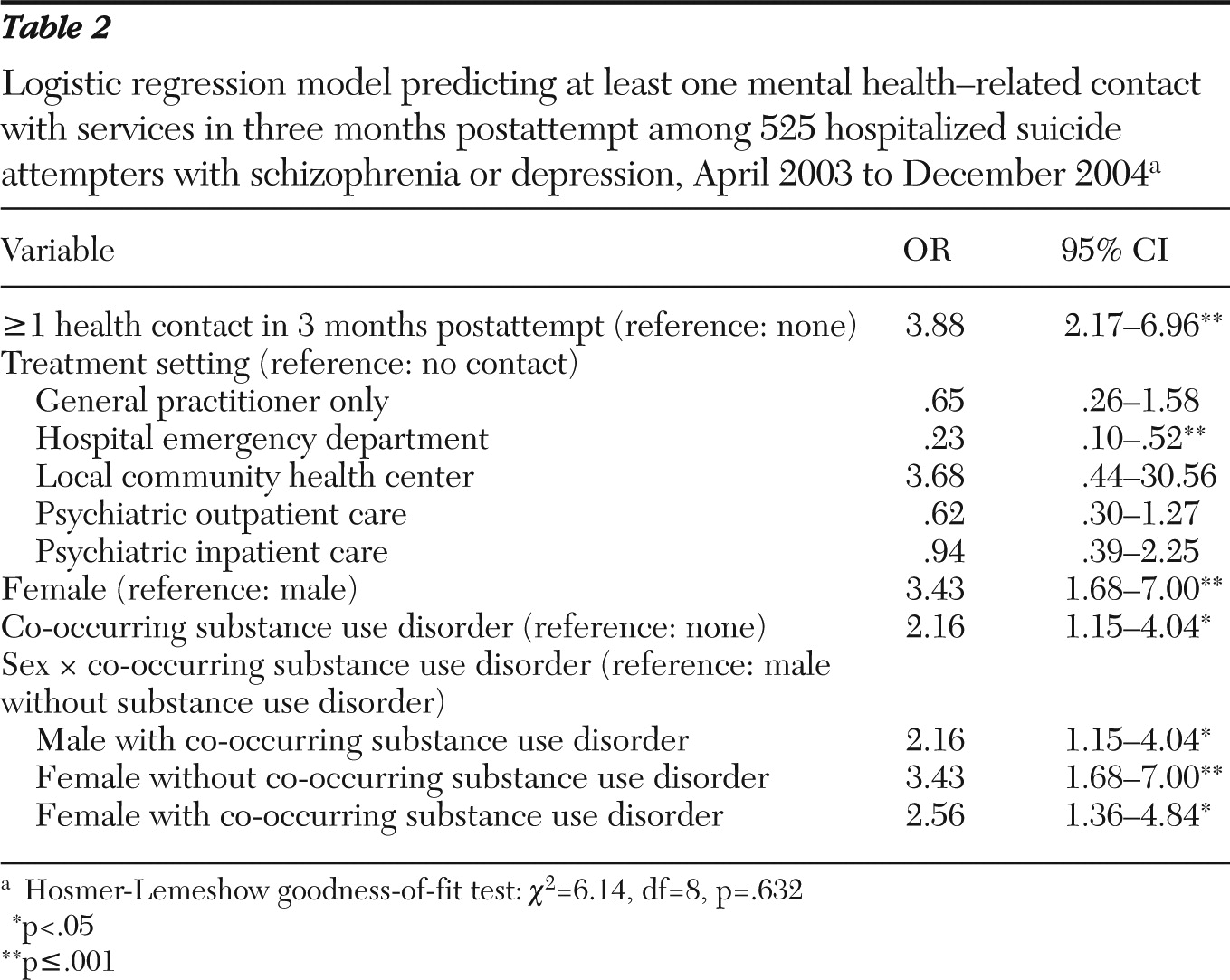
Factors predicting contact with services for mental health reasons in the three months after the attempt are shown in
Table 2. In our sample, primary diagnosis (depression or schizophrenia), age, and method of attempt were not associated with aftercare, unlike other characteristics identified (data not shown). An interaction between sex and a co-occurring substance use disorder was found, meaning that the effect of substance use disorder on the likelihood of aftercare differed between males and females. For males, having a substance use disorder in addition to schizophrenia or depression increased the likelihood of receiving aftercare; no such effect was found for females.
Discussion
Our results show that hospitalized suicide attempters with schizophrenia or depression differed in terms of mental health-related service use profile before the attempt. Although our study design did not involve a control group, we compared our findings with those obtained by the Montreal Health and Social Services Agency, which observed similar service use profiles in the general population (
21). Its study was conducted within a time frame similar to ours and used the same linked databases. The results of that study showed that the schizophrenia group was in contact mostly with specialized services (outpatient, 69%; inpatient, 22%) and that 50% of the depression group was in contact only with general practitioners. However, we found that hospitalized suicide attempters in both diagnostic groups were more likely to be in contact with specialized services, although one-fifth had no contact with mental health-related services in the 12 months before the attempt. Consistent with our results, data regarding Finland's publicly managed health care system has indicated that suicide attempters with diagnoses similar to those in our groups and treated in hospital emergency departments also were in contact mostly with specialized services in the year preceding the attempt (
27).
Consistent with other studies, our results showed a significant increase in contact with services for mental health reasons after attempted suicide (
23,
27). Indeed, a majority of our sample had at least one contact with services in the three months before and after the attempt; aftercare was provided mostly by specialized services or hospital emergency departments in both groups. Moreover, individuals with depression seemed to increase their contacts before hospitalization at the same rate as individuals with schizophrenia. However, a lack of service utilization pre- and postattempt was observed in both groups. Even during the three-month period after hospitalization, 23% of the depression group and 17% of the schizophrenia group still had no contact with services.
Our findings corroborate prior studies that established that previous contact with services was likely to facilitate aftercare (
24,
28). However, unlike the study by Suominen and colleagues (
24) in Finland, our study did not include individuals treated only in hospital emergency departments and not later hospitalized. We considered only the most severe cases of suicide attempt.
Only one of our service utilization profiles emerged as significant. Hospitalized suicide attempters with a previous pattern of using only hospital emergency services were less likely to contact services after their discharge. In line with past studies, our research revealed high rates of concurrent mental disorder and substance use disorder among suicide attempters (
14,
27,
29). Our data also point to specific sex differences associated with co-occurring addictive disorders. The interaction found indicates that men with co-occurring disorders were more likely than men without them to resort to services after attempting suicide. These results converge in part with previous findings showing higher treatment rates among individuals with co-occurring mental and addictive disorders than among those with one or the other (
26,
30,
31). In our study, we found that having a co-occurring substance use disorder increased the likelihood of receiving aftercare for males but not for females. Indeed, with or without a co-occurring substance use disorder, females were still more likely than males to seek mental health-related aftercare. Our results for males contrast with those of other studies that revealed that addictive disorders tended to decrease the likelihood of active and adequate aftercare among suicidal individuals (
14,
32,
33). Regardless of these differences, in our study, a primary diagnosis of depression or schizophrenia, age, and method of suicide attempt did not seem to play a major role in whether an attempter received aftercare.
Improving mental health care services
The increased likelihood of postattempt contact with services, particularly for males with a substance use disorder, is a positive indicator of adequacy of care for hospitalized suicide attempters. The distinct sex difference to emerge from our findings may be a result of regional efforts to ensure continuity of aftercare, including one protocol involving suicide prevention centers and hospital emergency services (
34). These protocols recommend that special attention be paid to men with a substance use disorder, because they are recognized as a high-risk group and are often reluctant to engage in treatment.
Experts argue that a multidisciplinary approach to patient assessment and management, which includes the involvement of a psychiatrist in the evaluation, is the best approach for helping persons who attempt suicide (
19,
35,
36). The authors of a recent audit conducted in the province of New Brunswick concluded that better accounting for behavior related to substance use should be one of the primary goals of a Canadian nationwide suicide prevention strategy (
14,
37). They added that early treatment of addiction and mental disorder, a more concerted effort on the part of specialized mental health and addiction services, and greater access to these services were needed in order to improve suicide prevention.
Our results show certain subgroups of attempters to be less likely to access or remain in contact with services. This finding is cause for concern in that suicide risk is particularly high soon after hospital discharge (
9,
38,
39). Earlier studies pointed out that poor treatment compliance increased suicide risk (
40). Finnish researchers suggested that referral to aftercare was the key factor affecting treatment contact after a suicide attempt (
27). Our findings indicate that a greater effort should be made to improve the continuity of care for men with common and severe mental disorders and for individuals with a service use profile centered exclusively on hospital emergency care. In this regard, quality and continuity of services dispensed in hospital emergency departments have been criticized (
41). A previous study determined that 14% of patients treated for attempting suicide were discharged without receiving any aftercare recommendations (
42). Still, hospital emergency services have a crucial role as a gateway to mental health services for patients at risk of suicide. Improvement is needed especially where coordination is concerned in order to enhance continuity of care.
Strengths and limitations
A key strength of our study is that the linked administrative databases used were those of an entirely publicly managed care system with access to data for all Montreal citizens. This allowed us to draw service utilization profiles according to the different levels of service available in care settings. Unfortunately, these databases do not document the nature of the services used and contacts with publicly funded health care service providers, such as mental health professionals in outpatient clinics, addiction services, and nongovernmental agencies or with privately funded psychologists (
14). For example, it has been reported that 3% of the Quebec population consults a private-practice psychologist in a given year (
43). Consequently, the rates of mental health aftercare are likely to be underestimated.
Our study reinforces the position that databases that allow linking of records are a valuable tool in the study of health care and public health policies (
44–
46). However, this source of data is subject to a recording bias. In order to minimize this limitation, we used broad categories of mental disorders instead of specific diagnoses because the validity of broad classifications, such as nonaffective psychotic disorders or depressive disorders, in administrative databases has been demonstrated across jurisdictions, over time, and in patterns of service utilization (
44).
The generalizability of our findings is limited to the most severe cases of attempted suicide—that is, those warranting hospitalization. We chose not to include attempters seen in emergency departments but not hospitalized because Montreal's hospital emergency room administrative databases have shown inconsistencies in how suicide attempts are documented (
47). The generalizability of our findings is limited also by the differences in health care systems between countries, although the characteristics of suicide attempters treated in hospitals in New Zealand and Finland are similar to those of our hospitalized attempters (
27,
29).
Conclusions
The publicly managed health and social services system in Montreal seems to respond relatively well to the needs of hospitalized suicide attempters, including men with a comorbid substance use disorder who are known to be at high risk of suicide. Specialized outpatient care and hospital emergency departments were the services most used before and after the attempt both by individuals with schizophrenia and by those with depression. However, the fact that a relatively large proportion of suicide attempters received no recognized aftercare is cause for concern. In this regard, efforts must be made to improve access to services for individuals who utilize only hospital emergency services. To this end, better coordination is needed among primary care services, specialized mental health services, and addiction services in order to enhance continuity of care.
Acknowledgments and disclosures
Ms. Routhier was supported by a fellowships from the Fonds de recherche en santé du Québec to the Groupe Interuniversitaire de Recherche sur les urgences and from the Centre de Santé et de Services sociaux Bordeaux-Cartierville-Saint-Laurent-affiliated University Center.
The authors report no competing interests.