The mental health needs of court-involved youths have been well documented. High rates of mood disorders, anxiety disorders, and behavioral disorders make the need for mental health interventions the norm, rather than the exception, in this population (
1–
3). Yet high levels of need do not translate into high levels of mental health service utilization for these youths (
4–
7). Although mental health interventions for delinquent youths are known to reduce symptoms, improve functioning, and prevent recidivism (
8,
9), less is known about systems of collaboration between juvenile justice agencies and mental health service systems to increase access to treatment and to strengthen treatment effects.
Juvenile probation officers provide direct supervision and services to over 60% of all youths referred to the juvenile court (
10). These justice personnel are the point of contact for most interagency collaboration involving delinquent youths and are responsible for exercising court authority to hold youths accountable for their cooperation with court mandates. Given the central role of probation officers in the management of delinquent youths with mental health problems, the lack of understanding about how these officers conceptualize interagency collaboration on behalf of these youths is a substantial gap in the current literature.
This study sought to examine the interagency collaboration strategies that juvenile probation officers use in their supervision of clients with mental health problems. A conceptual model of collaboration was developed on the basis of a qualitative analysis of 31 digitally recorded telephone interviews with probation officers. Results of the study provide a conceptual framework to guide future research into collaboration strategies for working with juvenile offenders who have a mental illness.
Methods
Participants were juvenile probation officers recruited from a pool of respondents who completed an online survey in 2008 about probation strategies (
11,
12). Of 308 survey respondents, 206 indicated their willingness to participate in a follow-up study. The list of probation officers willing to be recontacted was sorted randomly with a random-number generator. Probation officers were contacted via e-mail, with a second contact attempted for nonresponders. Those who expressed willingness to participate were scheduled for telephone interviews. A target sample of 30 probation officers was sought to ensure saturation in the main study aims. In total, 110 officers were contacted, 14 e-mail messages were returned as undeliverable, and 31 officers were recruited and interviewed.
The university institutional review board approved all recruitment procedures and approved verbal consent procedures, which were recorded on interview transcripts. Interviews followed a semistructured format. After giving verbal informed consent, officers were asked to identify a youth on their caseload whom they considered at high risk of recidivism and who was known to have mental health problems, to describe the youth’s case-plan goals, and to describe an intervention or probation strategy that officers would judge to have led to progress on their case-plan goals. Throughout the interviews, participants were prompted to provide behavioral descriptions where possible (for example, “If I was to watch you clarifying your role as a probation officer, what would I see you do?”) and to describe specific linkages between probation strategies and outcomes (such as, “When you ask open-ended questions about a youth’s long-term goals, what should change for the youth?”). Because detailed data were collected about specific youths on participants’ caseloads, geographic data about the officers (specifically, county or state of employment) were not collected in order to preserve officer and youth confidentiality.
A grounded-theory approach using open coding and constant comparison was used throughout the study (
13,
14). During interviews, memos were developed to track investigator interpretations, questions, and hypotheses. Follow-up questions to respondents were used to elaborate hypotheses generated in earlier interviews in a constant comparison approach. During the analysis, an open coding strategy was used to generate themes and categories about how probation officers described their approach to collaboration.
Results
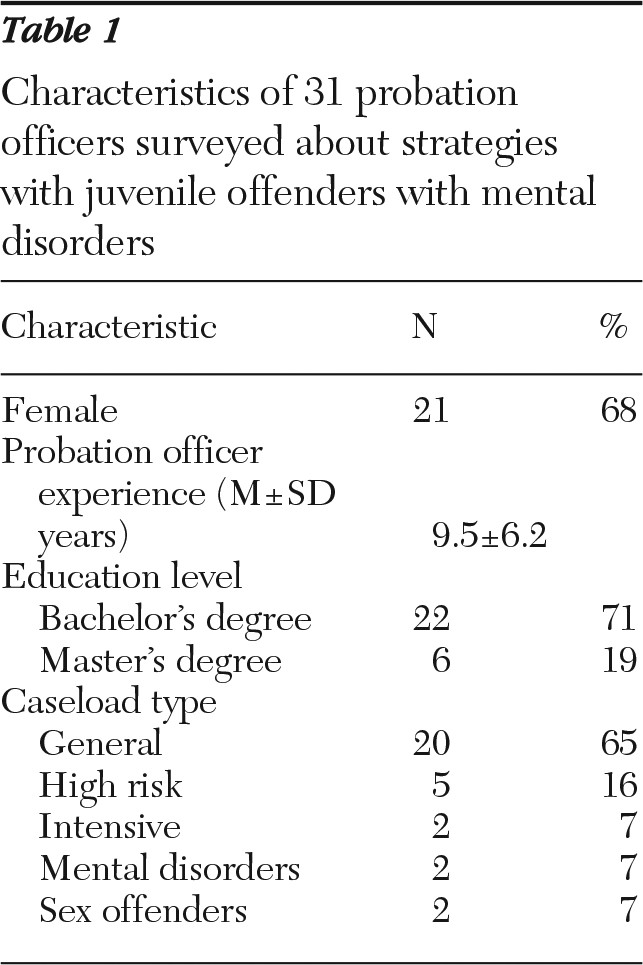
Characteristics of participants are shown in
Table 1. All participants endorsed collaboration with service providers as an essential element of their supervision of youths with mental health problems. Collaboration was used to hold youths accountable for their actions and to sustain their ongoing involvement in mental health treatment. On the basis of an analysis of themes reported by probation officers, three distinct collaboration models were identified: monitoring, teamwork, and partnership.
Officers who used a monitoring collaboration approach (N=7) reported only limited contact with mental health service providers. In such cases, contact was limited to providing information at referral (for example, “And so even though I’m not getting information back as to what’s happening in therapy, I give as much information as I could to the therapist so that they, they know what . . . we’d like to see happen”) and monitoring attendance through monthly contacts, which are often conducted via e-mail or other written form. Direct contact by the probation officer with the provider takes place as needed in this collaboration model. Confidentiality of the therapist-client relationship was the justification for the monitoring model (one officer stated, “We don’t have a lot of phone conversation, because a lot of that is confidential on their part, because it’s related to HIPAA, but they will always give us a written report that gives us sort of a generic thing of, are they attending and are they making progress?”)
Most officers (N=21; 68%) described a teamwork model of collaboration based on interdisciplinary and interagency case planning and problem solving. For example, an interagency team approach involving probation, individual therapists, and law enforcement ensured hospitalization rather than detention for a 17-year-old boy who had problems with post-traumatic stress disorder and a possible personality disorder. Teamwork models of collaboration occurred when formal team meetings were held as well as when probation officers and other treatment professionals regularly discussed cases and their management (“If she had a concern, she’d call me and say, ‘Hey, um, I’m real concerned with this kiddo”). Among the benefits of teamwork shared by officers were more highly coordinated services and shared brainstorming of ideas for difficult cases. In addition, the teamwork approach augmented probation authority (for example, “You give her an inch she’ll take a yard. So, having so many people around paying attention and following up, she needs to know that that’s [detention placement] possible”). Treatment teams increased the capacity for case monitoring, reduced splitting behaviors by the youth and family, and strengthened the rationale for case goals that were imposed on clients when they disagreed with treatment needs.
Several officers (N=6; 19%) also described a partnership model of collaboration involving their direct involvement with service providers in the treatment process, including their attending treatment sessions. In addition to the benefits associated with the teamwork approach, officers who described a partnership approach became adjuncts to the therapy process, facilitating generalization of treatment effects such as skill acquisition.
For instance, a female officer with six years of experience routinely observes an evidence-based program called Aggression Replacement Training (ART), which is available to youths on her caseload. Because of her intimate knowledge of the program, she was able to help a 16-year-old male client with serious substance use problems apply skills learned in ART to real-world situations (she reported, “I engage him in a conversation about that. . . . ‘you know, have, have you been able to use that in a situation?’ ”).
The distinguishing feature of probation-provider partnership is the presence of the officer during treatment affording the officer an opportunity to learn about the specific treatment models used with the client. In addition to acting as an adjunct to the treatment process, treatment partnerships increased officers’ insight into their cases (“I’m really just sitting back and listening and . . . taking in the dialog”), gave immediate feedback to clinicians about probation-related consequences for client behaviors (such as, “There might be a question that the therapist may ask me like, oh, you know, ‘If you continue to do this, is this what’s gonna happen with her probation?’ And, so then I can confirm with the therapist that, yes, that’s what’s gonna happen”), and provided guidance to officers about their use of authority (such as, “And it also helps me, with the therapist, . . . what does he recommend that I do to still hold her accountable but make sure that we don’t spin out of control into a crisis”).
Across all interviews, teamwork collaboration strategies were the norm, but results suggested that agency structural factors contributed to departures from the teamwork norm. For instance, officers with caseloads of greater than 50 cases typically reported using a monitoring strategy. Officers from agencies that provided in-house psychosocial services or specialized probation programs dedicated to mental health or substance abuse were more likely to use partnership strategies (“[Probation] is more of the enforcement, . . . but our officers are also very treatment-oriented. . . . [T]hey’re comfortable saying ‘Emily, I see that you’re going on some tough times. . . . [M]aybe we can talk to the clinician and find out what’s going on’”). Probation supervisors were also pivotal to the partnership strategy, encouraging officers to participate in the treatment process on a case-by-case basis (“And my boss actually has been encouraging me.” “He used to supervise adult offenders, and he said, ‘I used to go sit in on their groups all the time.’ ”).
Discussion
Probation officers generally valued interagency collaboration and its benefits. The teamwork and partnership models, in particular, promoted service coordination and collaborative problem solving. These approaches extended the authority of probation by expanding surveillance through joint monitoring. The teamwork and partnership models diverged to the extent that probation officers were invited into the inner sanctum of mental health interventions. Whereas the teamwork model preserved a strong boundary between the probation and treatment roles, the partnership model blurred the boundary and increased the engagement of probation officers with the treatment process. Indeed, this degree of cooperation conditioned officers to interact with clients in a manner that specifically reinforced treatment effects and aligned their case-monitoring activities with the needs of the youth in support of his or her mental health.
Probation officers shoulder the task of exercising authority on behalf of the juvenile court. However, because authority can have dramatic clinical implications, mental health service providers have a stake in how probation officers exercise this important aspect of their role. Working together, mental health professionals and probation officers can maximize the client’s having a say in and participating in the case-planning process and can plan the style of treatment pressures needed to maximize the clinical benefits of mental health intervention. But this level of collaboration implies that mental health professionals and probation officers are indeed working together, which is not likely to be seen in the monitoring approach described by some officers. Rather, consultation and leadership will be most likely when mental health professionals collaborate with probation officers in either a teamwork or partnership approach, with the latter perhaps providing the greatest depth of influence.
Among study limitations, three stand out and leave open possibilities for future research. First, within and between officers, factors and case characteristics that might explain variation in collaboration strategies were not deeply examined in the transcripts. There are hints that the partnership model was case dependent in at least a few instances, but this was not probed, nor were links between collaboration and officer attitudes, biases, and professional training made explicit. Second, the relative effectiveness of the collaboration models cannot be assumed by these study findings. To be sure, officers who endorsed a partnership strategy, and many who endorsed teamwork approaches, were highly enthusiastic about the specific benefits of collaboration. However, it is likely that the relative effectiveness of the collaboration models is at least somewhat dependent on case characteristics, including general risk level and specific diagnostic considerations. Therefore, justification for officer enthusiasm awaits additional empirical analyses with larger, more representative samples. Finally, sample selection necessarily excluded the perspectives of mental health providers who collaborate with probation. Whereas probation officers who endorsed the partnership strategy described its benefits, the impact of close partnership on the clinical processes between mental health providers and their clients awaits closer scrutiny.
Conclusions
This study introduced a practitioner perspective on interagency collaboration on behalf of delinquent youths. Conceptual frameworks for collaboration identified by probation officers can be used to develop and test collaborative systems of care to optimize the effectiveness of mental health and juvenile justice systems toward their complementary goals of mental health symptom reduction, improved functioning, and reduced recidivism. Needed are empirical studies that examine the relative effectiveness of the collaboration models described here.
Acknowledgments and disclosures
This work was supported by grant 9916 from the William T. Grant Foundation.
The authors report no competing interests.