Major depression affects about 16% of adults in their lifetime (
1), and the limitations in functioning and well-being associated with it make it one of the most prevalent and disabling medical conditions worldwide (
2,
3). Depressive disorders are frequently complicated by co-occurring substance use and substance use disorders. In 2008, among U.S. adults with a major depressive episode, 20% had a substance use disorder, and among individuals with a substance use disorder, 16% had experienced a major depressive episode in the previous year (
4). Further, there are many more individuals with depressive disorders who use or abuse illicit substances or alcohol but who do not meet full criteria for a substance use disorder.
Despite a growing consensus that individuals with co-occurring major depression and a substance use disorder need disease-specific treatment, treatment trials that have established the efficacy of psychosocial therapies as treatments for major depression have typically excluded individuals with co-occurring substance use disorders (
5,
6). A consequence of this exclusion is a lack of evidence for the efficacy of psychosocial treatments for patients with major depression who use or abuse substances. Research on this topic is important because most community-based substance abuse treatment programs do not have staff who can prescribe antidepressant medications, which limits the use of this treatment type. Moreover, in low-income minority groups, many individuals prefer psychosocial treatments to medications (
7).
The BRIGHT (Building Recovery by Improving Goals, Habits, and Thoughts) study was a quasi-experimental, community-based effectiveness trial (
8) that evaluated 16 sessions of group cognitive-behavioral therapy (CBT) for residential treatment clients with persistent depressive symptoms. The intervention was designed to be feasible for use in residential substance abuse treatment settings and to be delivered by substance abuse treatment counselors who typically have little to no formal training in mental health care. We report here on the subgroup of participants who entered the BRIGHT trial with major depression. The analysis was undertaken for the purpose of extending the literature on the efficacy of psychosocial treatments for major depression to individuals entering substance abuse treatment.
Methods
We used a quasi-experimental design. Experimental (BRIGHT) and comparison (usual care) conditions were offered at four publicly funded residential substance abuse treatment facilities in Los Angeles County at alternating times. For the first four months, eligible participants who entered residential treatment at the largest site were assigned to BRIGHT, and all eligible participants at the other three, smaller sites were assigned to usual care. After four months this assignment pattern switched, and participants at the three smaller sites received BRIGHT, and participants at the largest site were assigned to usual care. This pattern of alternating assignment continued over a 3.5-year enrollment period from August 2006 through January 2009.
After a field interviewer described the study to participants, written informed consent was obtained. Of 299 participants enrolled, 135 (45%) had a diagnosis of major depression, and four (1%) had co-occurring major depression and dysthymia, based on interviews conducted two to four weeks after residential treatment entry. Details are described elsewhere (
8). The study was approved by the RAND Human Subjects Protection Committee.
The baseline interview included an assessment of current depressive disorders with the Composite International Diagnostic Interview and an assessment of alcohol and drug use severity with the Addiction Severity Evaluation Index. The timeline follow-back technique was used to capture past 30-day alcohol use frequency and intensity, and questions from the Addiction Severity Index were used to capture days of problem substance use, which was defined as the substance, including alcohol, that respondents identified as their biggest problem. Depressive symptoms were measured with the Beck Depression Inventory-II (BDI-II). We measured mental health functioning using the 12-Item Short Form, version 2 (SF-12). A posttreatment interview was conducted three months after enrollment (follow-up 1), and another was conducted six months after enrollment (follow-up 2).
The BRIGHT intervention is described elsewhere (
8). To avoid inadvertent exposure of usual care clients to BRIGHT, the intervention was provided by outpatient counselors who were employed by the same parent organization and who traveled to the residential sites to deliver the intervention and then returned to their outpatient settings. Outpatient counselors had no contact with usual care clients. Usual care residential counselors had qualifications and experience similar to those of the outpatient counselors who delivered the intervention. Previous research demonstrated that counselors were delivering the intervention with fidelity (
9).
We conducted bivariate analyses on baseline characteristics to confirm that there were no significant differences between participants with major depression assigned to BRIGHT and usual care conditions and between respondents and nonrespondents at follow-up 1 and follow-up 2. Mental health outcomes were depression symptoms (BDI-II) and mental health functioning (SF-12). The two substance use outcomes were percentage of days of alcohol use or problem substance use out of days available for use during the past 30 days. BDI-II and SF-12 were modeled with repeated-measures mixed-effects regressions, with controls for the baseline value of each outcome and with the intraclass correlation of outcomes accounted for among participants attending group CBT sessions together (
10). Intervention effects at follow-ups 1 and 2 were estimated with coefficients for predictor variables of intervention assignment, follow-up wave, and intervention wave (
11). We also calculated the proportion of participants in each study condition whose depressive symptoms were minimal (BDI-II score ≤13) and compared the proportion with minimal symptoms in each condition at the two follow-up points.
We examined substance use outcomes at follow-up 2 because most clients (67%) remained in the residential treatment program at follow-up 1. Analyses were performed for the 69% of clients with any days available for use in the 30-day window at follow-up 2. We conducted a chi square test to confirm that the percentage of participants in BRIGHT versus usual care who had zero days available for use did not significantly differ. Because the estimated intraclass correlation in substance use outcomes associated with CBT session attendance was zero, we compared BRIGHT versus usual care using two-sided t tests.
Results
For the 135 individuals with major depression in the sample, response rates for follow-up 1 and follow-up 2 were 86% (N=116 at both follow-ups). Response rates for usual care versus BRIGHT did not significantly differ at either assessment, and baseline characteristics did not significantly predict nonresponse. The 64 participants assigned to BRIGHT attended a mean±SD of 9.8±5.7 sessions out of 16; 63% (N=40) attended at least eight sessions.
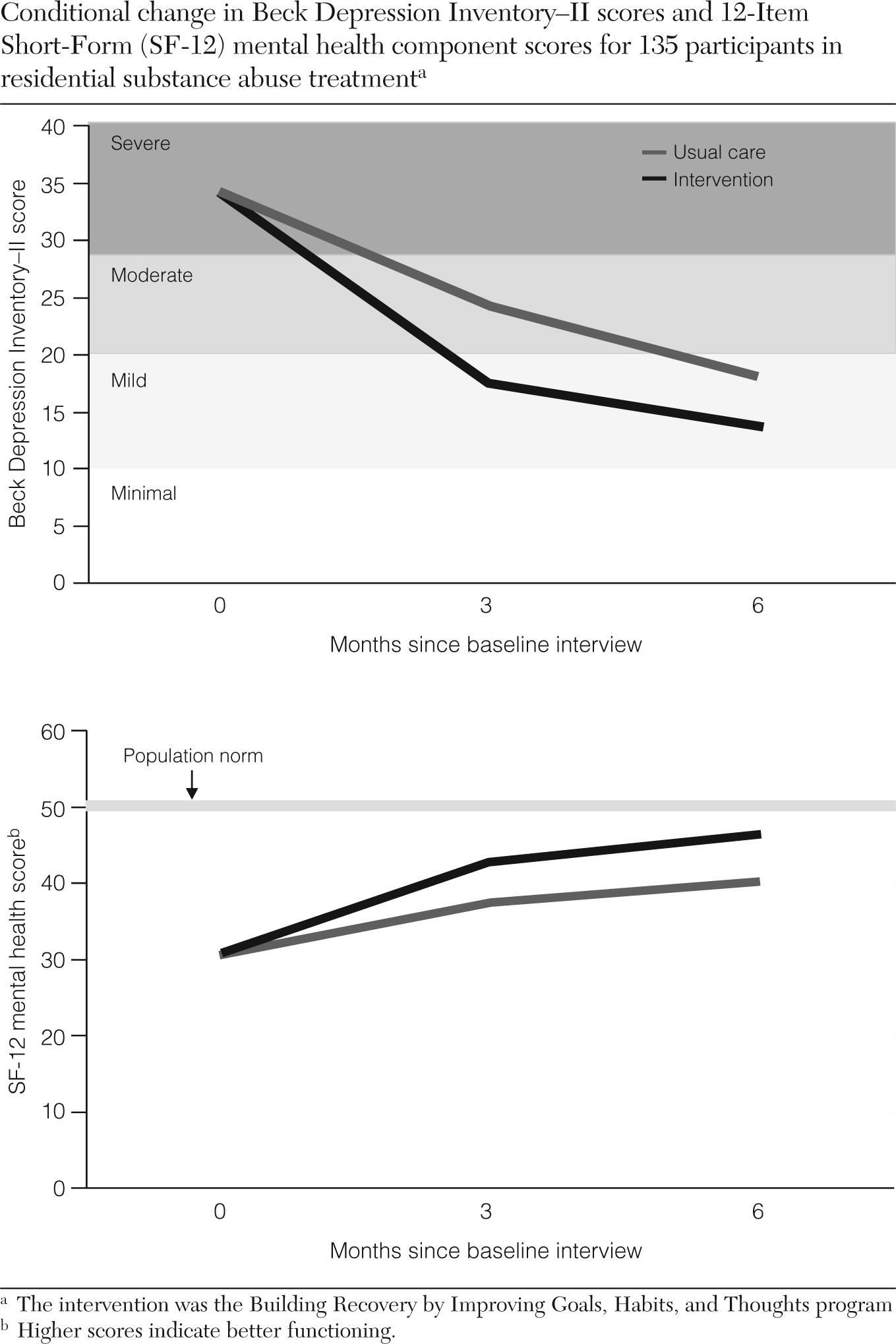
At follow-up 1, BRIGHT participants reported less severe depressive symptoms and higher mental health functioning than usual care participants (7.0-point difference in BDI-II scores, p<.01; difference in SF-12 scores=5.5, p<.05). At follow-up 2, the BDI-II difference was smaller (4.3-point difference, p=.08) and the SF-12 difference remained significant (6.2, p<.05). At follow-up 1, the group mean BDI-II score for the BRIGHT participants was in the mild range (mean±SE BDI-II score=17.1±1.9), whereas the group mean score for the usual care participants was in the moderate range (mean±SE BDI-II score=24.1±1.4). At both follow-up 1 and follow-up 2, more BRIGHT participants had minimal symptoms compared with the usual care group (follow-up 1, N=30, 57%, versus N=15, 24%, p<.001; follow-up 2, N=37, 65%, versus N=24, 41%, p<.001).
The usual care and BRIGHT conditions had similar percentages of participants still in residential treatment, and therefore with no days available for any substance use, at follow-up 2 (N=39, 68%, versus N=41, 70%, respectively, p=.91). The percentage of days in which a problem substance was used was 13.8 percentage points lower for the participants in the BRIGHT group (p<.05), but the groups did not significantly differ on alcohol use.
Figure 1 shows the change in BDI-II and SF-12 scores over time, conditional on clients having average baseline scores on each outcome measure at six months. [A figure available online as a data supplement to this brief report shows alcohol and problem substance use at six months.]
Discussion
Our results add to the literature on psychosocial treatments for major depression and extend the effectiveness of group CBT to a new setting, patient population, and type of provider. To our knowledge, this is the first large-scale depression psychotherapy trial conducted within community-based substance abuse treatment settings that included sufficient numbers of individuals with a diagnosis of co-occurring major depression to report on effectiveness. Few depression treatment trials have been conducted within substance abuse treatment settings, and psychotherapy treatment trials for major depression have typically excluded individuals with substance use disorders. Previous research that has examined the effectiveness of psychosocial treatments for co-occurring depression and substance use disorders have included either pharmacotherapy as part of the intervention or individuals with mild depressive symptoms rather than major depression (
12–
15). No depression treatment trials have used substance abuse treatment counselors, who typically do not have specialized mental health education or training.
These results have several implications. If more broadly implemented, this approach could increase access to effective mental health care and improve outcomes for the many individuals who enter substance abuse treatment with co-occurring major depression. The barriers to accessing both mental health and substance abuse treatment are well known, as are the social and economic consequences of untreated depressive disorders. Antidepressant pharmacotherapy is not a feasible treatment option for most community-based treatment programs because few programs have prescribing providers on staff and because most programs are publicly funded and do not have the funding mechanisms or resources that would enable them to hire mental health professionals. Because BRIGHT was implemented with existing staff, and because substance abuse counselors typically have lower salaries than depression treatment providers, the costs are likely to be less for this treatment than for other depression interventions, further increasing access. Finally, because our results suggest that BRIGHT is associated with improved outcomes for people with co-occurring substance use and major depression, it may be useful in other health care settings, such as primary care or specialty mental health care, where a diagnosis is necessary for providers to receive payment for treatment.
Our study had several limitations. Although we did not assess substance use diagnoses, the ASI alcohol and drug evaluation indices suggest that the substance use severity of study participants was similar to that of participants in other substance abuse treatment programs. Despite our efforts to develop and evaluate a treatment tied to the resources available to substance abuse treatment providers, additional training resources were required (
9). We did not conduct a randomized trial, although our quasi-experimental study design, in which sites alternated between delivering the intervention and usual care, minimized the chance that unmeasured site or personal characteristics would influence outcomes. The two conditions also did not differ on observed characteristics, such as age, gender, type of substance used, and current antidepressant treatment.
Results from our study should be generalizable to the large population of individuals with major depression entering residential substance abuse treatment. Our study population included individuals of diverse cultures and ethnicities, and study sites were geographically spread across Los Angeles County. Also, participants used a range of substances; we included individuals who were taking antidepressant medication as long as they met criteria for major depression at the time of enrollment.
Conclusions
Community-based substance abuse treatment providers have few options for providing depression treatment with demonstrated efficacy. Our study demonstrated that it is possible to develop the capacity of the substance abuse treatment system to deliver evidence-based mental health care by expanding the skills and clinical roles of substance abuse counselors. If more broadly implemented, this approach could increase access to effective mental health care for the many individuals who enter the substance abuse treatment system with co-occurring major depression. It may also be useful to disseminate this treatment more broadly for the many individuals with co-occurring depression and substance use who seek treatment within primary and specialty mental health care, where a diagnosis of depression is necessary for reimbursement.
Acknowledgments and disclosures
This project was sponsored by grant R01 AA014699 from the National Institute on Alcohol Abuse and Alcoholism. This study is registered at
www.clinicaltrials.gov (NCT01191788).
The authors report no competing interests.