Depression affects nearly one in five Americans at some point in their lives, resulting in a great deal of suffering and social and fiscal cost (
1). Although our understanding of the prevalence, phenomenology, and treatment of major depression has advanced considerably, the delivery of adequate specialized psychiatric care to affected individuals remains a challenge. This is particularly true for Hispanics and Latinos in the United States, for whom geographic, socioeconomic, linguistic, and cultural factors create a special need for understanding and sensitivity, further compromising their access to appropriate care (
2).
Even though primary care providers often diagnose and treat depression, the quality of care for depression has been found to be higher when delivered by mental health professionals (
3) and when delivered by linguistically and culturally congruent providers (
4). Hispanic patients, especially those who are less acculturated, may be less likely than patients from other racial-ethic groups to be medically literate, comfortable with the use of new technology, and proficient in English; less open to the need for psychiatric services, the use of prescription drugs, and receipt of professional help for emotional problems; and less familiar with the availability of services (
2).
Depression care typically involves an examination of the patient, which consists primarily of a spoken interview, and interventions that often include pharmacotherapy and talk therapy. The use of technology may facilitate access to specialized, linguistically and culturally congruent providers. Telepsychiatry has been shown to produce significant improvements among patients; however, the acceptability, diagnostic adequacy, and treatment outcomes of this mode of service delivery for Hispanic patients with depression is not known.
Telepsychiatry is usually carried out with sophisticated teleconferencing equipment and specialized wiring infrastructure that is out of reach of many community health centers and thus unavailable to uninsured, underserved individuals. A more accessible medium that uses commercially available Webcams and standard Internet connectivity is needed. The American Psychiatric Association has suggested that a high bandwidth is not needed for satisfactory transmission, although technological glitches will damage the acceptability of the medium for both patients and providers (
5). Nevertheless, the Internet is increasingly the method of communication for immigrants, who can see and speak with their relatives in distant locations. Although occasional glitches in home technology may be acceptable, the acceptability of this level of technology as a treatment medium has to be tested on the groups that may benefit from it. This broadly available and affordable technology can then be applied to improve the quality of care for underserved populations, reduce disparities in health care, and improve the health of people from minority groups, both in urban and in rural areas where there are shortages of health professionals.
Methods
The study compared the effectiveness and acceptability of specialized psychiatric treatment provided remotely through the Internet by using real-time video communication (Webcam intervention) with treatment as usual at a community health center.
Participants
A total of 182 self-identified Hispanic patients with a major depressive episode were invited to participate; four refused and 11 were ineligible (screened out or did not follow up with baseline assessments), leaving 167 enrolled study participants, most of whom were foreign born. The demographic characteristics of the sample, including general health, marital, financial, and employment status and other characteristics have been reported elsewhere (
6).
Screening and recruitment
Registration staff members at a community health center were instructed to invite every registering patient to complete depression screening with the nine-item Patient Health Questionnaire (PHQ-9). Participants with a PHQ-9 score of 10 or higher during routine clinic screening (
7,
8) were invited to participate in formal diagnostic confirmation of a
DSM-IV-TR major depressive episode with the Mini-International Neuropsychiatric Interview (MINI) (
9).
Exclusion criteria
Patients were excluded if they had a diagnosis of bipolar affective disorder, schizophrenia, schizoaffective disorder, dementia, current substance dependence based on the MINI, or any concurrent DSM-IV axis I disorder that required inpatient or crisis residential treatment at the time of screening. Patients were also excluded if they manifested signs or symptoms of serious general medical or neurological illness (for example, severe liver or renal failure) that in the opinion of the primary care provider was likely to increase the risk of complications during treatment or if they manifested signs or symptoms of serious general medical illness that may have explained the observed depressive symptoms (for example, traumatic brain injury or uncontrolled seizures). Patients were also excluded if they had active suicidal or homicidal ideation or were felt by one of the investigators on the basis of clinical presentation and history to pose a significant risk of harm to themselves or others, if they were pregnant or lactating, or if they lacked mental capacity to provide informed consent.
Procedure
After complete description of the study to participants in the participant’s preferred language, written informed consent was obtained before the MINI was administered. Patients who met all entry criteria were randomly assigned to the Webcam condition (N=80) or the control condition of treatment as usual (N=87). Participants were offered treatment and data collection visits for a period of six months between July 2008 and June 2010. Clinician ratings were conducted by a rater who was blind to the participant’s treatment condition. [A flowchart depicting study recruitment and completion is available online as a data supplement to this article.]
Webcam intervention
Patients assigned to the Webcam intervention were given appointments with one of two bilingual psychiatrists, who provided services in the patient’s preferred language (all the patients preferred Spanish). For patients, the remote session took place in a consulting room at the community health center where they received medical care. All equipment in the consulting room complied with provisions in the Health Insurance Portability and Accountability Act. It included a fax (used for signature requirements for prescriptions, consent forms, and treatment plans and for medical records exchange) and a standard computer set up with commercially available higher-resolution Webcam equipment (Logitech QuickCam Orbit AF).
This intervention consisted of six monthly Webcam sessions with the psychiatrist. The first session, which lasted 45 to 60 minutes, included initial psychiatric evaluation and treatment. The six subsequent sessions lasted 20 to 30 minutes and included evaluation and management. Psychiatrists offered medication management using measurement-based treatment consistent with the Texas Medication Algorithm Project (TMAP) (
10). In addition, patients received psychoeducation and other brief eclectic interventions as appropriate, mostly supportive in nature. Before each session, the project recruiter initiated the Webcam connection and ensured that the psychiatrist and patient were in place and the equipment was functional. At the end of the six months, patients were transitioned back to the primary care provider or specialist for appropriate management. This process included sharing study records, including a written psychiatric assessment, follow-up progress notes, and the medication log. The study recruiter provided notification and clinical updates as she handed Webcam participants back to the primary care provider. Study psychiatrists were also available for case discussions when required and routinely wrote follow-up treatment recommendations, most importantly in cases where participants remained depressed.
Emergency contact information was provided to participants in each treatment condition. Webcam patients were covered by the psychiatry department crisis system, and patients receiving treatment as usual were covered through their home clinic crisis line. The study psychiatrists could adjust the treatment schedule or content as necessary to secure the safety of the patient and others and to ensure adequate clinical progress. All participants received general medical care from their primary care providers.
Treatment as usual
Depression treatments for patients randomly assigned to treatment as usual were determined by their assigned primary care provider and based on guidelines by the Agency for Healthcare Research and Quality (
11). Treatments often included generic antidepressants; some patients received counseling through the behavioral health clinicians on site. Patients in the treatment-as-usual group who required additional mental health care were referred to community mental health agencies. Primary care providers included three family physicians and three independent family nurse practitioners. They were sufficiently fluent in Spanish to conduct general medical assessments and monitor specific depression symptoms; however, they were generally less able to converse in depth about important social and psychological issues contributing to patients’ clinical presentation and management.
Other interventions
All study participants were allowed to continue using—or were referred for—other services available at the clinic, such as individual, couples, and family counseling provided by master’s-level bilingual behavioral health counselors. The Webcam participants had a mean±SD of 4.0±2.3 visits, and those receiving treatment as usual had 4.3±3.6 counseling visits.
Measures
Effectiveness was measured with widely used scales that address aspects of depression symptom severity and that measure continuous and categorical response and remission changes. These scales included the clinician-rated Montgomery-Åsberg Depression Rating Scale (MADRS) (
12) and the self-rated PHQ-9 (
7). Categorical outcomes were prospectively defined: response was a 50% or greater decrease in severity ratings, and remission occurred when the decrease was 75% or greater. Similarly, impact of depressive symptoms on quality of life was measured with the self-rated Quality of Life Enjoyment and Satisfaction Questionnaire (Q-LES-Q) (
13), and health-related functional ability was measured with the self-rated Sheehan Disability Scale (SDS) (
14).
Data analysis
The main hypothesis was that patients who were randomly assigned to the Webcam intervention would show a greater decrease in depression rating scores and greater improvements in quality of life and functional ability than patients randomly assigned to treatment as usual.
Data analysis software (Predictive Analytics Software [
15]) was used to conduct analysis of variance (ANOVA) with repeated measures (baseline and three and six months) and to analyze clinician-rated (MADRS) and patient-rated (PHQ-9) depression severity measures and measures of quality of life (Q-LES-Q) and functional ability (SDS). Between-subjects variables included treatment condition (Webcam intervention versus treatment as usual). Categorical changes were assessed with t tests, using intent-to-treat analysis with last observation carried forward and comparing the proportion of patients showing response and remission in the two treatment groups.
Fidelity measurement
To monitor protocol adherence to the Webcam intervention, study notes were reviewed for 50% of the patients (N=40) and video-recordings were reviewed for 10% (N=8). Bilingual psychiatric clinicians who were not involved in providing care conducted these reviews.
To enhance reliability, a single clinician who was blind to the treatment condition conducted the MADRS ratings during separately scheduled clinic visits. All self-ratings were obtained by the study recruiter–clinician on the date of the treatment visit.
Results
Participants
A total of 87 participants were assigned to treatment as usual—75 women (86%) and 12 men (14%)—with a mean±SD age of 43.2±11.9 years. A total of 80 participants were assigned to the Webcam intervention—73 women (91%) and seven men (9%)—with a mean age of 42.8±12.0. No statistically significant differences were found between groups in demographic characteristics, such as age, sex, education level, employment or marital status, and perceived general medical health (
6). The study was conducted with minimal variation from the study protocol. Independent raters assessed fidelity of treatment for the Webcam providers and found them to be in compliance with the format proposed for evaluation and treatment. Any variations from the TMAP algorithm were reconciled and were either explained by patient choice or corrected upon supervisory review. Results for the target outcomes are presented below. [The online appendix includes figures summarizing the time trajectory of mean scores on the MADRS, PHQ-9, Q-LES-Q, and SDS for both treatment groups.]
Depression
For patients in both treatment conditions, significant reductions in symptom severity were seen over time (
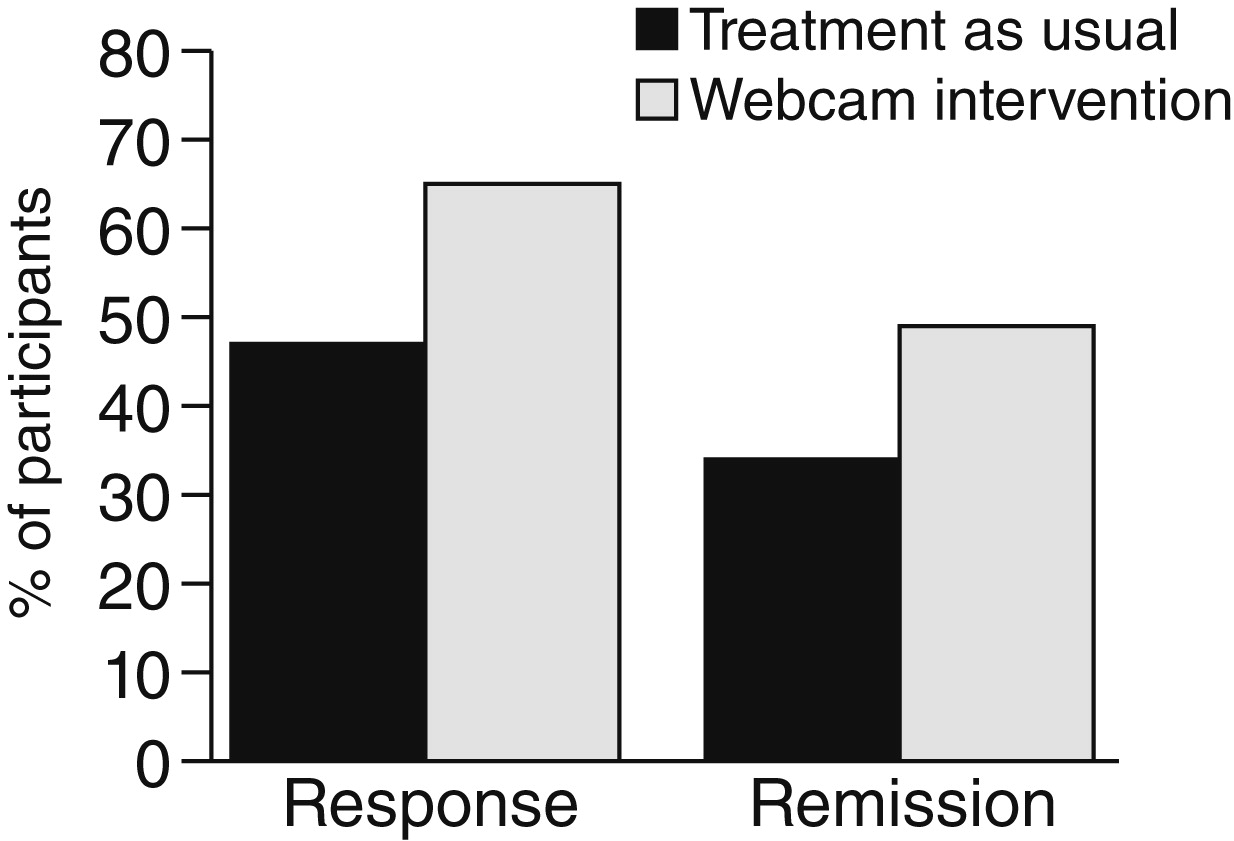
Table 1). ANOVA with repeated measures showed a significant main effect of time for the MADRS (F=120.55, df=2 and 122, p<.001) and a significant interaction of time by intervention (F=5.93, df=2 and 244, p<.01) favoring the Webcam intervention. For the PHQ-9 there was also a significant main effect of time (F=212.14, df=2 and 130, p<.001) and a significant interaction of time by intervention (F=3.6, df=2 and 260, p<.05) favoring the Webcam intervention. Analyses using last observation carried forward yielded the following results. Of 159 evaluable cases for whom at least baseline ratings were collected (85 treatment as usual and 74 Webcam intervention), 88 patients (55%) showed a treatment response—40 (47 %) in the treatment-as-usual group and 48 (65%) in the Webcam group (t=2.75, df=157, p=.024). In addition, 65 patients (41%) achieved remission—29 (34%) in the treatment-as-usual group and 36 (49%) in the Webcam intervention group (t=1.87, df=157, p=.06) (
Figure 1).
Quality of life
Q-LES-Q scores indicated significant increases in quality of life over time for both treatment groups. ANOVA with repeated measures showed a significant main effect of time for Q-LES-Q (F=112.16, df=2 and 130, p<.01) and a significant interaction of time by intervention (F=3.1, df=2 and 260, p<.05) favoring the Webcam intervention.
Functional ability
Disability ratings decreased significantly over time for both treatment groups. ANOVA with repeated measures showed a significant main effect of time for the SDS scores (F=129.43, df=2 and 131, p<.01) and a significant interaction of time by intervention (F=3.23, df=2 and 262, p<.05) favoring the Webcam intervention.
Discussion
Measurement- and algorithm-based treatment for depression provided by a psychiatrist via the Webcam intervention led to significant improvements in depression severity, functional ability, and quality of life. Patients completed the PHQ-9 at each session, which was used to determine response and remission rates and guide prescribing behavior based on the TMAP. The response rate of patients in the Webcam intervention was significantly higher than that seen among patients receiving treatment as usual that was delivered by primary care providers. The remission rate for patients in the Webcam intervention was also higher, but the difference did not reach statistical significance (p=.06).
It is possible that some of the differences between the treatment groups result from the use of measurement-based, algorithm-informed treatment with a target of full remission. Various artifacts introduced by the protocol should be considered as study limitations. Examples include the small proportion of male participants, which limits the generalizability of the findings. In addition, per study protocol, patients in the Webcam group were seen more regularly and extensively and had visits dedicated to the treatment of depression, whereas patients in the treatment-as-usual group received customary care at the clinic, with an average of 3.2 visits during the study period. These differences are likely to have affected clinical outcomes.
This study did not measure adequacy of care in the treatment-as usual group, and the differences in response and remission rates may have resulted from provision of less than adequate care to this group. However, in support of the adequacy of care provided by the primary care providers, the outcomes observed for patients in the treatment-as-usual group are consistent with response and remission rates among patients in effectiveness studies of antidepressants, including primary care patients with uncomplicated major depression, such as participants in STAR*D (Sequenced Treatment Alternatives to Relieve Depression) (
16).
To our knowledge this is the first study to use common household technology to provide psychiatric care to patients with depression. Because patients with depression received effective care via this method, it should be further investigated, especially if use of the Webcam intervention can facilitate access to specialized care that is both linguistically and culturally congruent for patients from underserved communities. Using this technology also allows patients to receive specialty care at the site where they obtain primary care services, which is a clear advantage that minimizes the usual mobility limitations and discomfort that patients from underserved immigrant populations often experience when they are referred to community psychiatric clinics or tertiary care centers.
Conclusions
The findings of this study of primarily Mexican immigrant Hispanic patients being treated for major depression at a community health center suggest that use of measurement- and algorithm-based treatment for depression by psychiatrists via Webcam can lead to improvements in depression severity, functional ability, and quality of life that are at least equivalent and possibly superior to improvements achieved with treatment as usual delivered by primary care providers. Use of common household information technology may help facilitate access to linguistically and culturally congruent psychiatric specialty care among underserved Hispanic patients.
Acknowledgments and disclosures
Funding for this study was provided by the Finding Answers Program, Robert Wood Johnson Foundation (grant 64305). The authors thank Martha Preciado, B.A., Ellen Ouellette, B.S., Katherine Ovsevitz, M.P.H., Veronica Mendoza-Jenkins, M.D., Adolfo Martinez-Costelo, M.D., and the patients and staff at St. Elizabeth’s Health Center.
The authors report no competing interests.