Posttraumatic stress disorder (PTSD) is the most common psychiatric condition for which veterans seek disability compensation from the Department of Veterans Affairs (VA). Although most veterans with PTSD have some college education, few have jobs, almost 40% are impoverished, and most have lower scores on measures of work role and social functioning than people with serious mental illness (that is, bipolar I disorder, schizophrenia, schizoaffective disorder, other psychotic disorder, or major depressive disorder with psychotic features) (
1).
According to a 2011 report from the U.S. Department of Labor, the 2010 unemployment rates were 11.5% for Gulf War-era II veterans, 21% for Gulf War-era II veterans with service-connected disabilities, 13% for all service-connected veterans of all eras combined and 9.4% for nonveterans (
2). Veterans of Gulf War era II include all those who served in the military since September 2001, which includes those serving in Operation Enduring Freedom and Operation Iraqi Freedom. The unemployment rates for civilians with PTSD and veterans with PTSD are much higher than the rates for the civilian and veteran general population (
3). According to a recent VA Northeast Program Evaluation Center report, 61% of veterans (N=11,647) entering specialized outpatient PTSD programs were not working (26% were retired, 22% were completely disabled, 27% were unable to find work, and 25% were not looking for work) (
4).
Among veterans with PTSD, seeking disability compensation has not adversely affected clinical outcomes (
5,
6). However, disability compensation programs for veterans have appeared to discourage full participation in vocational rehabilitation programs, which has resulted in poorer rehabilitation outcomes (
7).
Prior randomized trials have shown that compensated work therapy through Veterans Health Administration (VHA)-contracted industries had initially positive but declining effects on addiction outcomes and episodes of homelessness and incarceration (
8). In a Northeast Program Evaluation Center study evaluating electronic data for 5,862 veterans from 122 compensated work therapy programs (
9), veterans with PTSD were 19% less likely to be employed at discharge from the VHA compensated work therapy program than those without a diagnosis of PTSD (that is, 30% and 36% employed, respectively). Veterans with PTSD involved in compensated work therapy were no more likely to be employed at four-month follow-up than those who participated in a specialized PTSD treatment program (
10). Thus the standard VA Vocational Rehabilitation Program (VRP) does not meet the occupational recovery needs of veterans with PTSD.
Individual placement and support (IPS) supported employment is an evidence-based vocational rehabilitation model that has been shown to improve occupational and rehabilitation outcomes for people with severe and persistent mental illness, but few participants with a primary diagnosis of PTSD have been included in previous studies (
11–
15). Engaging in competitive employment, rather than in sheltered jobs, has been shown to enhance other recovery outcomes, such as self-esteem and quality of life, among people with serious mental illness (
16).
The impact of IPS supported employment for individuals with a primary diagnosis of PTSD has not been studied. Our study specifically addressed this gap in the field of rehabilitation research. We hypothesized that participants assigned to IPS would have a higher competitive employment rate than their counterparts assigned to VRP. A secondary hypothesis postulated that those assigned to supported employment would work competitively for a higher proportion of eligible weeks than those assigned to VRP.
Methods
Participants
From 2006 to 2010, veterans with PTSD at the Tuscaloosa VA Medical Center (VAMC) were enrolled in a 12-month, prospective randomized comparison of IPS and VRP. This study (
www.ClinicalTrials.gov identifier number NCT00333801) was approved by the Tuscaloosa VAMC Institutional Review Board. A trained investigator or clinical research coordinator explained all study procedures, alternatives to participation, and potential benefits and risks to prospective participants and obtained their written informed consent before study enrollment. Veterans were eligible for the study if they had a diagnosis of PTSD, were aged 19 to 60, were eligible for the Tuscaloosa VAMC VRP (that is, had a medical clearance that they were able to participate in a work activity; work restrictions had to be noted, if present), were currently unemployed, were interested in competitive employment, and were planning to remain in a 100-mile radius of the Tuscaloosa VAMC for the 12-month duration. Veterans were excluded if they had a lifetime history of severe traumatic brain injury that resulted in severe cognitive disorder; a diagnosis of schizophrenia, schizoaffective disorder, or bipolar I disorder (because these individuals are already eligible for IPS); a diagnosis of dementia; immediate need of detoxification from alcohol or drugs; or pending active legal charges with expected incarceration. A history of mild to moderate traumatic brain injury and all other comorbid axis I diagnoses, including substance use disorders, bipolar disorder type II, major depression, and other anxiety disorders, were permissible.
Interventions
Both interventions operated under the VHA Compensated Work Therapy program. The final goal for both interventions was competitive employment, although the methods and pathways were different.
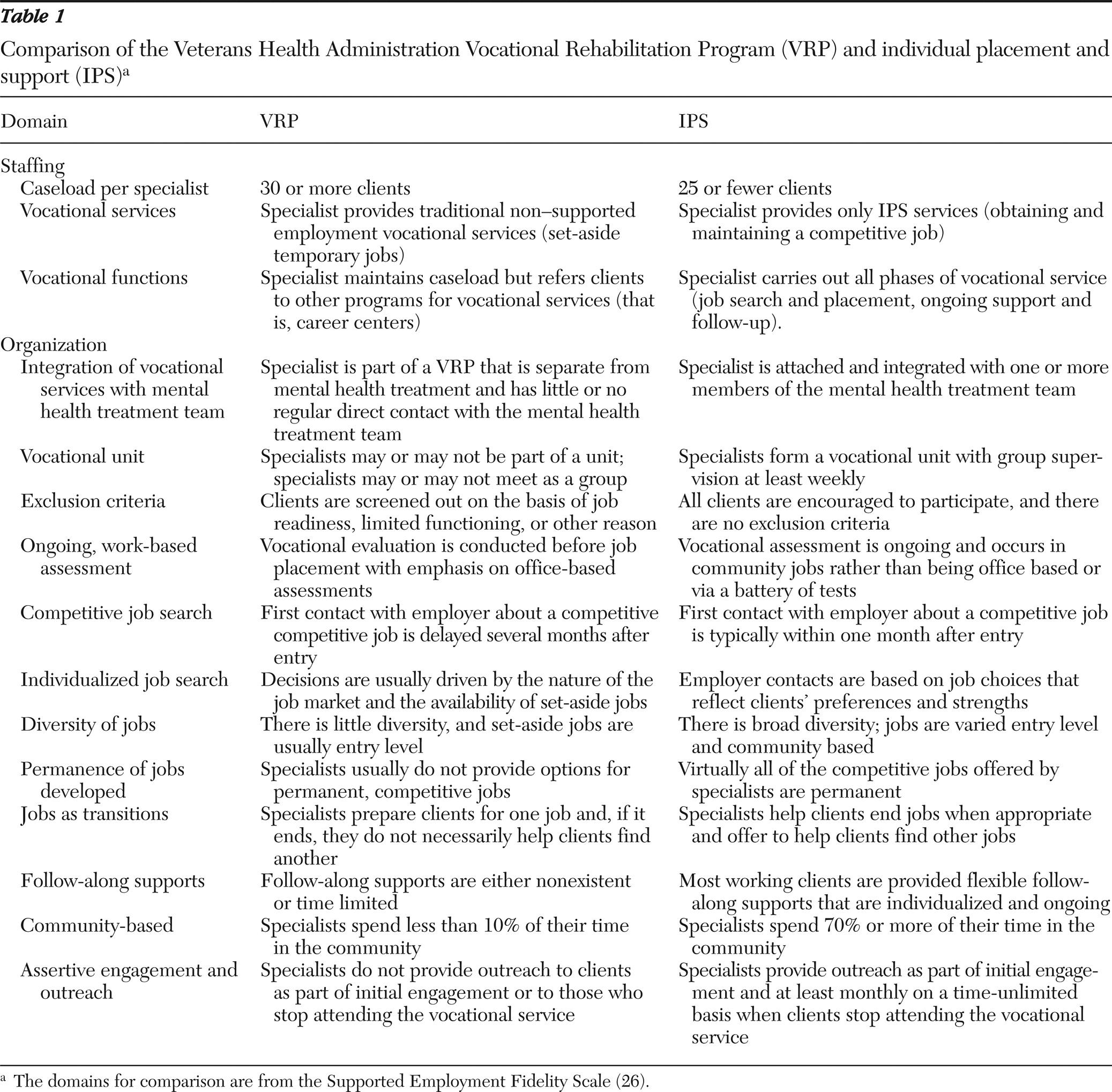
Table 1 provides an overview of the interventions and the differences between them. The IPS intervention involved several important features. Eligibility was based on the participant's choice and interest in competitive work. The IPS specialist was integrated into the clinical mental health or PTSD treatment team, carried out all phases of the vocational services, provided predominantly community-based services, provided assertive engagement and outreach in community-based employment, had a caseload of no more than 25 clients, and provided continuous, time-unlimited, follow-along supports for vocational services. IPS involved rapid job search and individualized placement in diverse competitive jobs, with ongoing work-based vocational assessment and assistance in finding subsequent jobs, if needed. Group supervision is regularly scheduled with IPS specialists and an IPS supervisor. The IPS model is described in
A Working Life for People With Severe Mental Illness (
17) and an IPS manual from the Substance Abuse and Mental Health Services Administration (
18). These references served as the study's manuals for IPS.
VRP followed the standard care in place at the Tuscaloosa VAMC, which included one or more of these components: routine prevocational testing and evaluation for all patients on referral to VRP, vocational rehabilitation therapy that provided a work regimen with monetary incentives derived from contracts whereby participants are paid on a piece-rate basis related to their production, and a transitional work program that included a temporary work experience (that is, time limited) either within the Tuscaloosa VAMC or in community settings (called the transitional work external or transitional work experience). The VRP model featured a VRP specialist who carried out some, but not all, phases of the vocational service; provided some community-based services (if a temporary work setting was external to VAMC), provided time-limited job search assistance to help the client obtain competitive employment, and had no maximum caseload. VRP had an initial short-term set-aside of transitional work experiences (such as work in VAMC environmental management services, food services, delivery services, or community jobs in food or other service delivery environments) that were not necessarily individualized to the patient's long-term preferences and had very little integration with the mental health treatment team. The VRP specialist assisted the veteran in a limited search for placement in a competitive job that was delayed until after the set-aside work experience neared completion and provided time-limited follow-along support during the set-aside work experience, with little or no long-term follow-up vocational assistance after the first competitive job was obtained.
Assessment procedures
After providing informed consent at baseline, participants underwent a psychiatric and general medical evaluation, including a medical history, psychiatric history, and family psychiatric history. The clinical research coordinator recorded a comprehensive history of level of education, past employment, housing, relationships, major traumatic life events, and disability status. The clinical research coordinator also evaluated the participant for PTSD and other axis I disorders using the Mini-International Neuropsychiatric Interview (
19). Participants were instructed to keep a job log formatted in a daily calendar that captured whether they were employed, number of hours worked, wages earned, and reasons for missed work. At baseline and one-, two-, three-, four-, six-, eight-, ten-, and 12- month follow-up visits, the clinical research coordinator collected the participants' job logs and reviewed the calendar with the participant for completeness. The clinical research coordinator recorded on a case report form the number of job interviews, job offers, and jobs obtained and the type of jobs, number of hours worked, wages earned, and reasons for missed work or job termination for each week.
At the follow-up visits, a trained assessor administered the Clinician Administered PTSD Scale (
20), Clinical Global Impression-Severity (
21), 16-item Quick Inventory of Depressive Symptomatology-Clinician Rated (
22), and the Clinical Global Impression-Improvement, and veterans completed the Quick Inventory of Depression Symptomatology-Self-Report, World Health Organization Disability Assessment Schedule II (
23), Sheehan Disability Scale (
24), and Davidson Trauma Scale (
25). The assessors were kept blind to the intervention assignment. Although there was a concerted effort to maintain this blind, accidental unblinding occurred infrequently (exact frequency unknown), in which case the ratings were subsequently conducted by a different blinded rater.
To minimize attrition, the investigators provided thorough preenrollment education to all prospective participants about the study objectives and procedures to assess and confirm their commitment to and feasibility for long-term follow-up. If needed, the clinical research coordinator and assessor traveled to the participant's community for the participant's convenience. To enhance the rate of return and to address a loss-of-wage or transportation cost barrier, all participants received a modest payment for follow-up interviews, regardless of whether they continued in the IPS or VRP assignment.
Randomization
After signing informed consent and undergoing baseline assessments, eligible participants were assigned to receive either IPS or VRP. Assignment was based on a randomization list that was prepared before the study began. The IPS supported employment was provided for 12 months, and the VRP was of variable time-limited service as determined by the Tuscaloosa VAMC's VRP program limits. Participants were followed and assessed at 12 months after baseline, regardless of intervention adherence, employment status, type of discharge, or attrition from the IPS or VRP intervention.
Fidelity monitoring
The IPS specialists received ongoing training and supervision via monthly conference calls and quarterly site visits by the national IPS consultant (RT). During these visits, the consultant also conducted fidelity monitoring, which included reviewing the IPS specialist's caseload, meeting with veterans from both IPS and VRP interventions, interviewing participants' clinical providers, interviewing participants' employers, and rating the adherence of the IPS intervention with the Supported Employment Fidelity Scale (
26). The national consultant also conducted a Supported Employment Fidelity Scale assessment of VRP to ensure that the ratings were low—that is, that VRP remained different from the IPS intervention as was intended by the study design.
Outcome variables
The primary outcome was whether the participant engaged in competitive employment (yes or no). Competitive employment was defined as a job for regular wages in a setting that was not set aside, sheltered, or enclaved, that is, the same job could be held by people without a mental illness or disability and was not a set-aside job in the VRP. Day labor (that is, pick-up cash-based day jobs for yard work, babysitting, manual labor, and so forth) and military drill were not counted as competitive employment; however, data on income from all sources were collected. Secondary outcomes included the proportions of eligible weeks, days, and hours worked and gross income earned in competitive employment. Eligible weeks were defined as those in which the participant was not encumbered by a set-aside job (that is, a set-aside job in the VRP condition) and in which the participant was active in the study (that is, weeks during which the participant had exited the study were not counted because determining whether the participant was employed was not possible).
Data-analytic procedures
Using intent-to-treat analyses and two-tailed tests with significance set at p≤.05, we compared rates of competitive employment (the primary hypothesis) with chi square tests and number of eligible weeks of competitive employment (the secondary hypothesis) with a Mann-Whitney test. We also compared groups on the number of weeks, days, and hours worked in a competitive job; gross wages earned from all sources; and gross wages earned from competitive jobs. The between-group difference was tested by using either a t test or a Mann-Whitney test, depending on the distribution of the variable. There was no imputation for employment outcomes during the weeks in which the participants exited early and were no longer in the study. We examined the time (number of weeks) until the first week worked in a competitive job and used a Kaplan-Meier survival analysis with a log-rank test to compare intervention groups. Participants who did not get a job were classified as censored at their final assessment point.
Results
A total of 100 participants were assessed for eligibility, and 85 were randomly assigned to either IPS (N=42) or VRP (N=43). A total of 71 (84%) completed the one-year follow-up. Reasons for early exit included withdrawn consent (N=1), relocation (N=3), and incarceration (N=2) for the IPS group; for the VRP group reasons were loss to follow-up (N=2), relocation (N=5), and incarceration (N=1). [A CONSORT diagram illustrating recruitment and follow-up is available in an online appendix to this report at
ps.psychiatryonline.org.]
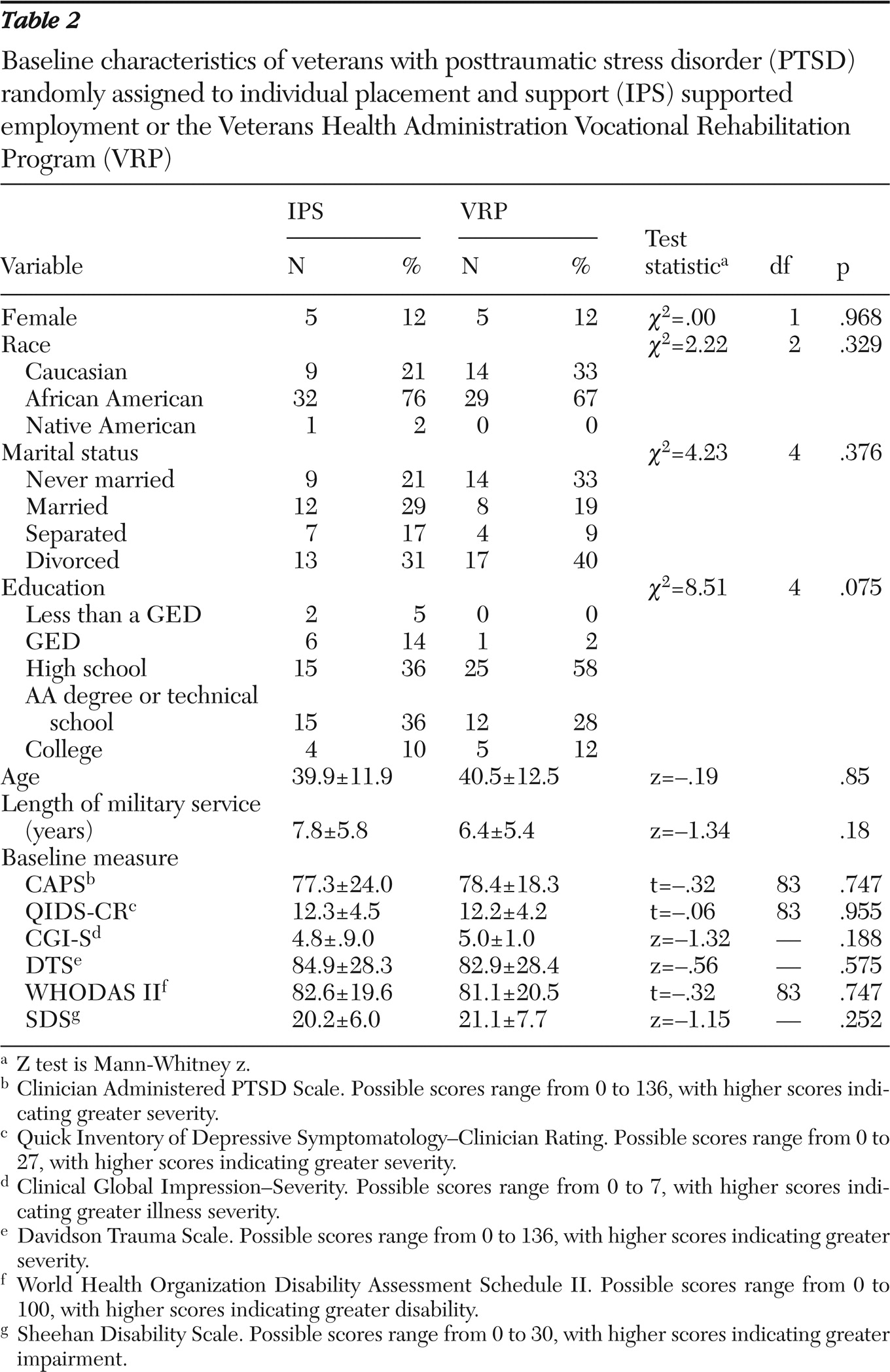
The 85 randomly assigned participants had been unemployed for a mean±SD of 18.9±42.0 months (range of 0–240 months; median of four months). In addition to PTSD, the participants had the following axis I disorders: major depressive disorder (N=76, 89%), dysthymia (N=17, 20%), agoraphobia (N=46, 54%), panic disorder (N=50, 59%), social phobia (N=24, 28%), alcohol dependence (N=36, 42%), alcohol abuse (N=18, 21%), drug dependence (N=31, 37%), and drug abuse (N=15, 18%). The baseline demographic characteristics and scores of the participants are shown in
Table 2. There were no significant differences between groups.
Thirty-two of the 42 IPS participants (76%) gained competitive employment, compared with 12 of the 43 VRP participants (28%) (χ2=19.84, df=1, p<.001). That is, veterans with PTSD who participated in IPS were 2.7 times more likely to gain competitive employment than those who received VRP. The number needed to treat was 2.07 (95% confidence interval=1.96–2.19). In other words, if three individuals received IPS and three received VRP, one more individual in the IPS intervention would get a competitive job. (Note that to treat 2.07 patients, three patients must be seen.)
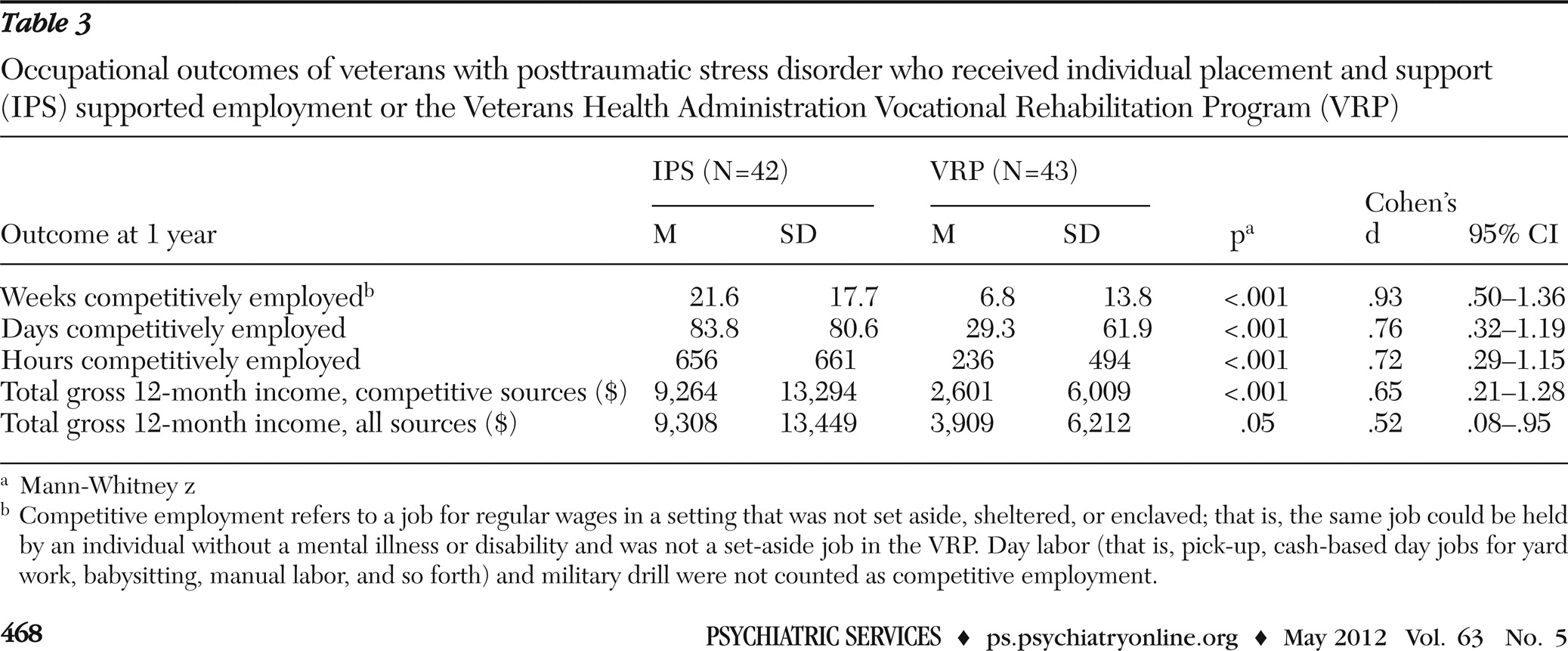
While in the study, IPS participants worked in a competitive job an average of 42% of the eligible weeks and those assigned to VRP worked an average of 16% of the eligible weeks (Mann-Whitney z test, p<.001). As shown in
Table 3, other occupational outcomes also favored IPS.
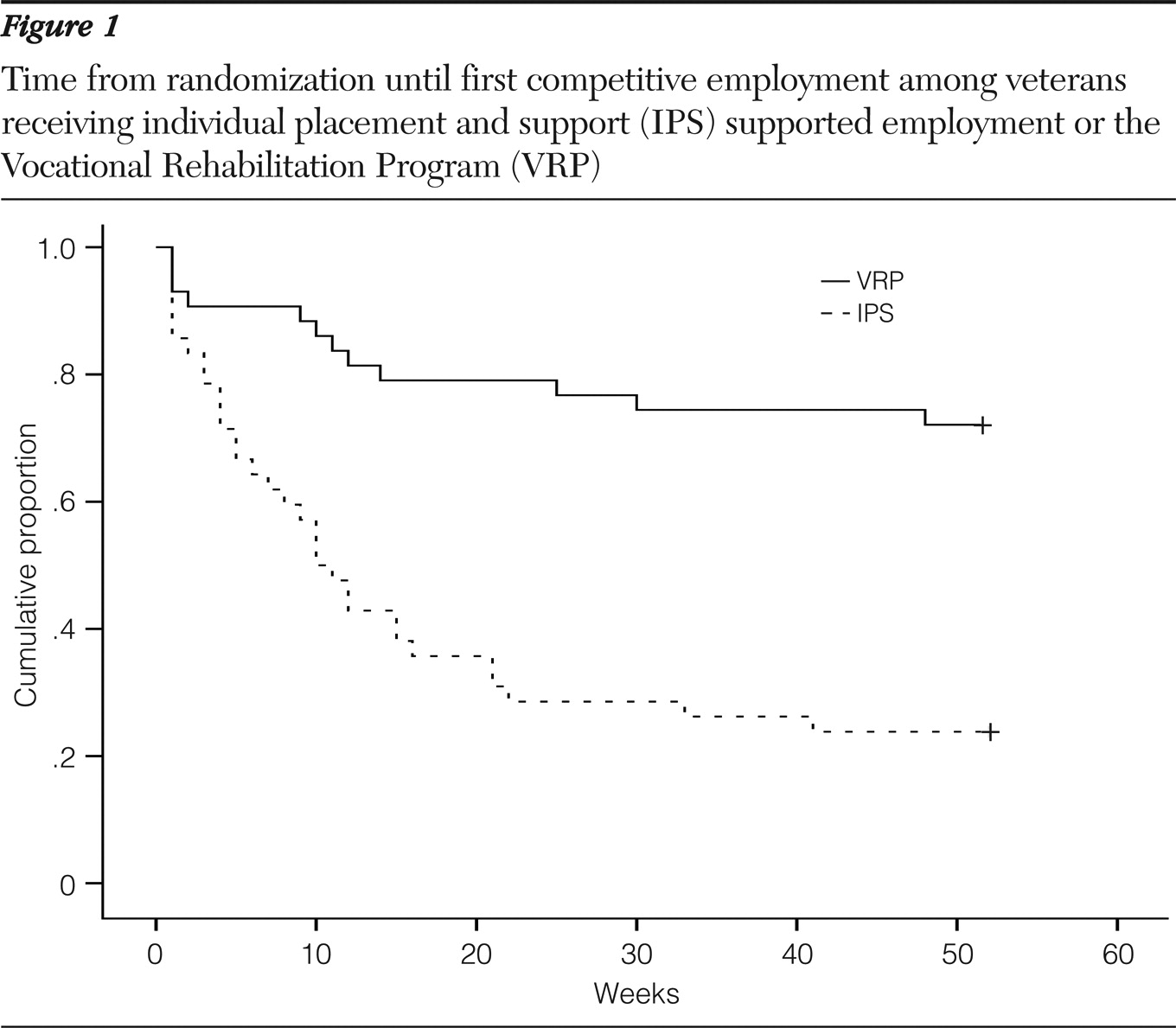
The Kaplan-Meier survival curves in
Figure 1 illustrate the time until first competitive job for each group. The IPS group achieved competitive employment significantly more quickly than the VRP group (log-rank Mantel Cox
χ2=21.32, p<.001). Most job acquisition occurred within the first 20 weeks of the IPS program.
The IPS fidelity monitor scored the Supported Employment Fidelity Scale as 55 at the onset of the study, and this score steadily improved to within a range of 58–65 during the study, with a mean±SD score of 61.2±2.1. On this scale, 66–77 is regarded as good IPS implementation, 56–65 as fair implementation, and ≤55 as “not supported employment.” The VRP was consistently rated by the fidelity monitor as ≤40 during the study, which is appropriate for this intervention.
Discussion
This study was the first to examine IPS supported employment outcomes for veterans with PTSD. Compared with those who received standard VRP services, unemployed veterans with PTSD who received IPS were 2.7 times more likely to gain competitive employment. Other employment outcomes, including time worked and total earnings, also favored IPS. These findings were consistent with previously reported advantages of IPS over traditional VRP (
11). More than a dozen randomized controlled trials have shown that IPS enhances vocational outcomes among patients with severe and persistent mental disorders. Moreover, the effect size in our study was similar to those in previous studies. Studies in samples of individuals with serious mental illness have consistently shown that 42%–78% of individuals who receive IPS gain competitive employment. In our study, 76% of veterans with PTSD who received IPS gained competitive employment compared with 28% of those assigned to VRP. The results for VPR in our study were consistent with those in a recent VA report that 30% of veterans with PTSD were competitively employed at discharge from a VA VRP program (
9).
The strengths of our study include its randomized controlled trial design, fidelity monitoring, and frequent follow-up assessments over one year. Limitations included the single study site, the limited number of IPS interventionists, and exclusion of nonveterans. A multisite trial with a larger and more diverse study sample would confirm the results and allow examination of secondary outcomes, such as PTSD symptoms, quality of life, and other such outcomes. In addition, a larger study could evaluate the cost-effectiveness of the IPS intervention.
Conclusions
In conclusion, occupational outcomes for veterans with PTSD were significantly better with the evidence-based IPS intervention than with a standard VA VRP. Our study was the first study of IPS to focus exclusively on individuals with PTSD and the first to directly compare the outcomes of IPS and VRP. The results of this study suggest that the VHA should consider changing its current guidelines for vocational services and provide IPS as a commonly available alternative intervention—and perhaps a preferred intervention—for all unemployed veterans with PTSD. IPS supported employment is patient centered in that it comprehensively addresses individual vocational needs, potentially enhancing clinical recovery and quality of life for veterans with PTSD. Given the large number of veterans returning from Operation Enduring Freedom, Operation Iraqi Freedom, Operation New Dawn, and other Southwest Asia deployments who often experience PTSD and confront unemployment upon military discharge, this study was timely and has critical implications for clinical care and vocational rehabilitation programming in the VA and elsewhere.
Acknowledgments and disclosures
This project was funded by VA Rehabilitation Research and Development grant D4092i and is registered at
www.ClinicalTrials.gov (identifier number NCT00333801). The authors acknowledge the generous support of the Tuscaloosa VAMC's Research and Development Services and the hard work and devotion of the vocational rehabilitation specialists involved in the study, especially Allen Riley, M.A. The authors acknowledge the consultative expertise of Robert Rosenheck, M.D., and the Tuscaloosa VAMC vocational rehabilitation programmatic support of Thomas McNutt, Ph.D., and James Carr. The authors are grateful for the technical assistance of Catherine M. Blansett, Ph.D., Charles Li, Bonita S. Perry, M.S., Laura E. Blackburn, and Jessie McAlpine.
Dr. Davis has received a speaker honorarium and research funding from AstraZeneca. Dr. Leon served on independent data and safety monitoring boards for AstraZeneca, Sunovion, and Pfizer; served as a consultant-advisor to MedAvante and Roche; and had equity in MedAvante. The other authors report no competing interests.