A majority of individuals in the United States with significant mental health needs never receive mental health services (
1). Such needs can cause unnecessary suffering, impairment, and economic loss for the individual as well as society (
2). When those in need of mental health services are parents, these needs are likely to also affect their children and may lead to behavioral and school problems (
3,
4), family violence, and child maltreatment (
5). This study examined predictors of different levels of engagement in mental health services among mothers of children at elevated risk of, and oversampled for, child maltreatment. The overarching purpose of these analyses is to better understand the factors that predict successful and satisfactory engagement in mental health services among high-risk mothers. Such engagement has the potential to improve the functioning and well-being of mothers themselves (
1,
2), and reduce the likelihood of direct and indirect harms to their children by reducing the risk of maltreatment and family violence (
5) and improving parental competence (
3,
4).
Engagement in mental health services can be understood as a multistep process, in which potential patients move through consideration of seeking services to receipt of them. Although engagement in services is a frequent topic of research, few studies look beyond receipt of services and examine whether services are perceived as satisfactory (
6). Factors that predict engagement can operate at different levels of “distance” from the mental health encounter and the particular needs of the individual patient. At the most distal level are demographic factors, such as race-ethnicity and age, which are usually unrelated to mental health diagnoses but may influence utilization patterns. Another “prior factors” level to consider is the patient's prior experiences with mental health services and with social systems more broadly; as with demographic characteristics, patients come in to treatment with these experiences, but patients can further reevaluate these experiences in the context of treatment. Experiences of trauma are likely to influence psychiatric symptoms directly and are more likely to be a focus of therapy. Finally, and perhaps most proximally to decisions about mental health service utilization, a patient's overall functioning is often a key focus of treatment and may influence the course of engagement in services.
Several demographic factors have been examined as predictors of mental health services utilization. Typically, whites are more likely than members of racial-ethnic minorities to use mental health services (
1,
7); this disparity is also a factor among persons with an identified mental health need. There is mixed evidence that age is a factor in predicting service engagement (
1,
7). Higher family income is typically associated with use of services (
1,
8). Single adults typically have lower utilization rates (
9), and persons who have been formerly married (that is, those who are divorced or widowed) have higher rates of service use (
1).
Prior experiences with services may also be important. For example, a strong predictor of future mental health service use is past use (
10). There is also a strong and bidirectional link between mothers' and children's use of mental health services (
11). Whether this association simply indicates a marker of family attitudes toward these services or differences in access and knowledge about services remains unclear. As well, many families receive mental health services through public assistance for child welfare. Indeed, involvement in child welfare programs increases likelihood that parents will use services (
12,
13). Thus, although child maltreatment is a frequent negative outcome of parent mental illness, if this mental illness comes to the attention of child welfare, it can present an opportunity for intervention (
13).
Trauma exposure, particularly history of victimization, is also likely to be a key predictor of service use. In general, victims of violence are more likely to receive mental health services than those without such a history (
14), although there is some evidence that victims of child sexual abuse use services at a lower rate than would be expected (
9). Some research indicates that intimate partner violence strongly predicts use of mental health services (
10,
15).
Finally, and not surprisingly, functioning and well-being predict use of mental health services. Poor mental health functioning is the strongest predictor of services, with the presence of diagnosable mental disorders dramatically increasing the likelihood of mental health services (
1,
16). However, mental health services appear to be facilitated by better overall functioning. Good physical health (
17) and strong social support networks (
18) both increase the likelihood of receiving mental health services.
As noted earlier, most research examining mental health services as an outcome considers it a dichotomy; services were either received or not received. However, service engagement is likely a process that includes different phases of decision making (
19). The act of considering whether to seek services increases the likelihood of later receiving them, even if this process is time consuming (
20). Also, receiving services is distinctly different from engaging in services. In fact, most of the mental health services received do not meet standards of minimal adequacy (
1) and early dropout is common (
21,
22). Satisfaction with services is likely to predict staying in treatment (
21), as well as better clinical outcomes (
23). Thus understanding both consideration of and satisfaction with services is important.
This investigation examined predictors of engagement in services in a large sample of mothers, who were enrolled with their children in a longitudinal study on child maltreatment. Four levels of engagement in services were available for analysis: no services or consideration of services, considering services but not yet receiving them, receiving services and being dissatisfied with them, and receiving services and being satisfied with them. The analyses examined factors distinguishing between three dichotomous pairings at different levels of engagement: those who considered services versus those who did not consider services, those who received services versus those who considered but did not receive services, and those who received services and were satisfied with them versus those who received services and were not satisfied with them.
Methods
Sample and design
Data used in these analyses were collected by the Consortium for Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) (
24). LONGSCANis a consortium of a coordinating center and five study sites, drawn from different geographical regions of the United States. Its mission is to investigate the antecedents and consequences of child maltreatment, and thus there was an oversampling for families reported as maltreating, with different sampling frames at each site. All sites collect data according to the commonly shared protocols at age-specific data collection points. One of the five sites, the Southwest site, selected only children who had been removed from the home and placed in foster care. The female caregivers in this region were primarily foster, rather than biological, parents (who were the caregivers of most children in the other sites). Therefore, the sample used for analysis included four sites and excluded the Southwest site. Each participating study site, as well as the coordinating center, obtained independent approval from their local institutional review board. Caregivers provided informed consent.
Data at each time point were collected from dyads of children and their mothers; data collection occurred when children were four and six years old, as well as at later ages, which are not included in the analyses reported here. Data used in these analyses were collected primarily when children were age six, although some variables were collected when children were age four. Data collection occurred from 1991 to 2001. The data used in these analyses relied in almost all cases on the mother's report, except where noted.
Measures
Participating mothers reported on mental health services they had received in the past year (
25). The analyses here focused on the responses to three questions: “In the past year, did you consider seeking outside help for any emotional problem?” “In the past year, did you see someone for help with an emotional problem?” “How satisfied were you with the services you received from this person? Very satisfied, somewhat satisfied, somewhat dissatisfied, or very dissatisfied.” From these questions, four levels of services engagement were constructed: no services or consideration of services (none), considering services but not yet receiving them (considered), receiving services and being dissatisfied with them (unsatisfied), and receiving services and being satisfied with them (satisfied).
Demographic information for the mothers included race, marital status, age, years of education, and family income. Assessment of previous systems involvement used data collected from two sources: administrative data and mother self-report when children were age four. To determine whether children had been reported to child protective services (CPS), LONGSCAN investigators at each site reviewed state and local CPS records for allegations of maltreatment of the participating children (
26). Because services are frequently offered to families reported to CPS, regardless of whether specific allegations are founded (
12), and because of biases in the process of substantiation of allegations (
27,
28), the analyses included all allegations of maltreatment that occurred before the self-report data collection.
Also, when children were age four, mothers had reported on whether they themselves had received mental health services and whether they had felt they needed such services. They also reported on whether their child received such services and whether they felt that their child needed such services.
Assessment of traumatic exposure relied on self-report by mothers. When children reached age four, mothers completed the Mothers' History of Loss and Harm Scale (Hunter WM, Everson MD, unpublished instrument, 1991) to assess the mother's history of physical and sexual victimization in childhood, adolescence, and adulthood. The questions addressed specific experiences that mothers might have had (for example, “Were you ever physically hurt by a parent or someone else: hit, slapped, beaten, shaken, burned, or anything like that?” “Has anyone ever sexually assaulted or raped you?”). Endorsement of any victimization item resulted in the person's classification as having been victimized.
In addition, mothers reported on recent intimate partner victimization, using the Conflict Tactics Scale—Couple form (CTS) (
29). The CTS measures the frequency of specific acts used by the mothers' romantic partners in response to conflict. Mothers were asked to report on incidents of physical and psychological aggression that had occurred in the prior three months. The CTS was administered only to mothers who reported having a current romantic partner; those without a romantic partner were assigned a level of zero in regard to recent physical and psychological intimate partner victimization.
Assessment of mothers' functioning included depressive symptoms, physical health, and social support. Mothers' depressive symptoms were assessed with the Center for Epidemiologic Studies Depression Scale (CES-D) (
30). Mothers' physical health was assessed with a global question about current health status (rated as poor, fair, good, or excellent), which is one of the most reliable and widely used indicators of physical health functioning (
31). For these analyses, mothers' health status was dichotomized into poor or fair versus good or excellent. Mothers' social support was assessed with a modified version of the Duke-University of North Carolina Functional Social Support Questionnaire (
32).
Analyses
First, descriptive bivariate statistics tests (chi square analyses and analysis of variance) were conducted for the potential predictors across the four levels of service engagement. Next, three logistic regression analyses were conducted to examine predictors of mothers' level of service utilization, defined by four levels of engagement: considering versus not considering services, receiving versus considering but not receiving services, and receiving services and satisfied with them versus receiving services and not satisfied with them. In these logistic regression analyses, all predictors were entered simultaneously.
Results
Potential predictors across four levels of service engagement
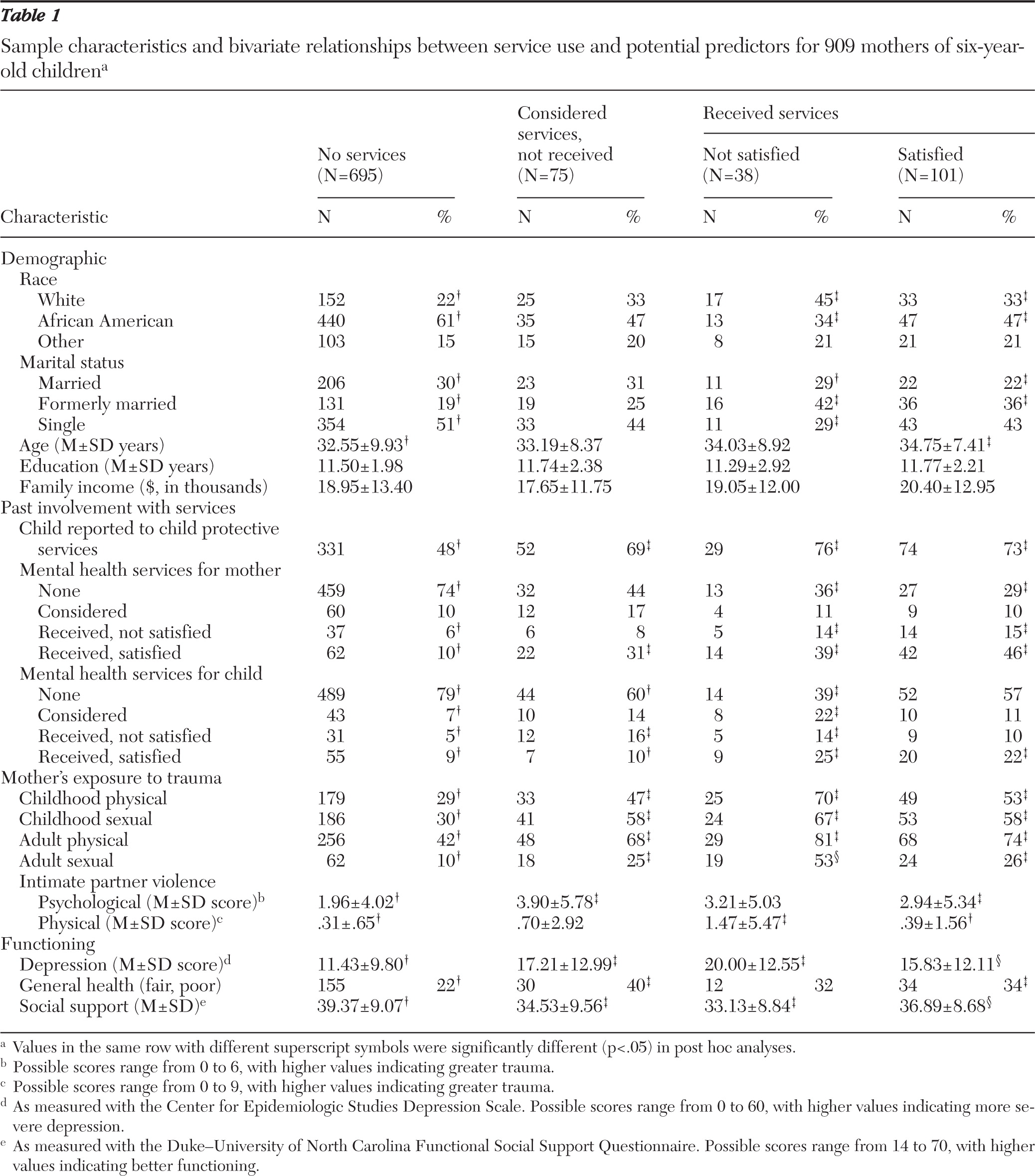
Table 1 presents descriptive statistics for potential predictors across four levels of engagement in mental health services. Demographic information, prior experiences with services, exposure to trauma, and functioning all showed significant bivariate differences across the four levels of service engagement. Of the demographic characteristics, race and marital status were strongly associated with level of service utilization. All of the variables examined in terms of prior system involvement (that is, child welfare involvement, prior mental health services for the mother, and prior mental health services for the child) predicted level of service engagement. In trauma exposure, all examined variables (physical and sexual victimization during childhood and adulthood and physical and psychological intimate partner victimization) were associated with engagement in services. Finally, all indicators of functioning examined (depressive symptoms, general health, and social support) were associated with level of engagement in services. For subsequent analyses (the logistic regression), the variables family income and years of education were not retained because they did not show any significant differences across group membership.
Prediction of mothers' engagement in services
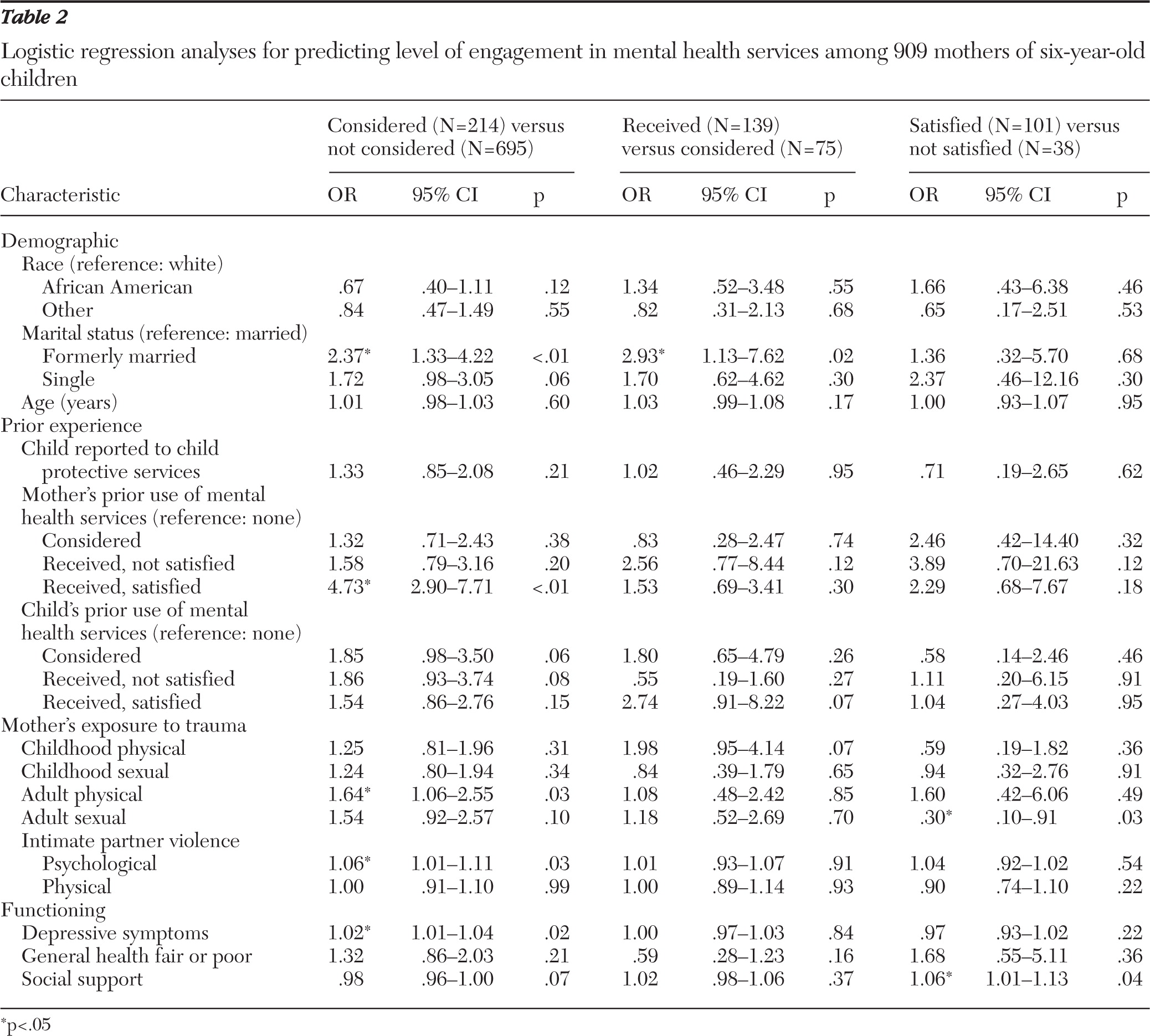
The regression analyses are presented in
Table 2. As indicated, significant unique predictors of considering mental health services included being formerly married (versus married), receiving services previously and being satisfied with them (versus not having received services), having experienced physical victimization as an adult, having experienced psychological victimization by an intimate partner, and higher levels of depressive symptoms.
In contrasting mothers who received services with those who considered but did not receive services, we found only one significant unique predictor: being formerly married (versus currently married). Finally, two factors uniquely distinguished between participants who received and were satisfied with services and those who received services and were not satisfied; mothers who had not experienced sexual victimization as adults were more likely to be satisfied with mental health services, as were participants who reported higher levels of social support.
Discussion
Predictors of mental health services were examined across four domains (demographic characteristics, prior experience with services, trauma exposure, and current functioning) in a large sample of mothers of children at risk of maltreatment. Engagement with mental health services appeared to be determined by multiple factors, with unique contributions from each of the four domains examined, and to vary depending on the stage of engagement.
Several factors, from each of the four domains examined, distinguishedwomen who considered seeking mental health services from those who did not. Two forms of trauma (physical victimization as an adult and psychological intimate partner victimization) were associated with increased likelihood of considering services. Although treatment engagement with trauma survivors can be challenging (
33), it appears that such survivors are, in fact, open to receiving services. One might suppose women who are being emotionally or verbally abused would be less likely to receive external encouragement to get help because there would be less opportunity for intervention than if they went to an emergency department for physical victimization. On the other hand, dissatisfaction in their relationship with their partner may motivate these women to seek counseling, whereas those who have experienced physical victimization may prioritize services that are not primarily mental health focused.
Symptoms of depression were also associated with consideration of mental health services. Formerly married women were more likely than married or single women to consider mental health services, consistent with nationally representative research with a general population sample (
1). It is striking that only one variable distinguished between women who considered mental health services and women who received such services. It is possible that practical barriers to services are a key determinant (
6), and we did not examine practical barriers. Alternatively, this finding may be related to power issues or because a cluster of covarying factors predicted receipt of services. In particular, the effects of physical victimization in the mother's childhood approached significance in these analyses.
Satisfaction with services was associated with two factors: lower rates of adult sexual victimization and high levels of social support. Prior research has suggested the positive role that social support can play in facilitating successful mental health treatment (
18). The finding that women with recent sexual victimization were especially unlikely to be satisfied with mental health services is provocative. One area of future investigation is the way that such victimization interacts with therapist characteristics, such as gender, as well as with types of mental health services to predict client engagement. Perhaps mothers who experience adult sexual victimization by men are less inclined to be satisfied with male treatment providers. Similarly, women receiving group therapy may be less satisfied with these services if they are uncomfortable disclosing trauma in a group setting. Finally, the services received may not be focused on trauma. Qualitative research has suggested that women with trauma histories that are not addressed by their therapists tend to be dissatisfied with treatment (
6).
In considering these results, it is important to keep in mind several limitations of this study. First, in comparing this study with other studies of mental health service utilization, it is important to note that the LONGSCAN studies oversampled for exposure to trauma and child welfare involvement. This is understandable, given that the focus of the LONGSCAN studies was child maltreatment, but it should lead to some caution in interpreting the results. Also, given the child welfare focus, the research participants were more likely than the general population to have low incomes and to be members of racial-ethnic minorities, especially African Americans. Perhaps for these reasons, the respondents reported lower rates of service use than samples in the general population (
1) and other high-risk samples (
10). Finally, the subgroups among the women who considered services were relatively small, influencing power to detect effects. Power may also have been an issue overall, given the number of variables examined.
Another set of caveats relates to the assessment of the variables in the study. Like most research in this area, these analyses relied on self-report of service utilization. Such self-reports are typically valid (
34) but should be viewed as provisional. Most of the predictors (history of victimization and previous use of services) were also assessed via self-report. Finally, it is important to keep in mind that we assessed satisfaction with mental health services, which is a proxy indicator of engagement or persistence in treatment. Quality or effectiveness of services is an important area for future examination.
Conclusions
With these limitations in mind, there are several conclusions that can be drawn from this research. First, it is important to highlight the need to be broader in the assessment of mental health services. Recent research has highlighted the importance of examining adequacy of (
35) as well as satisfaction with services (
6). Given the differences found among those who received satisfactory treatment, those who received unsatisfactory treatment, and those who only considered treatment, this investigation underlines the need for research to move beyond the dichotomy of receipt versus nonreceipt of mental health services as an outcome (
6).
This research identified, in addition to those who did not seek services, those who reported receipt of unsatisfactory treatment and those who considered treatment but did not receive it. Implicit in this way of assessing treatment is the notion that satisfactory treatment is the goal. Women who have experienced recent physical victimization or significant intimate partner conflict, as well as women with depressive symptoms, are likely to consider receiving mental health services. This consideration may be fostered through motivational interviewing or referral to mental health services by their general medical contacts.
Few factors distinguished between mothers who considered services and those who received them, suggesting that more work is needed in understanding the process by which those contemplating services actually receive them. Practical barriers such as child care, cost, and distance from treatment sites, may be key factors (
6). Mothers with high levels of social support were likely to be satisfied with the mental health services they received, suggesting that social functioning may be an important metric by which they evaluate the effectiveness of services. Health care providers would likely benefit from asking about social support and engaging patients' social networks. Finally, women with recent sexual trauma were especially unlikely to be satisfied with the mental health services they received. This suggests the importance of tailoring interventions for women who have experienced such trauma with a focus on their perceived needs (
9). Given the high number of women with prior child welfare involvement in this sample, these findings also highlight that comprehensive needs assessments are necessary, not simply for child victims of maltreatment, but for their mothers as well.
Acknowledgments and disclosures
This research was supported by grants to the Consortium for Longitudinal Studies of Child Abuse and Neglect (LONGSCAN) from the Children's Bureau, Office on Child Abuse and Neglect, Administration for Children, Youth, and Families.
The authors report no competing interests.