Housing programs for people with severe mental illnesses aim to maximize community integration (
1,
2). Community integration has been conceptualized as multidimensional (
1), involving physical, social, and psychological dimensions. As so defined, community integration is related to both subjective (
3) and objective (
4) outcomes that are associated with recovery. Whereas the subjective components of community integration are related to perceived belonging and sense of community, objective dimensions concern behavior and include physical integration (participation in local activities) and social integration (interactions with community members) (
1), as well civic participation or “citizenship” (for example, voting or volunteering) (
5). Independent scatter-site housing (also known as supported housing) has become increasingly common (
6) and is intended to maximize opportunities for community integration (
7).
Little is known about how the community integration of mental health consumers living in supported housing compares with that of other community residents in the socially disadvantaged communities where supported housing is often located. There is reason to expect that social disadvantage compromises opportunities for community participation among all residents, given evidence that poverty and neighborhood disorder are associated with diminished social participation and psychological community integration (
8,
9). One strategy for addressing this issue is to compare the community integration of mental health consumers with that of residents of the same communities who are not mental health consumers. In previous research that used community members as a control group, one study found that the social integration of mental health consumers, but not physical and psychological integration, was lower than that of matched community members (
10). More recently, Abdallah and colleagues (
11) found that older adults with schizophrenia had lower psychological, social, and physical integration than matched adults in a community control group. Neither of these studies, however, focused on mental health consumers living exclusively in supported housing.
Previously, we reported that the subjective community integration of people with severe mental illnesses living in supported housing did not differ from that of other community members living in the Bronx, New York (
12). The study reported here built on our earlier report and examined the predictors of objective community integration (physical and social integration and citizenship) of mental health consumers living in supported housing and of other community members.
Methods
Setting
Participants were recruited from neighborhoods in the Bronx, New York, where mental health consumers lived. Participants with severe mental illnesses were housed through a supported housing program that provides mental health services (either assertive community treatment or supportive case management) off site. Off-site services aim to support consumers in their efforts to live independently and adjust to community living. Housing consists of apartments that are subleased to the consumers through the agency and that are located in regular rental buildings. Although the agency sometimes houses more than one consumer within a building, the agency avoids renting more than 15% of the units in a given building so that consumers remain interspersed with other community members.
Most Bronx residents are Hispanic (52%). They tend to have lower incomes than other New York State residents (2010 median household income of $32,568±$1,393, compared with a state average of $54,148±$376) (
13). Participants were recruited from zip codes 10451–10453, 10456–10459, 10466–10468, and 10470, which correspond to neighborhoods in south and north central Bronx. Nearly identical numbers of consumers and community members were recruited from each zip code, with only a few exceptions (for example, seven consumer participants and six community participants were recruited from 10468, whereas five community participants and four consumer participants were recruited from 10456). Zip codes in these neighborhoods typically cover an area of roughly 10×10 city blocks. Areas covered by these zip codes are densely populated and feature a mixture of housing—90% apartment buildings, with a small number of town homes and single-family homes (
13)—stores, and parks. These communities are generally poor, even compared with the overall Bronx median income; the median income of these communities is $24,681±$6,282 (range $16,664 to $38,464), and a mean±SD of 35.00%±8.67% of residents live below the poverty level (range 14.5% to 44.9%) (the overall Bronx average was 30%±1% in 2010).
Procedures
Institutional review board approval was received for the study, and data were collected between January and June 2009. English-speaking mental health consumers living in the Bronx and receiving services from the supported housing program were considered eligible for the study. Potential participants were approached through the field offices of the supported housing program, as well as through treatment team members, who were asked to distribute study flyers to eligible participants. After they gave informed consent, interested individuals were then interviewed either at a program location or their apartment. Because participants were approached through flyers, we cannot directly estimate the number of “refusals” (only one individual directly refused to participate). In addition, active recruitment was halted after the study reached its recruitment goal of 60. According to program records, 56% of clients who were potentially eligible (that is, who were program clients and lived in the Bronx) participated in the study.
Participants for the community sample were recruited via flyers handed out at public locations (for example, in front of subway stations) in the areas where the mental health consumers resided. All community members expressing interest first completed a brief screening to determine that they did not have a significant psychiatric history (for example, any past psychiatric hospitalization or current receipt of services such as day treatment, case management, or assertive community treatment) and that they lived in independent housing (that is, not in a shelter or residential drug treatment program) and in one of the targeted study zip codes that matched with the consumer group. After completing informed consent, eligible participants were then interviewed at a convenient location. Fifteen community members' interviews were subsequently excluded because there was evidence that the participant had a psychiatric disability (for example, he or she received Supplemental Security Income for mental health reasons), did not live in one of the targeted zip codes, or did not live in independent housing.
Participants
Participants were 124 English-speaking adults. Sixty of the participants (48%) were adults diagnosed as having severe mental illnesses who were residing in supported housing, and 64 (52%) were other community residents without severe mental illnesses residing in the same zip codes as the mental health consumers.
Measures
Demographic and background variables, including age, race-ethnicity, education, criminal justice involvement, income, and employment history, were assessed by self-report.
The Colorado Symptom Index (CSI) is a 15-item self-report scale that measures psychopathology by assessing the frequency of experiencing symptoms (including psychotic symptoms) in the past month (
14). In this sample, an overall Cronbach's alpha of .76 was observed, although the alpha among the mental health consumer sample was .79 and a much lower alpha of .49 was observed in the community sample. The Center for Epidemiologic Studies-Depression Scale (CES-D), a 21-item measure, was used to assess depressive symptoms in the past week (
15). A relatively low Cronbach's alpha of .49 was observed for the CES-D for the overall sample, and alphas were even lower when we examined them separately by sample: .49 for the consumer sample and .19 for the community sample. CES-D scores achieved acceptable internal consistency (.74 for the consumer subset and .66 for the community subset) when the four reverse-scored positively worded items were excluded. Findings are therefore reported for the 17-item version of the CES-D.
Current substance use was assessed with the section of the Addiction Severity Index that addresses recent substance use (
16); it assesses use of a variety of substances in the previous 30 days. Two subscales were derived from this measure: a drug use scale, which sums the number of days that a variety of illegal drugs were used, and an alcohol scale, which sums the number of days for both alcohol use and alcohol intoxication.
Established measures that have been used in several previous studies (
11,
17) were used to measure physical and social community integration. Physical community integration was measured with the External Integration Scale (
18), which is a 12-item self-report scale assessing the number of days in the past two weeks that the individual spent in a variety of activities outside his or her household (for example, attending religious services or walking in a park). Cronbach's alphas for the scale were .73 for mental health consumers and .74 for community residents. Social community integration was assessed with a 12-item scale that assesses the frequency of interactions between the participant and community members, such as borrowing or lending items and going on a social outing (
10). Internal consistency was excellent for this scale (.85 for the consumer sample and .90 for the community sample).
Because no measure had yet been validated to assess citizenship among people with severe mental illnesses, we identified a measure—the Social Capital Survey Short Form (
19)—that closely taps into aspects of the construct as discussed by Ware and colleagues (
5), including involvement in activities such as political activism or volunteering during the past year. We found this scale to have acceptable internal consistency overall (Cronbach's
α=.65) and among the community sample (.73), but internal consistency was lower for the consumer sample (Cronbach's
α=.48).
Analyses
Mean differences between the two groups in objective community integration and symptoms were first assessed with analysis of variance. We then examined Pearson and Spearman correlations, where appropriate, between study variables separately for each subgroup. Finally, we conducted simultaneous linear regressions predicting objective community integration for the overall sample.
Results
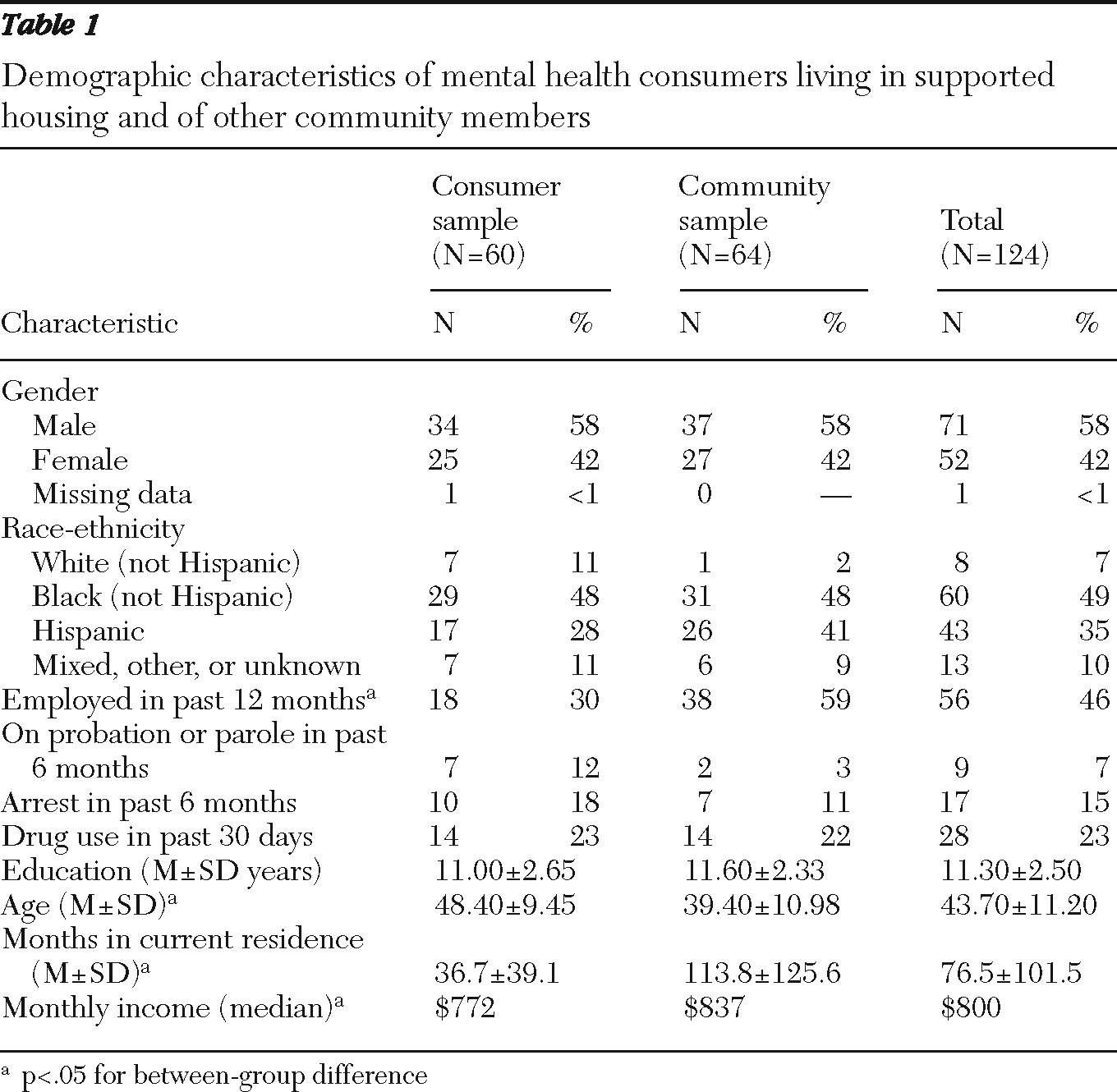
Demographic characteristics of the two participant groups are shown in
Table 1. The two groups did not differ significantly in gender, race-ethnicity, education, recent criminal justice involvement, or recent drug use; however, mental health consumers were significantly older and had lived in their apartments for significantly less time (roughly three years compared with nearly ten years for the community sample), were significantly less likely to be currently or recently employed, and earned significantly lower monthly incomes. Most participants were men and African American or Hispanic, had less than a high school education, and were living in poverty (their monthly incomes were consistent with roughly $10,000 annual incomes). A substantial minority of participants from both groups reported recent illegal drug use, and a small number had recently been arrested or were on probation or parole.
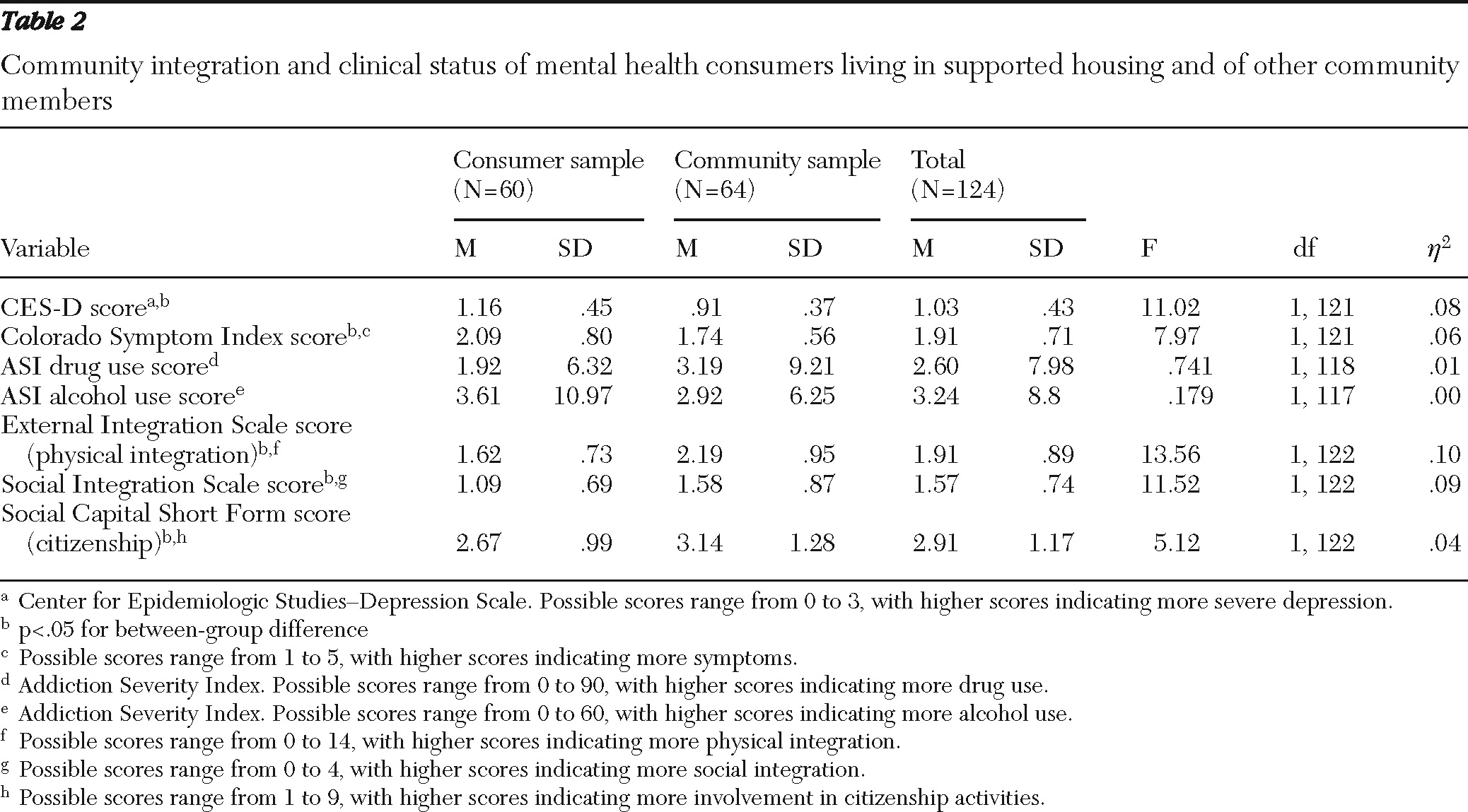
Table 2 presents means for community integration, psychiatric symptoms, and citizenship for the two samples. The two samples differed significantly on all three of the community integration variables; mental health consumers had lower mean scores in physical integration, social integration, and citizenship activities. For physical integration—the number of days in the past two weeks on which the person was involved in activities outside of his or her household—mental health consumers reported half a day less than persons in the community sample. Similarly, mental health consumers were half a point lower on the scale of social integration; this indicates that they typically responded that they engaged in activities with neighbors rarely, whereas those in the community sample were at the midpoint between rarely and occasionally. For citizenship activities, consumer responses ranged between “once” and “a few times” in the past 12 months, whereas community members' responses tended to be “more than a few times.” Differences between the two groups on all three variables were on a magnitude of roughly half of a standard deviation.
Consumers reported more depressive symptoms and psychiatric symptoms overall than reported by community members (
Table 2). On average, mental health consumers reported that they experienced the symptoms listed in the CSI once during the month, whereas community members' responses were between “not at all” and “once during the month.” Scores for the consumer sample, on average, met criteria for the overall score of 30, which is the cutoff for clinically significant symptoms (which is comparable to the item mean of 2 that we observed) discussed in previous research (
20). Consumers and community members did not differ significantly in recent alcohol or drug use.
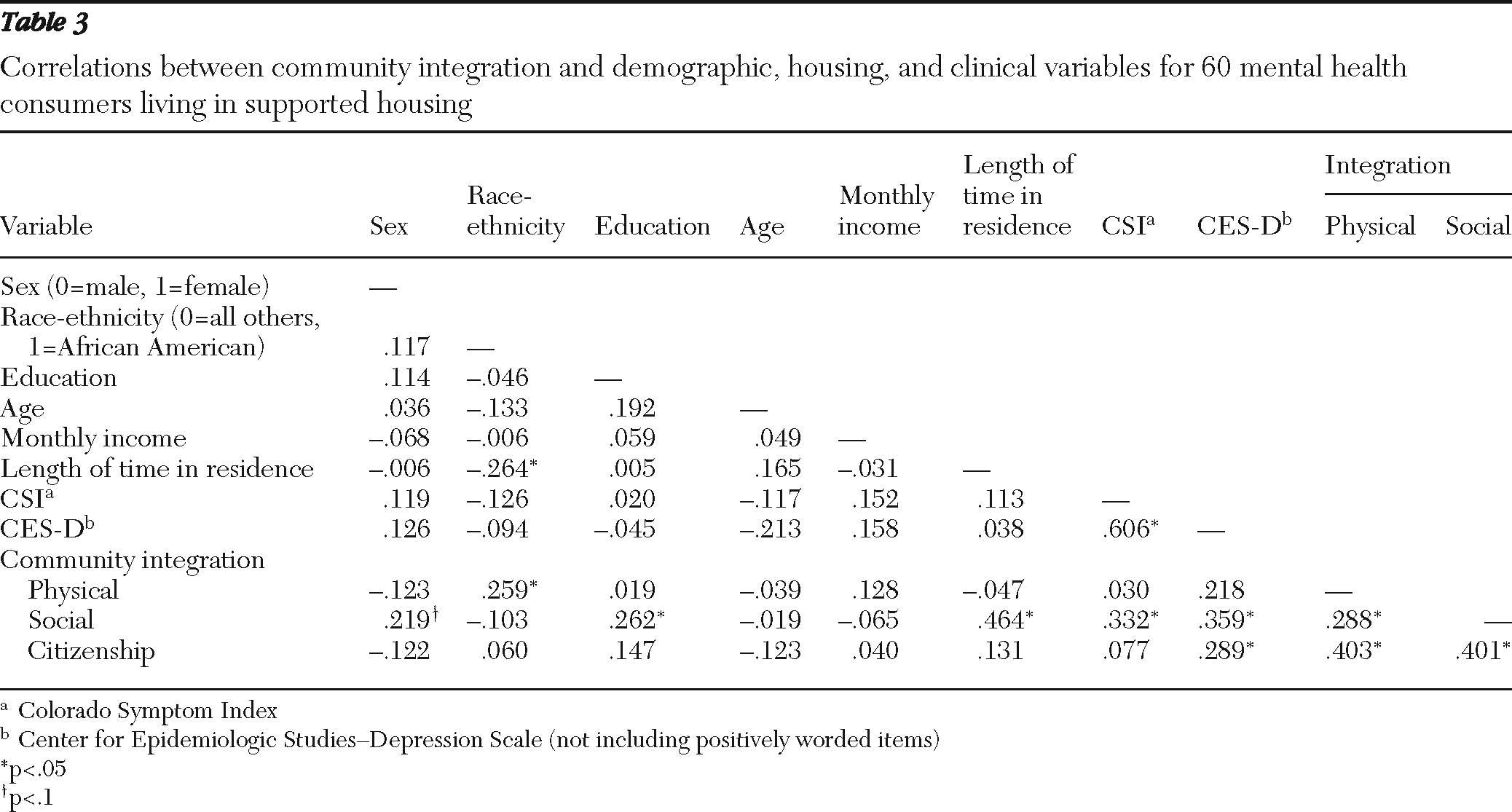
Table 3 presents correlations between demographic, housing, psychiatric, and community integration variables in the consumer sample only. We contrasted African-American participants with all others on the basis of prior evidence that African Americans with severe mental illnesses tend to have better community integration (
21). The three aspects of community integration were significantly correlated with one another, but physical and social integration were weakly correlated and physical and social integration showed moderate correlations with citizenship. The only variable significantly associated with physical community integration was African-American race, which was associated with higher physical integration scores. Social integration was significantly associated with demographic, housing, and psychiatric factors. Among the demographic factors, education was positively associated with social integration scores, and length of time in current apartment had a strong significant association with social integration. Symptoms as measured by the CSI and depressive symptoms as measured by the CES-D were both significantly associated with social integration; however, the direction of the relationship was opposite to what might be expected—more symptoms were associated with better community integration. Citizenship was not significantly associated with any variables, with the exception of CES-D score; however, this was again in the unexpected direction. Income was not significantly associated with any of the community integration variables.
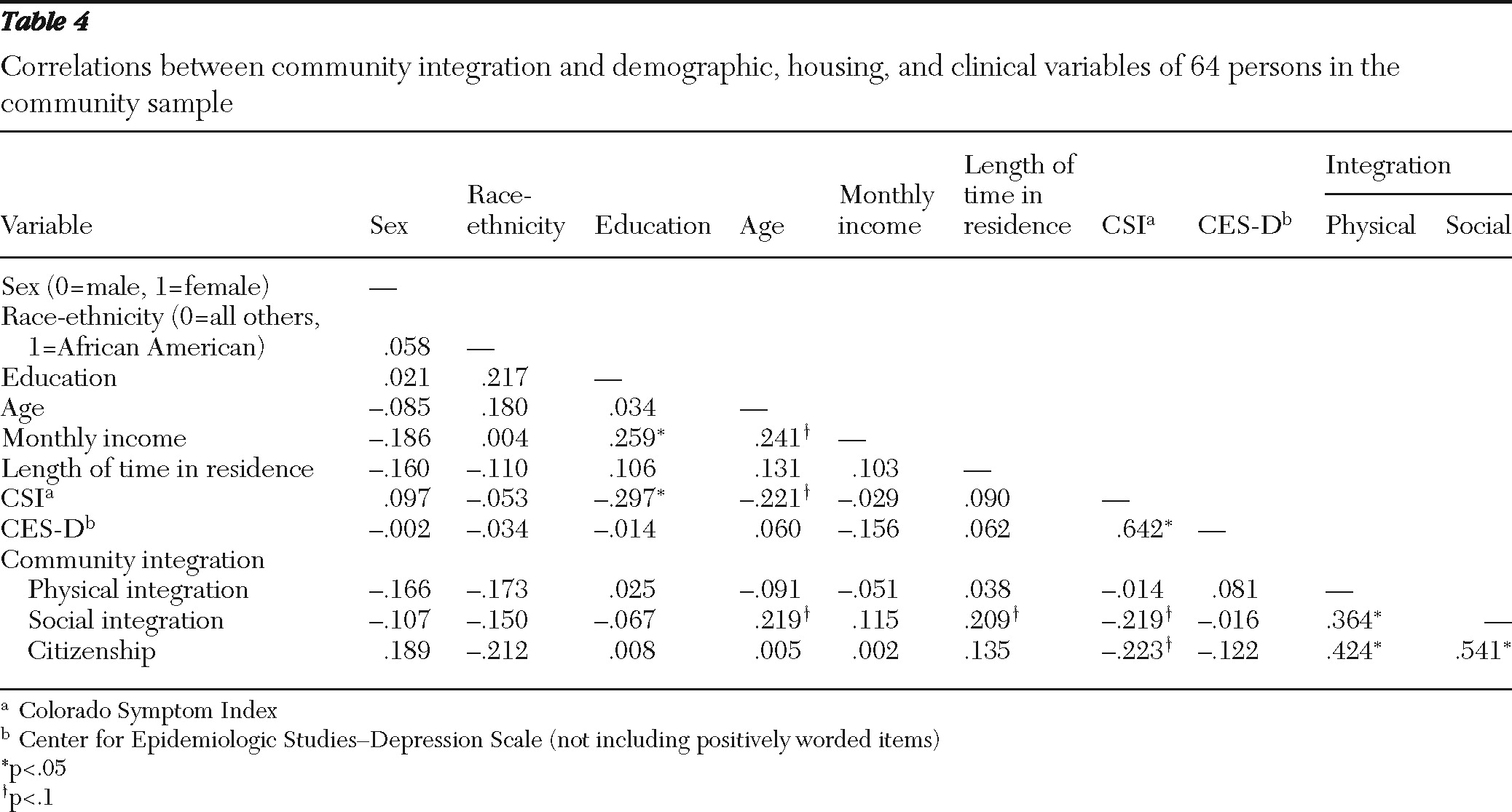
Table 4 presents correlations between demographic, housing, psychiatric, and community integration variables in the community sample only. The three aspects of community integration were again significantly correlated with one another, and correlations tended to be stronger than among the consumer sample, although physical and social integration were again more weakly correlated with each other than with the other variables. None of the demographic or psychiatric variables were significantly associated with the community integration variables in the community sample, although there was a trend for length of time in residence to be associated with social integration and trends for psychiatric and depressive symptoms to be negatively associated with social integration and citizenship (associations in this case were in the expected direction).
We conducted a series of simultaneous regressions to explore whether differences in community integration between the two samples could be explained by any of the demographic and psychiatric differences between them. For these analyses, we included group (community=0, consumer=1) and the variables on which the groups significantly differed in the bivariate analyses and that showed evidence of being associated with community integration in the correlation analyses (length of time in current residence and CSI and CES-D scores were excluded because of the possibility that it might be collinear with the CSI). We entered the three variables into simultaneous regression equations predicting social integration, physical integration, and citizenship. The overall equation was significant in predicting social integration (R2=.138, F=6.36, df=3 and 119, p=.001). Inspection of variables that were uniquely predictive of social integration indicated two significant variables: length of time in current residence (β=.244, t=2.64, p=.009) and group (β=−.343, t=−2.18, p=.03). The overall equation was significant in predicting physical integration (R2=.095, F=3.08, df=3 and 119, p=.008). Inspection of variables that were uniquely predictive of physical integration indicated that only group was significant (β=−.302, t=−3.09, p=.002). For citizenship, the overall equation was not significant, and none of the variables, including group, were significant predictors in the equation.
Discussion and conclusions
Several interesting findings emerged from this study. First, we note that in contrast with our prior finding that mental health consumers did not differ from other community members in subjective indicators of community integration (
12), mental health consumers living in supported independent housing had significantly lower scores on indicators of objective community integration than other community members. This finding is generally consistent with findings from previous studies of mental health consumers and other community members (
10,
11). However, differences were relatively small, and on the whole, community integration was low for both groups. This finding may reflect the fact that both groups had similar educational and racial-ethnic backgrounds, which may indicate similarities in culture and lifestyle. Both the consumer and community samples met objective criteria for poverty and lived in disadvantaged communities, which also may have restricted the range of possibilities for community integration.
Some interesting findings emerged regarding psychiatric symptoms. First, as expected, consumers reported more symptoms than other community members. However, symptoms did not explain differences between the community members and mental health consumers in any of the community integration outcomes, and, in fact, associations between symptoms and community integration were in the opposite direction in the consumer sample (more symptoms were associated with better social integration). Although this finding is counterintuitive, it was also observed in a previous study, which found that symptoms reported on the CSI had a significant positive relationship to social integration (
22). It is possible that this reflects a tendency for participants who experience more anxiety and depressive symptoms to more readily seek out social interaction as a source of support. To explore this possibility, we conducted supplementary analyses of subscale associations between the CSI and social integration and found that the relationship between social integration and symptoms was largely driven by nonpsychotic symptoms. It is also possible that the self-report approach to assessing symptoms, although well validated in previous research (
20), is flawed in that it does not assess “negative symptoms,” which might have a more profound effect on social functioning than self-reported psychotic, anxiety, and depressive symptoms. The inclusion of rating scales that are able to assess the severity of negative symptoms in future research might help to disentangle this issue.
Among mental health consumers, we replicated a previous finding that African-American race and education are both associated with better community integration (
21). Another notable finding was that length of time in current residence was a significant predictor of social integration among mental health consumers. This underscores that longevity and familiarity with one's neighborhood may facilitate interaction with neighbors. Furthermore, when we examined variables that explained differences in the community integration outcomes between the two groups, we found that length of time in current residence accounted for a significant proportion of the variance, although it did not wholly explain the difference between the two groups.
We found that no variables were significantly associated with citizenship in the regression equation, and on the whole, findings with regard to this variable were disappointing. We note that although the concept of citizenship as a component of community integration among persons with severe mental illnesses has been previously discussed (
5), the measure that we used had not been previously used in this context. It is possible that another measure that is more focused on types of citizenship participation that are more culturally and economically relevant to this population (for example, volunteering in a church program or in mental health organizations and leadership in self-help groups) might provide a more useful measure of citizenship.
Although our findings of variables that are predictive of community integration are similar to those of Wong and colleagues (
21), our findings were not consistent with those of Abdallah and colleagues (
11), who found that gender and income were both positively associated with overall community integration and that symptom severity (as measured by a rating scale and the CES-D) were both negatively associated with community integration (in contrast with our sample, in which a higher level of symptoms was positively associated with community integration). Some important differences between our studies should be noted. Our study included a mixed group of mental health consumers with a variety of ages living only in supported housing, whereas the study by Abdallah and colleagues (
11) included only older adults with a diagnosis of schizophrenia and included individuals living in a variety of housing settings. In addition, they did not use previously established scales to assess community integration; instead they used a variety of items from other scales as “proxy” measures. These methodological and sampling differences may account for some of the discrepancies in our findings.
Some implications of the study findings should be noted. Our overall finding suggests that mental health consumers living in supported independent housing have the potential to achieve community integration outcomes that are at least close to what other community members achieve. Our findings with regard to specific variables associated with community integration suggest that symptoms are not a major factor in impeding community integration but that other factors, such as length of time in a given area, are important predictors. This suggests that mental health consumers need to be allowed the opportunity to adjust to new environments whenever possible. It also suggests that housing mental health consumers in communities where they have existing social connections may also be beneficial. When consumers enter housing programs, they are often homeless and are quick to accept the very first apartment that becomes available. Consumers might be advised to wait until an apartment in a neighborhood where they have existing ties is identified, given the long-term implications of this decision.
Our study also had important limitations. The community sample was recruited through a convenience sampling approach and does not necessarily represent community members in the areas that we studied. Furthermore, although we were able to match other community members to mental health consumer participants on zip code of residence, we were not able to match on other demographic variables and, in fact, found that the community members were generally younger and had lived in their communities for significantly longer. In addition, we lacked data specifically on the type of housing in which community participants resided, and it is possible that some may have lived in houses or other types of housing not wholly comparable with that of consumer participants. Future research should seek to match participants on these key variables. It is also possible that other factors not measured in this study were associated with longer residence in a particular community (for example, the presence of relatives), which may explain why this variable significantly predicted social integration. Future research should seek to examine the role that existing family resources play in predicting both housing tenure and community integration. Finally, we found that some of the scales that we used (including the CSI and the citizenship scale) had suboptimal psychometric properties, which may have restricted our ability to detect a relationship for these variables.
Acknowledgments and disclosures
This work was supported by funding from the National Institute of Mental Health's Center to Study Recovery in Social Contexts (P20 MH078188). The authors thank Mike Tamburino, M.A., Laura Kurzban, M.A., Natalie Hornak, M.A., and LeKisha Mixon, M.A., for their research assistance.
Dr. Yanos provides consulting services to Pathways to Housing, which provides supported housing services. The other authors report no competing interests.