An estimated 80% of youths with mental health needs go untreated (
1). Racial disparities in mental health service use have been well documented, with youths from racial-ethnic minority groups more likely than non-Hispanic whites to have unmet need. For example, in a nationally representative sample of American families, Hispanic children were more than twice as likely to have unmet mental health need relative to non-Hispanic white children (
1). Among children in contact with public sectors of care, African-American and Asian-American children were about one-half as likely to use mental health services as non-Hispanic white children, even after analyses accounted for demographic variables and mental health need (
2).
Although overall racial and ethnic disparities are concerning, more recent research suggests that service use pattern may vary by type of presenting problem. Youths with externalizing problems (such as disruptive behavior) are more likely than youths with internalizing problems (such as depression or anxiety) to receive mental health services (
3). In fact, racial disparities appear to be less pronounced for externalizing need, with African-American (46%) and Hispanic youths (48%) having service use rates similar to non-Hispanic white (55%) youths (
4). With controls for demographic and need variables, African-American youths were more likely than non-Hispanic white youths to receive specialty mental health services in response to externalizing symptom severity (
4). Racial disparities appear to be more pronounced when considering internalizing need, with non-Hispanic white youths having higher rates of service use (72%) compared with Hispanic youths (41%). Rates for African Americans (56%) fall between those of their counterparts (
4).
Youths who come into contact with the child welfare system are at high risk of internalizing and externalizing problems, with nearly 50% having clinically significant emotional and behavioral problems (
5). Fortunately, contact with the child welfare system appears to facilitate access to mental health services, particularly in the initial months after a maltreatment investigation (
6). However, access to services is determined by a host of individual, family, and systemic factors. For example, children referred for allegations of abuse (versus neglect) and children who are taken out of the home (versus those who remain in the home) are more likely to receive mental health services (
5). Prior research has found that African-American youths (compared with non-Hispanic whites) who come into contact with the child welfare system continue to be less than one-half as likely to receive mental health services, even after analyses account for demographic characteristics, maltreatment history, and mental health need (
5). Leslie and colleagues (
7) found that racial disparities in service use appear to be most pronounced at lower levels of clinical need when children remain in the home but that disparities persist across the range of severity for children placed in foster care.
Mental health service use is likely influenced by multiple factors that converge to create problem-specific disparities in unmet need. Youths rarely self-refer for treatment and, as a result, service use is largely dependent on the ability of adult gatekeepers of mental health services to identify youths’ needs and link them to services. Caregivers play a prominent role in this process, but barriers such as heightened concerns about stigma, lack of access to linguistically appropriate services, and culturally influenced perceptions of mental health problems or the need for services may set a relatively high threshold for seeking services (
8–
10).
Disparities in mental health services may also be due to system-level factors that actually promote receipt of services for youths from racial-ethnic minority groups. Youths from minority groups are overrepresented in the child welfare and juvenile justice systems (
11,
12), where externalizing problems are closely scrutinized. Awareness of disruptive behavior problems is important within the child welfare system given that these problems are robust predictors of placement instability (
13) and represent highly visible indicators of need relative to internalizing problems. It is also important to consider that institutional bias may affect identification of needs in specific ways. For example, some studies suggest that teachers have a greater tendency to perceive externalizing problems among African-American youths (
14–
16) and African-American youths are more likely than non-Hispanic white youths to receive disciplinary action for disruptive behavior in school (
17,
18). In contrast to caregivers, teachers of African-American students perceive more externalizing problems (
19). Similarly, results from a large sample of youths in care suggest that even after demographic factors and impairment were controlled for, African-American youths were more likely than non-Hispanic white youths to be diagnosed as having a disruptive behavior disorder, although no racial-ethnic differences were noted in parent-rated externalizing problems or clinician-rated impairment (
20). Given that externalizing problems are more distressing to others and are more easily identified by adult gatekeepers relative to more subtle internalizing problems (
21,
22), there may be a particularly high threshold for identifying internalizing mental health needs of youths from racial-ethnic minority groups.
This study examined whether race-ethnicity moderates the association between type of mental health need (internalizing versus externalizing) and mental health service utilization for youths in contact with the child welfare system. We extended prior research by specifically focusing on racial-ethnic disparities by problem type and by examining service use prospectively for one year. We hypothesized that youths from racial-ethnic minority groups are more likely than non-Hispanic white youths to receive services for externalizing problems and that African-American and Hispanic youths are less likely to receive mental health services for internalizing problems relative to non-Hispanic white youths.
Methods
Participants
The National Survey of Child and Adolescent Well-Being (NSCAW) is a national probability study of over 5,500 children who were reported to child welfare agencies as possible victims of maltreatment. For the study reported here, participants (N=1,693) were non-Hispanic white (54%, N=910), African-American (29%, N=485), and Hispanic youths (18%, N=298) who remained with the same caregiver for the first 12 months after the close of the child welfare investigation and who were ages four to 14 (mean±SD age=8.9±3.2 years) at the initial interview. The median annual household income for families was $20,000–$25,000.
Procedure
Initial interviews were conducted two to six months after the close of the child welfare investigation. Demographic characteristics, alleged type of maltreatment, placement type, and caregiver report of mental health need were assessed during the initial interview. Youths age 11 or older also provided self-reports of mental health need at this time. Service use was assessed prospectively via caregiver interviews conducted 12 months after the close of the investigation.
Caregivers and caseworkers provided consent for their participation, and signed consent for the child’s participation was obtained from the person who had the legal authority to do so. Children age seven and older also provided assent. The NSCAW study received approval from the Research Triangle Institute’s Institutional Review Board (IRB) and from IRBs from four states and five additional NSCAW consortium institutions. The use of secondary data for this study was approved by the University of California, Los Angeles, IRB.
Measures
The demographic variables included child’s age and sex and family annual household income. The alleged type of maltreatment resulting in the investigation was obtained from child welfare agency workers responding to a modified version of the Maltreatment Classification Scale (
23). For this study, maltreatment type was coded as active abuse (physical, sexual, and emotional abuse) versus neglect (all forms). Placement type, also obtained from agency workers, was coded as being outside the home (including foster care, group home, or residential treatment) or remaining in the home. Mental health need was defined as having an internalizing or externalizing broadband T score ≥64 on either the Child Behavior Checklist (
24), completed by caregivers, or the Youth Self-Report (
24), completed by youths age 11 and older. Finally, service use was assessed with an adapted version of the Child and Adolescent Services Assessment (
25), which was completed by caregivers. Outpatient mental health service use was defined as any use of clinic-based specialty mental health services, private practice specialists, in-home mental health services, and therapeutic nursery or day treatment services in the 12 months after the close of the child welfare investigation.
Data analysis
Stata, version 12 (
26), was used to account for the complex survey design. All analyses used sampling weights to yield national estimates for the population of children involved with the child welfare system. Chi square tests and analyses of variance were used to examine potential racial-ethnic differences across study variables. Hierarchical logistic regression models were used to predict outpatient mental health service use. In the first step of each model, we entered the following independent predictors: youth’s age, sex, household income, placement type, race-ethnicity, alleged type of maltreatment, internalizing need, and externalizing need. To examine whether race-ethnicity moderated the association between mental health need and service use, interaction terms were added to the model in the second step.
Results
Descriptive statistics for study variables are presented in
Table 1. Compared with non-Hispanic white youths, African-American and Hispanic youths had lower median annual household incomes. Hispanic youths were younger than African Americans. Finally, African-American youths were significantly less likely to receive mental health services relative to non-Hispanic white youths. All other study variables did not differ on the basis of youths’ race-ethnicity (
Table 1).
Results from logistic regression analyses predicting mental health service use are presented in
Table 2. In step 1, children placed outside the home and children investigated because of allegations that they had been abused (versus neglected) were more likely to receive mental health services in the 12 months after initial contact with the child welfare system. Both internalizing and externalizing mental health need predicted service use in the overall sample. These multivariate analyses also suggested that African-American youths continued to be less likely than non-Hispanic white youths to receive mental health services, even after analyses controlled for demographic characteristics, maltreatment history, and mental health need.
In step 2, we tested whether race-ethnicity moderated the association between type of mental health need and service use. As seen in
Table 2, race-ethnicity did not significantly moderate the association between internalizing need and service use.
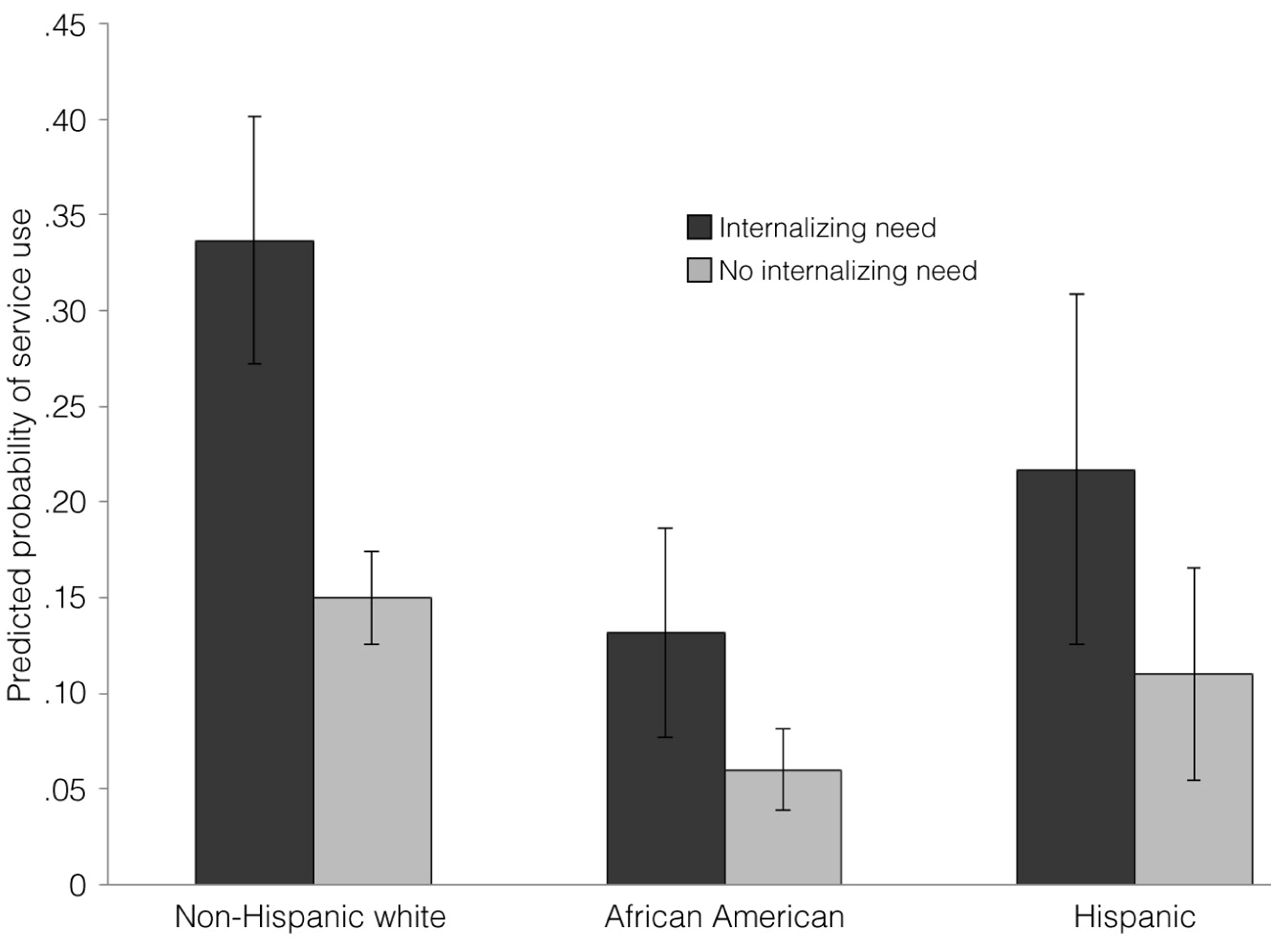
Figure 1 presents the predicted probability of service use as a function of the youth’s race-ethnicity and the presence versus absence of internalizing need, while all other predictors were controlled for. Race-ethnicity was not a statistically significant moderator of the association between internalizing need and service use. However, non-Hispanic white youths were the only group that had a significantly higher probability of using services when internalizing need was present versus absent (34% versus 15%, p=.008). The probability of service use when internalizing need was present versus absent did not differ significantly for African-American (13% versus 6%) and Hispanic (22% versus 11%) youths.
Consistent with study hypotheses, race-ethnicity moderated the association between externalizing need and service use for African-American youths compared with white youths (B=1.31, SE=.65, p<.05.
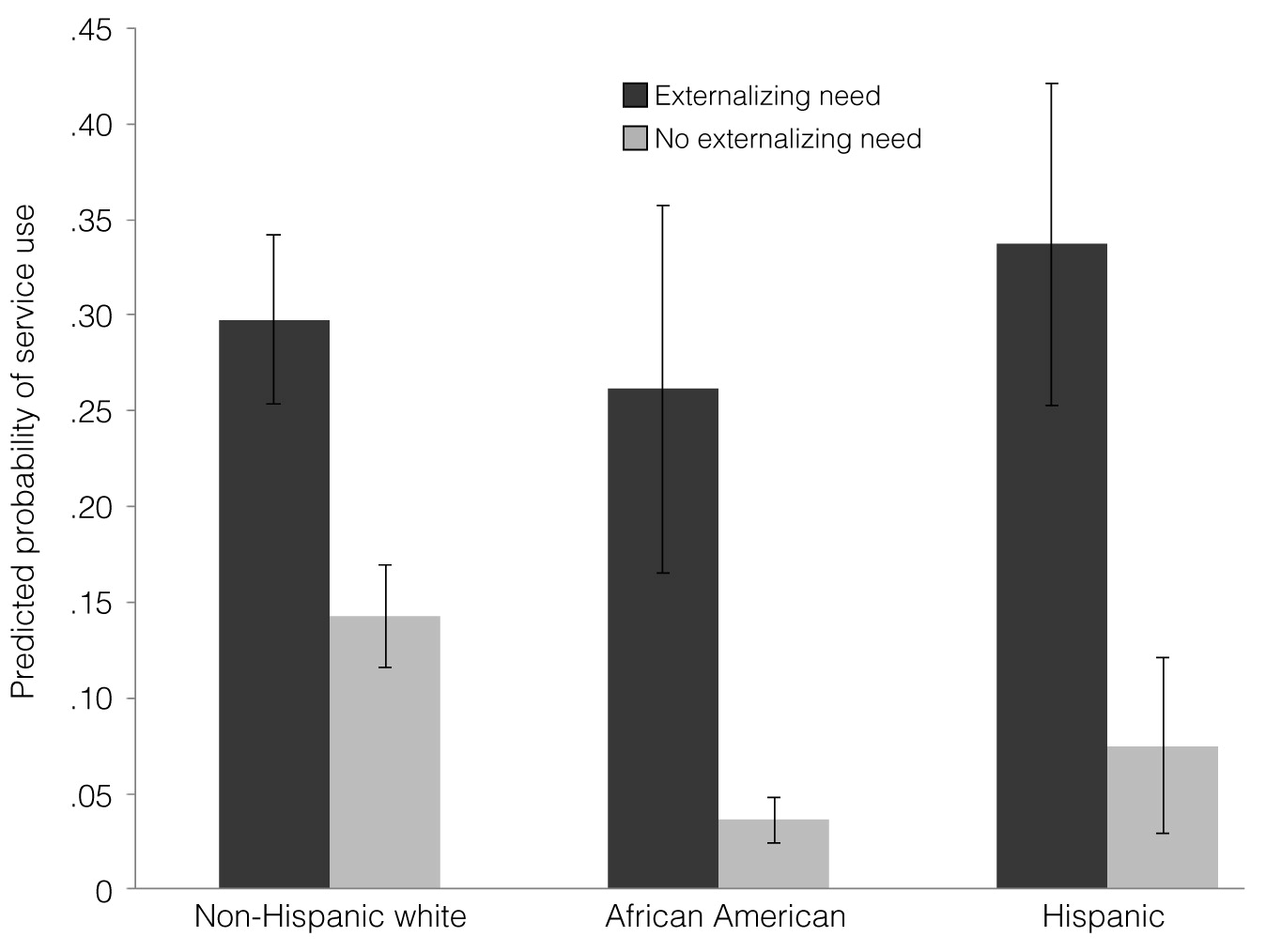
Figure 2 presents the predicted probability of service use as a function of youths’ race-ethnicity and the presence versus absence of externalizing need. African-American youths with externalizing need had a much greater probability of receiving services (26%) compared with African-American youths without externalizing need (4%). This discrepancy in predicted service use was smaller for non-Hispanic white youths with and without externalizing mental health need (30% versus 14%, respectively). Like African-American youths, Hispanic youths were more likely to receive services when they had externalizing need compared with when they did not (34% versus 7%, respectively), but this pattern did not differ significantly from that of non-Hispanic white youths.
Discussion
We examined racial-ethnic disparities in mental health service use by problem type in a national probability sample of children in contact with the child welfare system. Notably, we found no racial-ethnic differences in rates of internalizing or externalizing need. Consistent with previous cross-sectional research using these data (
5), African-American youths were less likely than non-Hispanic white youths to have received services by one year after contact with the child welfare system. However, when examining racial-ethnic disparities by problem type, we found that African-American youths were actually quite likely to receive mental health services in response to externalizing need. Although contrary to the typical finding of higher rates of unmet need among persons from racial-ethnic minority groups, this research is consistent with recent work aimed at examining problem-specific disparities (
4,
27). Conversely, race-ethnicity did not moderate the association between internalizing need and service use, but non-Hispanic white youths were the only group in which the presence of internalizing need was associated with a greater likelihood of service use relative to when internalizing need was absent.
Problem-specific disparities in service use likely result from multiple factors. First, practical barriers for racial-ethnic minority families may set a high threshold for accessing mental health services (
8–
10). Although contact with the child welfare system increases access to publicly funded health insurance, thus mitigating one important barrier, additional barriers remain (including access to mental health services in the community). Second, externalizing problems are more distressing to adults, may be easier for others to detect, and are considered more problematic than internalizing problems (
3,
21,
22). Cultural factors may also affect service use patterns in important ways. For example, previous research suggests that compared with non-Hispanic white parents, parents from other racial-ethnic backgrounds are less likely to identify child mental health problems (
28) or may hold different explanatory models about children’s problems (
10) or beliefs about how to address such problems (
29,
30). Furthermore, culture may also affect parental perceptions of the severity of their child’s problems, thus influencing caregiver thresholds for distress (
31). Within ethnic minority families, externalizing problems may be in high contrast to cultural values emphasizing respect, familism, and obedience, whereas internalizing behaviors may be more consonant with such values (
4,
27).
System-level factors in child welfare also likely affect problem-specific disparities. There is a robust finding that children from racial-ethnic minority groups are disproportionately represented in the child welfare system, despite no evidence of differential need for protection (
12,
32,
33). It remains unclear whether institutional bias in child welfare leads to increased scrutiny of disruptive behavior among children belonging to racial-ethnic minority groups. Similar to research in school systems (
14–
16), it is possible that in health services, adult gatekeepers of services (case managers, social workers, and foster parents, for example) may scrutinize the behavior of youths in minority groups more closely and may perceive more externalizing problems. Such factors may explain why African-American youths are more likely than non-Hispanic white youths to be diagnosed as having a disruptive behavior problem, even when parent-rated externalizing problems and clinician-rated impairment do not suggest racial-ethnic differences (
20). It should also be noted that disruptive behavior problems are of critical importance to child welfare, given that they are robust predictors of youths’ placement instability (
13). Heightened visibility and distress associated with externalizing problems may thus facilitate recognition of externalizing problems by adult gatekeepers of mental health services. Untreated internalizing problems, however, can also have lasting negative consequences (
34–
37).
The Institute of Medicine (
38) has noted that a disparity exists when there are differences in the treatment provided to individuals of different races or ethnicities when that discrepancy is not warranted by variation in the health conditions or treatment preferences of the group. A presumed injustice is thus central to the definition of a disparity. In this study, we found that after accounting for socioeconomic status and need, African-American youths continued to have a lower likelihood of receiving services compared with non-Hispanic whites. This finding would certainly fall within the Institute of Medicine’s definition of a disparity. However, our central focus on disparities by problem type also highlights a different form of disparity. African-American children in our study saw a sevenfold increase in the probability of receiving mental health services when they had an externalizing need. In essence, the child welfare service system appears to be quite responsive to the disruptive behavior of African-American youths—even more so than for non-Hispanic white children. Furthermore, the probability of receiving services was about 30% for all youths with externalizing problems, regardless of race or ethnicity. We did not find evidence of disparities by problem type for internalizing need. A sense of injustice may linger nonetheless when we consider that African-American youths are very likely to receive services (more than white youth) in response to “bad” behavior. The goal must be to ensure that need is a strong predictor of service use regardless of race or ethnicity and type of mental health need.
Our results should be viewed in the context of study limitations. For example, although we operationalized need based on caregiver- and youth-reported symptoms, the reason for seeking services was not known. Although disparities identified in our research are of high public health importance, additional research is needed to elucidate the specific processes that produced them. Understanding the factors that influence gatekeeper perceptions of need based on child race-ethnicity and problem type may be particularly illuminating. Furthermore, we defined service use as any contact with an outpatient mental health provider and thus are unable to address the quality and effectiveness of services received. Future research should examine whether quality of care differs by problem type. Finally, although constraining our analysis to children who remain with the same caregiver for the study period allowed us to examine the potential influence of caregiver-rated problems on subsequent service use, these results may not be generalizable to youths experiencing more frequent changes in placement.
Conclusions
This study examined problem-specific disparities in mental health service use prospectively in a nationally representative sample of youths in contact with the child welfare system and provides an assessment of the ability to identify and meet the needs of vulnerable youths. Results suggest that examining overall racial-ethnic disparities in unmet need obscured problem-specific disparities. Although identifying disparities is an important initial step, additional research is needed to elucidate factors that drive disparities. Because children in contact with the child welfare system are at high risk of emotional and behavioral problems and because a primary mission of the system is to ensure the well-being of children, it is imperative that we continue improving our ability to meet the needs of these youths. Routine evidence-based screening coupled with promotion of mental health education for biological parents, foster parents, and child welfare staff may prove to be useful interventions for reducing disparities in service use. By developing effective practices for reducing disparities, we may be better able to identify and meet in a more equitable manner the safety and mental health needs of all vulnerable children who come into contact with the child welfare system.
Acknowledgments and disclosures
The NSCAW was developed under contract from the Administration on Children, Youth, and Families, U.S. Department of Health and Human Services. This study was supported by Ruth L. Kirschstein National Research Service Award 5T32MH067763.
The authors report no competing interests.