The Veterans Health Administration (VHA) has delivered over 500,000 telemental health services in the past decade, with over 112,000 telemental health encounters in 2010 (
1). Historically, telepsychiatry consisted of medication management services, but it has since expanded to include individual and group psychotherapies. The large VHA administrative databases provide an opportunity to analyze the types of telemental health services being delivered, along with temporal trends in the expansion of telemental health.
The VHA has provided for extensive advances in knowledge about telemental health services, and there is now substantial evidence from randomized controlled studies supporting their use. This evidence includes the provision of diagnostic assessments (
2), medication management (
3), and individual (
4) and group psychotherapy services (
5). In addition, VHA administrative data were used in the first large-scale descriptive analysis of telemental health outcomes to show that access to telemental health services decreased inpatient hospitalizations (
6).
The VHA provides care to 3.3 million rural veterans, representing 41% of all VHA enrollees, and has created infrastructure and policies supporting the provision of telemental health services to this population (
7). Rural veterans are served by community-based outpatient clinics (CBOCs), which are connected to parent U.S. Department of Veterans Affairs (VA) medical centers by videoconferencing technology. In addition, VA policy mandates that specific mental health services are available at CBOCs. In 2004, VHA implemented the Mental Health Strategic Plan (
8), which identified increased access by veterans to evidence-based mental health treatments as a national priority. As VHA expands the use of videoconferencing to provide mental health services to rural areas, it is important to monitor the trends in the composition of telemental health services.
This study examined VHA administrative data to determine the types of telemental health services provided at the VHA over a five-year period, from October 1, 2005, to September 30, 2010. Specifically, the study sought to examine the composition of telemental health services delivered by the VHA health care system and to determine if the composition of telemental health services has changed over time.
Methods
We examined national-level VHA administrative data about telemental health services for fiscal years 2006–2010 (October 1, 2005–September 30, 2010). Typically the services were delivered to satellite CBOCs from a VHA health care facility by clinical videoconferencing equipment at bandwidth of 394 kbps. We did not examine home-based telehealth services. We obtained institutional review board approval from the Central Arkansas Veterans Healthcare System. Telemental health encounters were identified by a VHA mental health clinic stop code (500–599) and a VA telehealth secondary clinic stop code (690, 692, and 693). Duplicate workload credit for encounters at both the patient and the clinician site was eliminated.
Each telemental health encounter was categorized into one of five mutually exclusive services by Current Procedural Terminology (CPS) codes for medication management (90862), individual psychotherapy with medication management (90805, 90807, 90809, 90811, 90813, and 90815), individual psychotherapy without medication management (90804, 90806, 90808, 90810, 90812, 90814, 90845, 90875, 90876, and 96152), group psychotherapy (90849, 90853, 90857, and 96153), and diagnostic assessment (90801, 90802, and 90820). Individual psychotherapy with medication management was provided by a clinician with prescriptive authority, such as a psychiatrist or an advance practice registered nurse. Individual psychotherapy without medication management was provided by a nonprescribing clinician, such as a psychologist or a licensed clinical social worker. Group psychotherapy and diagnostic assessments were provided by clinicians with and without prescribing privileges. The total number of annual encounters for each service and the percentage change in the number of encounters for each service between fiscal years 2006–2010 were calculated.
Results
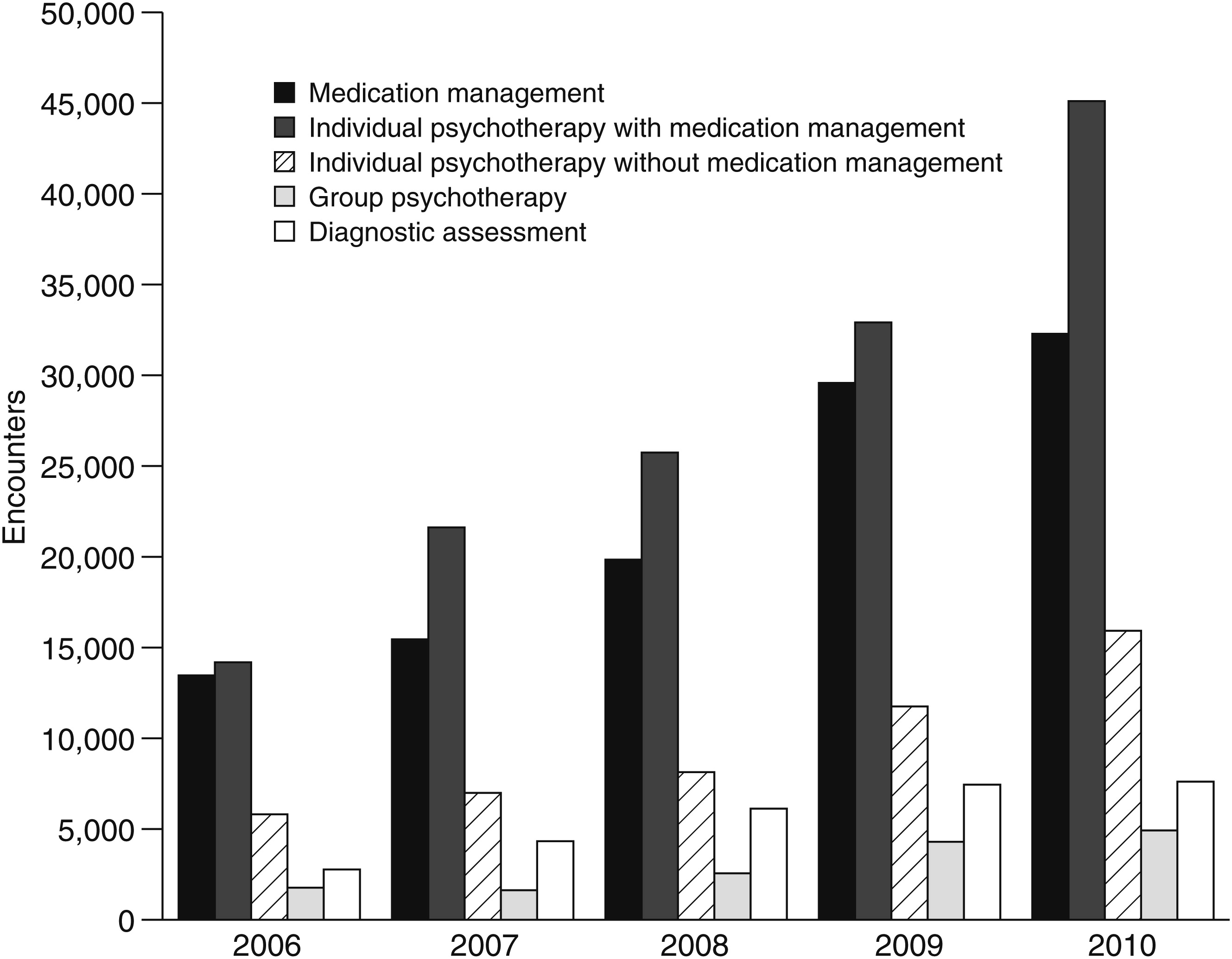
All types of telemental health encounters increased across the five years (
Figure 1). Individual psychotherapy with medication management was the most frequent telemental health service, followed by medication management alone. The third most frequent type of service was individual psychotherapy without medication management. The least frequently provided telemental health services were diagnostic assessments followed by group psychotherapy. [A figure showing the number of telemental health services in each category for each year is available online as a
data supplement to this report.]
As illustrated in
Figure 1, the proportional composition of telemental health services remained fairly consistent from year to year, with the exception of encounters for individual psychotherapy with medication management, which grew at a faster rate than the other services. Individual psychotherapy with medication management (N=139,569) grew by 218% over the five-year period while encounters for medication management (N=110,626) grew by 140%, individual psychotherapy without medication management (N=48,627) by 174%, group psychotherapy (N=15,184) by 178%, and diagnostic assessment (N=28,282) by 175%.
Discussion
Although the use of telemental health services originally focused on medication management, this national analysis demonstrates the expansion of telepsychotherapy, with or without medication management. The largest area of growth continued to be encounters with prescribing providers, suggesting that there is room for the growth of nonprescribing providers to provide manualized, evidence-based telepsychotherapy. The results of our trend analyses revealed that the composition of telemental health services has expanded to include large numbers of psychotherapy encounters, both with prescribing and nonprescribing clinicians. This finding demonstrates that telepsychotherapy has become more widely accepted and practiced and, perhaps, indicates that this trend will continue. In addition, this study, which reported nearly 5,000 group telepsychotherapy encounters in 2010, is the first to show that delivery of group telepsychotherapy on a large scale is feasible.
One limitation of the study is that the data were contingent upon correct coding by the clinician. Additionally, CPT codes that could have been used for telemental health, such as codes for brief new office visit (9000) and new limited office visit (90010), were excluded from the analyses because of our inability to classify them meaningfully. It is also important to note that the study did not include in-home telehealth services.
Conclusions
This study is the first to describe the types of telemental health services provided by VHA. The increase in number of telemental health encounters is encouraging given the growth of CBOCs and the number of recently returning veterans who reside in rural areas and face geographic barriers to mental health care (
9). A majority of telemental health services were for medication management and medication management with psychotherapy services, but there was a trend toward increased use of both individual and group psychotherapy services, which will be important to monitor. Future research should continue to refine our understanding of telemental health services by exploring the types of patients served (demographic and diagnostic characteristics) by telemental health providers and the location of these services (rural versus urban) and by comparing the results of this study with the use of face-to-face mental health services provided by VHA.
Acknowledgments and disclosures
The authors thank James Williams, B.S., program specialist at Central Arkansas Veterans Healthcare System, for valuable assistance in attaining and analyzing the data for this report.
The authors report no competing interests.