Childhood mental health problems are prevalent, debilitating disorders, but only half of the children with such disorders receive services (
1,
2). Those who do receive treatment frequently receive inadequate services (
3). Often children come for an evaluation, but do not start treatment, prematurely terminate services, may not adhere to treatment recommendations, or, given the slow diffusion of evidence-based practices into typical community-based services, may not receive an efficacious treatment (
4–
8).
Given that children rarely make their own treatment decisions, examinations of barriers to mental health treatment usually focus on parental and family factors. Although many theoretical models to describe use of mental health treatment have been proposed, a model by Olin and colleagues (
9) for explaining parental engagement has been particularly useful. Using the unified theory of behavior (
10,
11), they proposed that parent engagement is focused on four primary constructs, including beliefs and expectations, social norms, attitudes, and self-efficacy. Other research has identified barriers to treatment, including structural barriers, such as availability of services, transportation, and insurance, and perceptual barriers, including stigma, denial of need for treatment, and questions about the effectiveness of services (
12–
20). For families who terminate treatment early, important factors appear to be concerns about the cultural relevance of services, the families' comfort engaging with services, and the lack of consideration of family preferences when selecting services (
5–
8).
Family treatment preference is especially important for use of medications, given that many parents, particularly African-American parents, prefer psychotherapy over medication (
21–
24). Kazdin and colleagues (
25), as well as others, have established that parental ratings of the relevance of treatment are related to premature termination (
5,
21,
26). Further, parental beliefs in the likely effectiveness of therapy appear to have a curvilinear relationship to treatment attendance (
25).
Attention to parents' perceptions of the benefit of current services has been largely absent from the investigation of barriers, even though the model by Olin and colleagues (
9) suggests that parents' involvement in child mental health treatment depends on their perception of benefit. Data suggest that the risk of antidepressants as perceived by parents predicts fewer future child medication visits (
21). Similarly, parental expectations are related to perceived barriers to treatment, treatment attendance, and premature termination (
24). Data suggest that among adults, patients who strongly preferred counseling but did not receive it were likely to forego treatment completely (
23) and that attendance at self-help groups by families of individuals with mental illness was related to perceived benefits (
27).
Given the potential importance of parents' perception of benefits early in the treatment process for utilization of child mental health services, we examined family and child characteristics related to perceived benefits of outpatient mental health services for children. In addition, we examined whether perception of benefit after an initial treatment visit predicted continued use of outpatient mental health services during six-month follow-up. Specifically, we tested the hypothesis that parental rating of significant benefit measured early in the care process would be related to use of mental health services at six-month follow-up.
Methods
Parents or guardians of children age six to 12 years who were new patients of outpatient clinics participating in the Longitudinal Assessment of Manic Symptoms (LAMS) study and who spoke English were asked to complete a ten-item questionnaire to screen for elevated symptoms of mania. The Parent General Behavior Inventory Ten-Item Mania Scale (PGBI-10M) assesses hypomanic, manic, and biphasic symptomatology and discriminates bipolar disorder and other diagnoses among youths (
28,
29). Participation was limited to parents or guardians who spoke English and who did not have a child living in the same household who had been previously screened. Possible PGBI-10M scores range from 0 to 30, with higher scores indicating more manic symptoms. Children with scores of 12 or higher were invited to participate in the longitudinal portion of the LAMS study. In addition, a smaller group of patients with scores of 11 or lower who were roughly matched in real time on age, sex, race, ethnicity, and Medicaid status was selected to enroll in the longitudinal portion of the study. More details concerning participant ascertainment and the rationale for using a cutoff score of 12 on the PGBI–10M are described elsewhere (
30,
31).
Of the 1,124 children with elevated symptoms of mania, 621 (55%) accepted the invitation to participate in the longitudinal portion of the LAMS study. There were no statistically significant sociodemographic differences (age, sex, race-ethnicity, or insurance type) between children who did and did not enroll in the longitudinal study. A total of 86 parents or guardians of children without elevated symptoms of mania agreed to participate. A child whose family was approached but refused to participate was replaced by another demographically matched youth with a score of 11 or less on the PGBI–10M. Thus 86 children without symptoms of mania were also included in the longitudinal cohort (
30).
Baseline assessments were completed after the initial visit to the clinic, and participants who continued to be eligible were seen every six months. After six months, 678 children (96%) remained eligible, and the 573 (85%) children whose baseline benefit and treatment data were available were included in these analyses.
Children in the LAMS study received treatment as usual, starting with their first visit, at one of the nine clinics associated with four university-affiliated LAMS sites (Case Western Reserve University, in Cleveland; Cincinnati Children's Medical Center; the Ohio State University, in Columbus; and the University of Pittsburgh Medical Center-Western Psychiatric Institute and Clinic). Institutional review boards at each site reviewed and approved all procedures in the protocol. Written informed consent by parents or guardians and assent by participants were obtained before any procedures related to the study were performed.
Baseline assessment
Baseline data were collected during an interview conducted by specially trained research assistants within, on average, 36 days of the initial visit.
Demographic data.
Parents or guardians provided information on the child's age, sex, race, ethnicity, parental education, health insurance status, and medical history and on whether the child was living with both biological parents.
Diagnoses.
Children and their parents or guardians were administered the Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Episode (K-SADS-PL) (
32) with additional depression and manic symptom items derived from the Washington University in St. Louis Kiddie Schedule for Affective Disorders (WASH-U K-SADS) (
33,
34). Items to assess nonverbal communication, the child's relationship with others, shared enjoyment, and social-emotional reciprocity acording to
DSM-IV criteria were added to the K-SADS-PL to screen for pervasive developmental disorders. The resulting instrument, the K-SADS-PL-W, is a semistructured interview that assesses current and lifetime psychiatric diagnoses and the time course of each illness.
Unmodified
DSM-IV diagnostic criteria were used in the LAMS study. The criteria for bipolar disorder, not otherwise specified, were clarified for the LAMS study to follow the same criteria used in the Course and Outcome of Bipolar Youth (COBY) study (
35). All diagnoses were reviewed and confirmed by a licensed child psychiatrist or psychologist.
Medication history.
During the interview, the child's parent or guardian provided a complete history of the psychotropic medications prescribed to the child currently or in the past.
Functional assessment.
Study interviewers completed the Children's Global Assessment Scale (CGAS) to rate the severity of the participants' current impairment (
36). Possible CGAS scores range from 1 to 100, with higher scores indicating better functioning. Unfiltered manic and behavioral dysregulation was assessed by parent report on the PGBI-10M and the Young Mania Rating Scale (YMRS) (
37). Possible scores on the YMRS range from 0 to 60, with higher scores indicating more manic symptoms. Filtered manic symptoms were rated with the K-SADS Mania Rating Scale (
38). Unfiltered depressive symptoms were measured by the Children's Depression Rating Scale-Revised (CDRS-R) (
39). Possible CDRS-R scores range from 17 to 113, with higher scores indicating more depression. Filtered depressive symptoms were rated by the K-SADS Depression Rating Scale.
Family factors.
Parents' self-reports of mental health diagnoses as well as reports of diagnoses of first- and second-degree relatives were collected by using the Modified Family History Screen (
40). Parents were asked whether they or any of the child's siblings had received treatment or had been hospitalized for an emotional or behavioral problem. Parental stress was assessed by the Parent Stress Survey, and parental burden was assessed with 13 items from the Parent Stress Survey (
41). Possible scores for parent burden range from 0 to 52 and possible scores for parent stress range from 0 to 100, with higher scores indicating more burden or stress.
Use of mental health services.
The Services Assessment of Children and Adolescents (SACA) was completed at baseline and at each follow-up by parents or guardians. The SACA documents use of mental health services in inpatient, outpatient, and school settings and provides detailed data with excellent reliability and validity (
42–
44). Parents were asked to describe the child's most recent outpatient treatment (medication, therapy, medication and therapy, or evaluation) and to rate how well it had matched the child's needs by choosing one of three responses—not well, somewhat well, or very well. They were also asked to rate how much the child had benefited from treatment by choosing one of three responses—not at all, some, or a lot. This last question served as an outcome for these analyses. Because responses of some or not at all showed similar patterns of relationships with mental health services use, the responses were dichotomized (a lot versus some or not at all). The SACA was used at the six-month follow-up visit to establish whether children continued to use services.
Statistical analyses
SAS, version 9.2, was used to analyze the data; alpha was set at .05, and two-tailed tests were used for all analyses. Child and family characteristics were described by using counts and proportions for categorical variables; medians (25th and 75th percentiles) for skewed variables; and means and standard deviations for normally distributed continuous measures. Bivariate associations of child and family characteristics with each outcome of interest were examined by using univariable logistic regression analyses. Post hoc, pairwise comparisons were examined if the overall p value was statistically significant; given the descriptive nature of the bivariate analyses, no adjustments were made for multiple comparisons.
Multivariable logistic regression examined associations of child and family characteristics with each outcome, with site included as a design variable. The first model of parent perception of benefit included site and the three clinical measures of interest: primary diagnosis, treatment, and baseline child functioning. Model 2 included those measures plus child and family characteristics that were found by the bivariate analysis to be significantly related to parent perception of benefit and number of days between screening (initial clinic visit) and baseline assessment. The relation of parent perception of benefit of the child's most recent treatment with continuation of treatment for six months was examined by using a similar method. Model 1 included parent perception of benefit and site, and model 2 added child and family characteristics that were significantly related in the bivariate analysis to continuation of treatment. Results of the logistic regression analyses are summarized by using adjusted odds ratios (aORs) and 95% confidence intervals (CIs) (
45).
Results
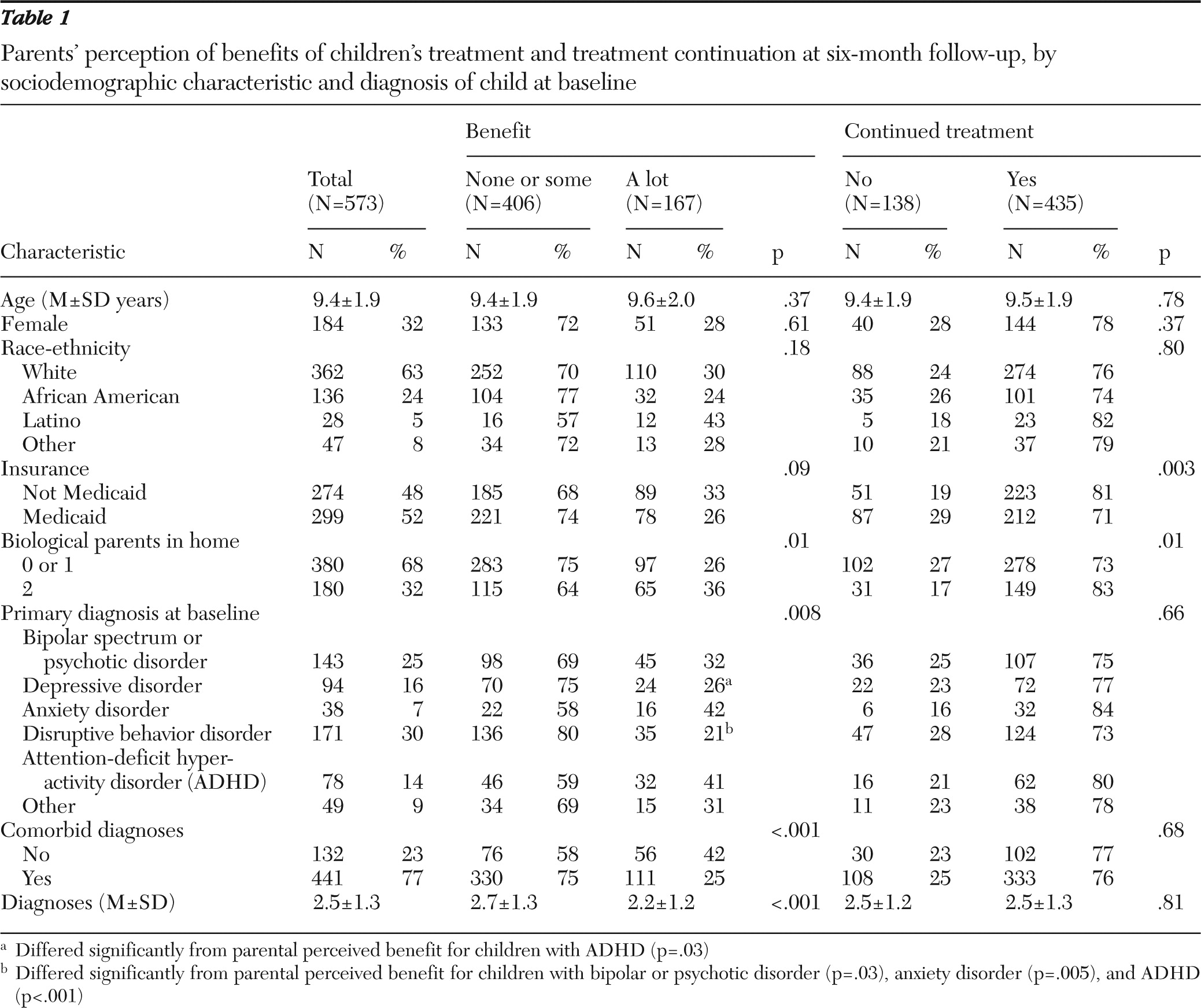
Perceived benefit
Tables 1–
3 show baseline characteristics of the entire sample (N=573) stratified by perceived benefit of treatment at baseline and continuation of treatment at six-month follow-up. Parents of 167 children (29%) reported that the child benefited a lot from treatment; 299 (52%) parents reported some benefit, and 107 (19%) reported no benefit. As shown in
Table 1, parents of children living with both biological parents were more likely than parents of children who lived with one or neither biological parent to report a lot of benefit from the most recent outpatient mental health treatment (36% versus 26%, p=.01).
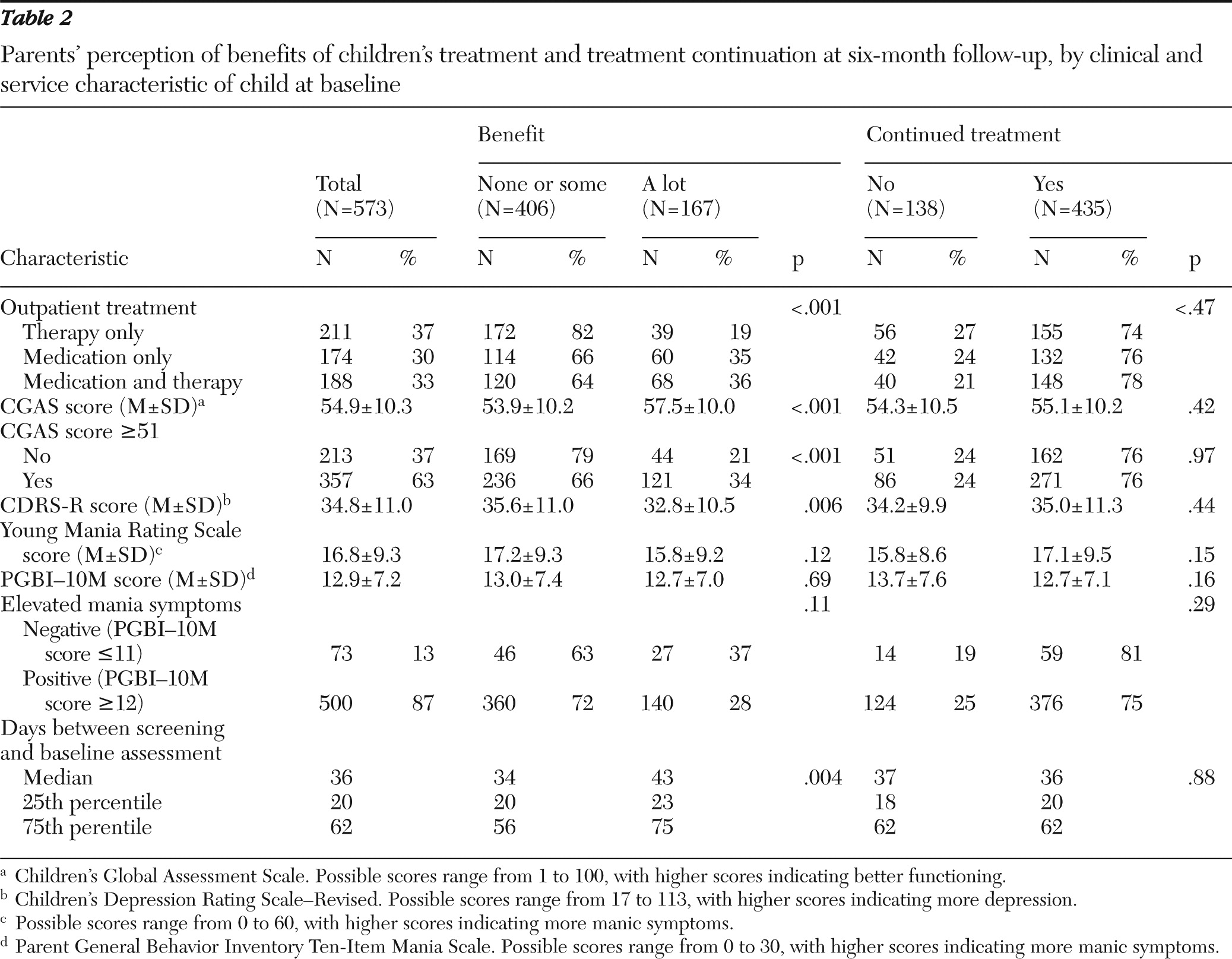
Children's clinical characteristics were consistently related to parent-reported treatment benefit. Parents of children with a primary diagnosis of bipolar or psychotic disorders, anxiety disorder, or uncomplicated attention-deficit hyperactivity disorder (ADHD) were more likely than parents of children with disruptive behavior disorders to report considerable benefit. Children with a depressive disorder were less likely than children with ADHD to receive treatment rated as very beneficial (26% versus 41%, p=.03). Parents of children without comorbid diagnoses and fewer diagnoses were more likely to rate the most recent treatment as beneficial. Parent ratings indicated that children who received only psychosocial therapy were half as likely as children who received medication with or without therapy to have benefited a lot from their most recent treatment (19% versus 36% and 35%, respectively, p<.001) (
Table 2).
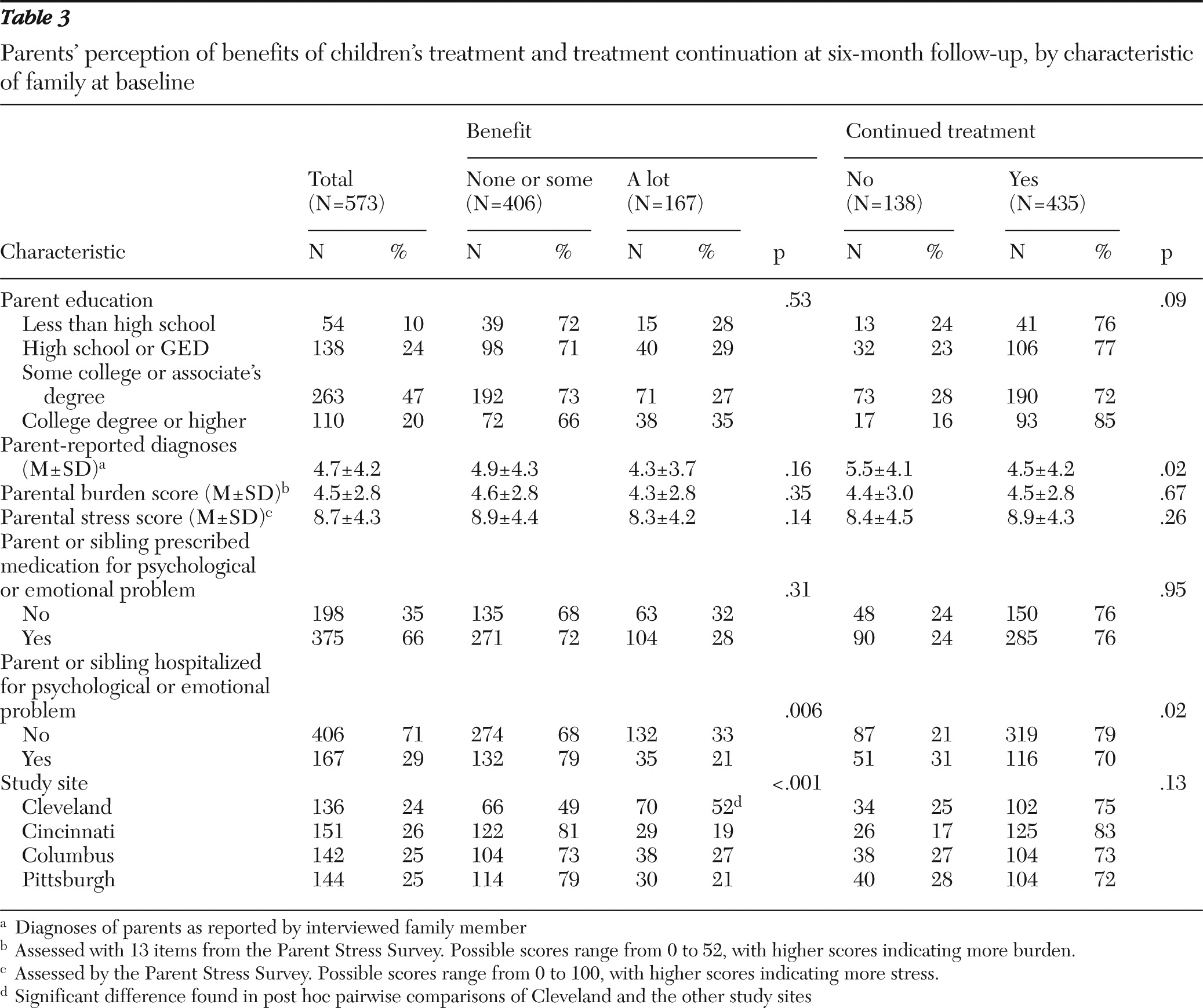
Parents were more likely to rate treatment as beneficial if their child had higher CGAS scores or lower CDRS-R scores (
Table 2) and no immediate family member who had been hospitalized for a mental health problem (
Table 3). Parents in Cleveland were twice as likely as parents in Cincinnati, Columbus, and Pittsburgh to rate mental health services as beneficial (52% versus 19%, 27%, and 21%, respectively, p<.001) (
Table 3). There were no statistically significant differences in ratings of benefit among the three other sites. Finally, the proxy measure of length of treatment, days between screening and the baseline interview, was positively associated with benefit.
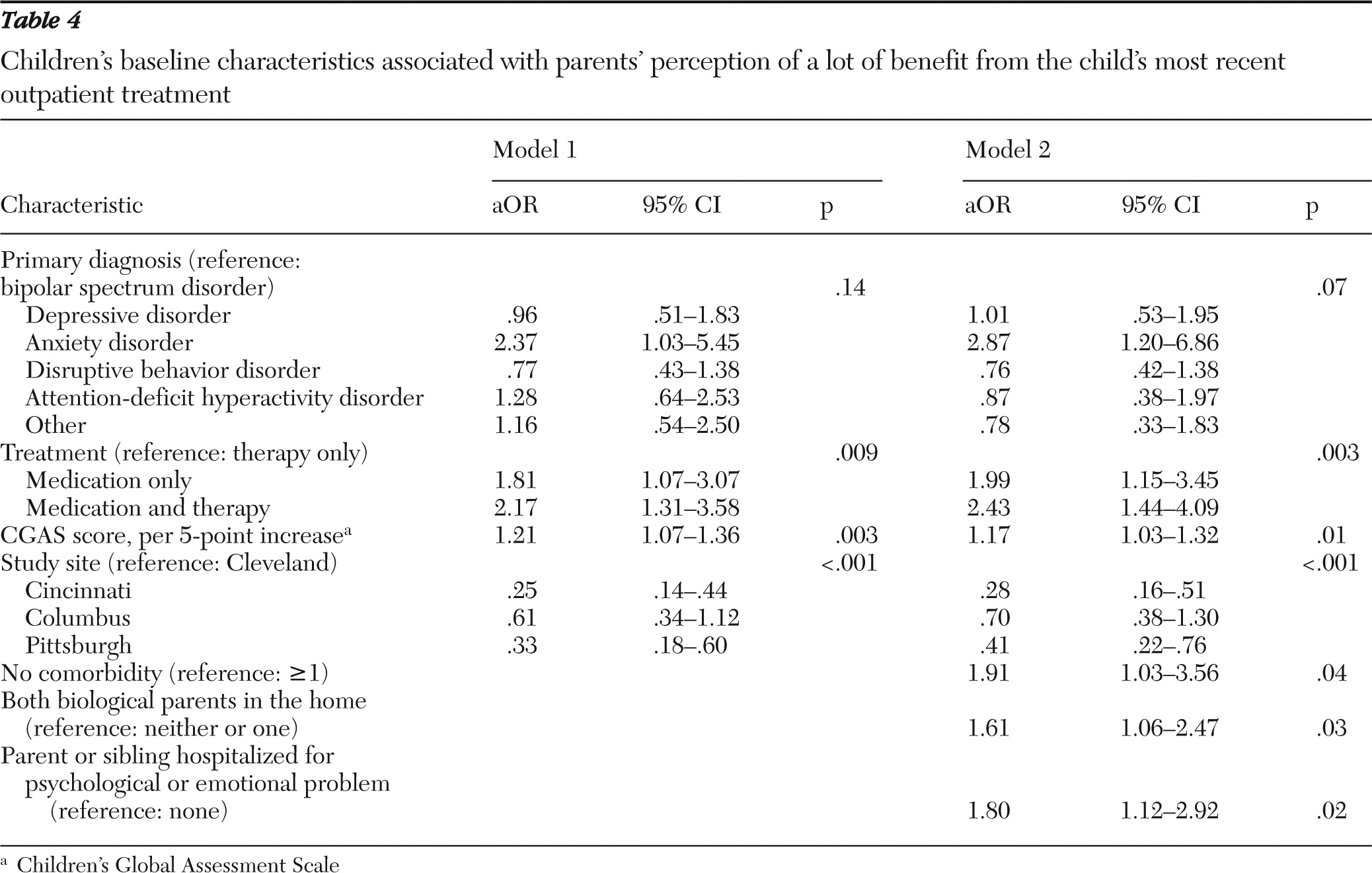
Model 1 of the multivariable modeling showed that diagnosis was no longer significantly related to the perception by parents that their children received a lot of benefit from treatment (
Table 4). However, baseline treatment, baseline CGAS score, and site of treatment were related to perceived benefit of most recent treatment. Compared with parents whose children received therapy alone, parents of children receiving medication only had 1.81-fold increased odds of reporting considerable benefit, and parents of children receiving medication and therapy had more than twofold increased odds of reporting considerable benefit (aOR=2.17, p<.009). Similarly, CGAS score, a measure of functioning, remained related to perceived benefit. Each 5-point increase in CGAS score was associated with 21% increased odds of perceived benefit (p=.003).
Model 2 also indicated that parents of children with no comorbid diagnoses had almost twice the odds of perceiving treatment as beneficial (aOR=1.91, p=.04). Other factors in the model that remained associated with perceived benefit included treatment site, living with both biological parents, and not having an immediate family member who had ever been hospitalized for a mental health problem.
Continued use of services
We examined characteristics associated with remaining in services at the six-month follow-up (
Tables 1–
3). Three-quarters of the children (N=435, 76%) continued to receive outpatient mental health services at the six-month follow-up. Demographic characteristics, including race-ethnicity, were not associated with continuation of treatment. Children who lived with both biological parents were more likely than children who lived with one or neither biological parent to continue outpatient treatment (83% versus 73%, p=.01). The proportion of children who continued outpatient treatment for six months was smaller among children with Medicaid insurance than among children without Medicaid insurance (71% versus 81%, p=.003). Children's clinical characteristics at baseline were not significantly related to continuation of treatment, but clinical characteristics of the family, including fewer parent mental health problems (4.5 versus 5.5, p=.02) and not having a parent or a sibling who had been hospitalized for a mental health problem (79% versus 70%, p=.02), had positive associations with continuation of treatment.
A majority (83%) of parents who perceived a lot of benefit from their child's most recent outpatient mental health treatment reported that their child continued with treatment for six months. Continuation of treatment was reported by 78% of parents who perceived some benefit and by 60% of parents who perceived no benefit (data not shown).
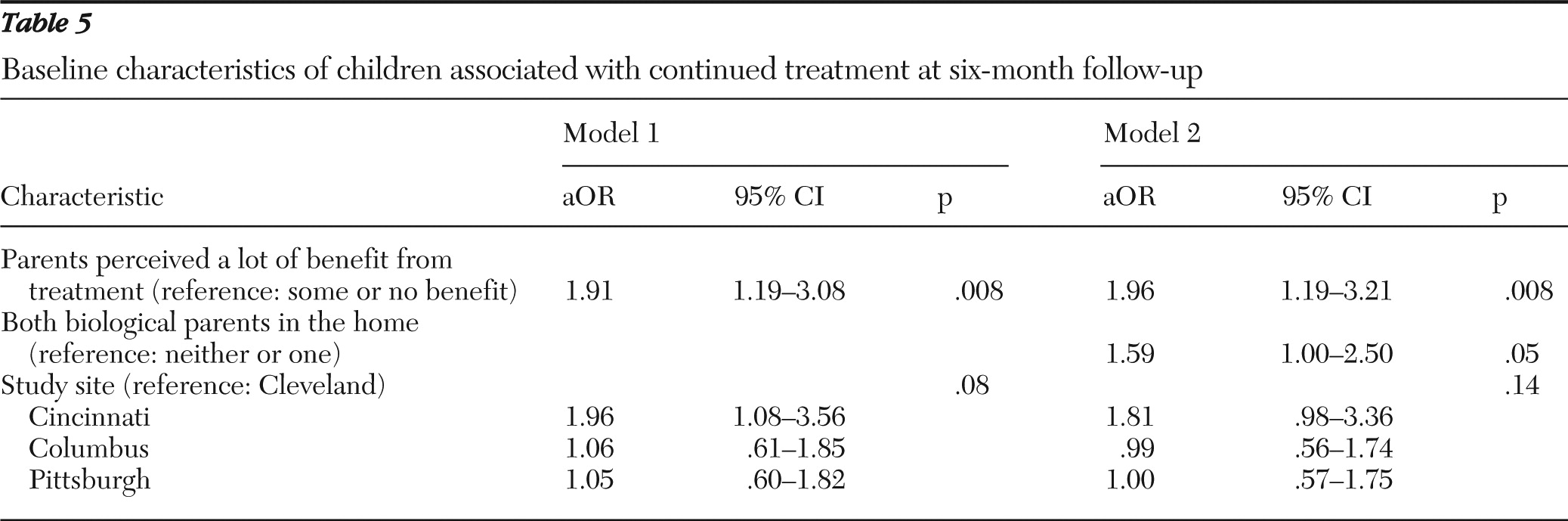
The multivariable model predicting continued use of treatment showed that after adjustment for study site, perceived benefit of treatment was significantly related to continued treatment at six-month follow-up (
Table 5). The odds of continuing treatment for six months were increased 1.91-fold among children whose parents perceived a lot of benefit from treatment compared with children whose parents perceived some or no benefit (p=.008). Living with both biological parents was the only other baseline characteristic that was significantly associated with continuation of treatment for six months (aOR=1.59, p=.05) (model 2).
Discussion
These analyses suggested that perceived benefit early in treatment may be an important predictor of remaining in treatment and that multiple factors were correlated with parents' perceptions of the benefit of treatment. As previously suggested in the literature (
24), parents perceived treatment to be beneficial among children with higher functioning and fewer symptoms at baseline. Surprisingly, among the sociodemographic variables associated previously with perceived efficacy of treatment (
21,
24), only living with both biological parents was related to perceived benefit in this study population. Perhaps most striking was the association of benefit and receiving medication or medication and therapy versus receiving therapy alone, a finding similar to results reported for treatment of ADHD (
46). Given the reported preference of parents, particularly parents belonging to a racial or ethnic minority group, for counseling over medication (
18,
24), the endorsement of benefit of medication may indicate that parents suspend their concerns about potential side effects when they believe medications have led to improvements for their children.
Interestingly, race and ethnicity were not related to perceived benefit from treatment or continuation of treatment at six-month follow-up. In fact, African-American and white children continued in treatment at similar rates (74% and 76%, respectively) as Latino children and children of other or mixed race (82% and 79%, respectively). That suggests that early termination of treatment by nonwhite children and families, which has been often reported, may be service-setting specific.
The relationship of perceived benefit to remaining in treatment is consistent with, although not the same as, the finding by Nock and Kazdin (
24) that parent expectancies are related to premature termination. Thus, as suggested by Olin and others (
9), discussing with parents their perceptions of the benefits that their children are receiving from treatment early in the treatment process may be a useful strategy to prevent premature termination (
47). Parental engagement in their children's mental health treatment has been shown to increase utilization, and seeking parents' input about treatment benefit may be an important part of such engagement (
9,
48).
As with all data, these data have certain limitations. The sample was a cohort of outpatient utilizers that was enriched for symptoms of mania and that was located in one geographical region. These children may not have been representative of all users of child outpatient mental health services. Not all members of the study population had baseline treatment and benefit data, although we identified no child, family or clinical differences between those with and without those data. These treatment-utilization data were self-reported, and no data were verified. Benefit from treatment consisted of one question, and we collected no data from clinic records on the quality of care children received. The absence of data on the care received is important because of the differences in perceived benefit of treatment in Cleveland compared with treatment at the other sites. Because these children were recruited from outpatient mental health clinics, these data also provided no information on factors important for initially seeking services.
Conclusions
The relationship of perceived benefit of treatment to its continued use is an important finding that could be used to develop strategies to engage families in treatment. Given the paucity of interventions that improve engagement and retention, exploration of perceived benefit as a factor in continuation of treatment is warranted (
49). Future studies should also consider the child's perception of benefit (
50,
51) as well as the interaction of parental and child perceptions of benefit. Given that efficacious mental health treatments are available, initiating and maintaining treatment among children are critically important to ensure that children receive the care that could improve their health.
Acknowledgments and disclosures
This study was supported by grants R01-MH073967, R01-MH073801, R01-MH073953, and R01-MH073816 from the National Institute of Mental Health (NIMH). The authors thank NIMH for the support but acknowledge that the findings and conclusions in this manuscript are theirs and do not necessarily reflect the opinions of NIMH.
Dr. Frazier has received research support from, acted as a consultant to, received travel support from, or received a speaker's honorarium from Integragen, Shire Development, Inc., and Bristol-Myers Squibb. Dr. Fristad receives royalties from Guilford Press, American Psychiatric Press, and Child and Family Psychological Services, Inc. Dr. Arnold receives research funding or advisory board honoraria from Curemark, Eli Lilly and Company, Shire, AstraZeneca, Biomarin, Novartis, Noven, and Seaside Therapeutics. Dr. Youngstrom receives travel support from Bristol-Myers Squibb and serves as a consultant to Lundbeck. Dr. Birmaher receives royalties from Random House and Williams & Wilkins. Dr. Findling receives or has received research support, acted as a consultant, received royalties from, or served on a speaker's bureau for Abbott, Addrenex, Alexza, American Psychiatric Press, AstraZeneca, Biovail, Bristol-Myers Squibb, Dainippon Sumitomo Pharma, Forest, GlaxoSmithKline, Guilford Press, Johns Hopkins University Press, Johnson & Johnson, KemPharm Lilly, Lundbeck, Merck, Neuropharm, Novartis, Noven, Organon, Otsuka, Pfizer, Physicians' Post-Graduate Press, Rhodes Pharmaceuticals, Roche, Sage, Sanofi-Aventis, Schering-Plough, Seaside Therapeutics, Sepracore, Shionogi, Shire, Solvay, Sunovion, Supernus Pharmaceuticals, Transcept Pharmaceuticals, Validus, WebMD, and Wyeth. The other authors report no competing interests.