In early 2009, Australia experienced its most extensive natural disaster. Bushfires devastated large parts of Victoria, which resulted in the loss of 173 lives, affected 51 townships, and destroyed over 2,000 homes in addition to many businesses, schools, and kindergartens (
1). As part of the Australian government's mental health response to the 2009 Victorian bushfires, support to people most affected by the fires was delivered through enhanced primary mental health care services.
The existing evidence demonstrates that disasters of this magnitude can significantly affect the mental health of individuals and communities in multiple ways and at varying levels of severity and duration. Mental health sequelae after previous international disasters have been widely documented (
2,
3), including after Hurricane Katrina, which devastated Mississippi in 2005, and after the September 11, 2001, terrorist attacks on the World Trade Center and the Pentagon. Furthermore, the prevalence of sequelae such as posttraumatic stress disorder (PTSD), other anxiety disorders, and suicidality has been reported to persist at 17 to 19 months postdisaster (
4). Despite this lingering need, only a minority of disaster survivors with mental disorders access adequate mental health care. Structural, financial, and attitudinal barriers contribute to this problem (
5), and little is known about what treatments work in this context (
3).
Primary mental health care
In July 2001, the Australian government funded the Better Outcomes in Mental Health Care (BOiMHC) program in response to low treatment rates for common mental disorders. A key feature of the BOiMHC program is its Access to Allied Psychological Services (ATAPS) component. ATAPS enables family physicians (known in Australia as general practitioners) to refer patients with highly prevalent disorders (depression and anxiety) to allied health professionals (predominantly psychologists) for free or low-cost, evidence-based mental health care (most commonly cognitive-behavioral therapy [CBT]). This care is typically delivered in six individualized sessions, with an additional six sessions (or 12 sessions in exceptional circumstances) made available in a calendar year if this is considered warranted after a review by the referring general practitioner. In addition, up to 12 group sessions are also available (
6).
ATAPS is operationalized via a series of projects run by regional general practice networks, which are primary health care organizations involved in health promotion, early intervention and prevention strategies, chronic disease management, and workforce support for general practitioners. Currently, all 111 Australian general practice networks are running ATAPS projects.
Enhanced primary mental health care
In February 2009, additional funding from the Australian government was provided to each of nine bushfire-affected Victorian state general practice networks (one via a fund-holding arrangement with a tenth organization) under the ATAPS projects. The funding aimed to increase provision of psychological services to bushfire-affected people, with additional training made available for ATAPS allied health professionals to enable them to provide appropriate and evidence-based support to this group of people.
ATAPS projects in bushfire-affected regions were enhanced to provide more flexible services. Bushfire-affected individuals with persistent psychological symptoms (as opposed to a disorder) were afforded certain flexibilities concerning their access to services. In addition to the usual general practitioner referral pathway, referrals could be made by the Victorian Department of Human Services bushfire case managers (provided that, in the case of the latter, a general practitioner referral involving an explicit assessment and treatment plan was prepared while the consumer was being treated via ATAPS), and there was no limit on the number of sessions of care provided. Additional funding continues to be provided to a number of general practice networks to ensure that they have capacity to support people affected by bushfires.
This study evaluated services delivered via ATAPS. To demonstrate the role of enhanced primary care in a disaster context, we report on the uptake of ATAPS, the consumer and session profiles, and the outcomes achieved. Qualitative data are presented to supplement this aim. To our knowledge, the role of primary mental health care has not been the focus of postdisaster mental health service utilization literature (
7).
Methods
The study received clearance from the University of Melbourne, Human Research Ethics Committee. Deidentified data were analyzed from a Web-based minimum data set used for routine program monitoring and required under organization funding agreements. Before participating in the interviews, key informants were asked to provide their written informed consent.
Data sources
Minimum data set.
Data were collected via providers and entered by project officers (or providers) into a Web-based purpose-designed national minimum data set that captured data on the numbers of general practitioners, allied health professionals, and consumers involved in the projects; sociodemographic (including age, gender, and level of income) and clinical (including diagnosis, previous psychiatric service use, and clinical outcome) characteristics of consumers; and the number, type, and duration of sessions and the nature of the interventions provided. In addition, a field for program type identified a given consumer as having been referred to the ATAPS bushfire service, and a separate data field identified the source of the referral (general practitioner or bushfire case manager). Uptake data were available for nine general practice networks.
Key informant interviews.
Semistructured interviews were conducted with ten project officers or program coordinators and one chief executive officer from ten general practice networks (including the fund holder) involved. Interview questions explored issues related to offering services for consumers affected by bushfires (such as impacts on general practice networks, facilitating factors, and potential improvements). Interviews were conducted in person or by telephone, then recorded and transcribed.
Data analyses
Minimum data set.
Descriptive analyses of the uptake of the ATAPS bushfire services and consumer and session profiles were conducted. Paired t tests were used to examine the difference between mean pre- and posttreatment scores on selected outcome measures. Consumers who did not have a matched pair of pre- and posttreatment scores were excluded. The analysis period was January 1, 2009, to June 30, 2011.
Interviews.
Transcripts of interviews with key informants were thematically analyzed. The analyses involved coding responses according to a prestructured thematic coding system that was developed in direct alignment with the interview questions. These broad response categories were then further analyzed for the existence of more detailed subthemes.
Results
Uptake of the ATAPS bushfire service
Overall, 1,891 referrals were made by 391 general practitioners and 65 case managers, and sessions were conducted by 194 allied health professionals. Overall, 9,949 sessions were delivered to 1,535 (or 81% of the referred) consumers, making 6.5 the average number of sessions per referral.
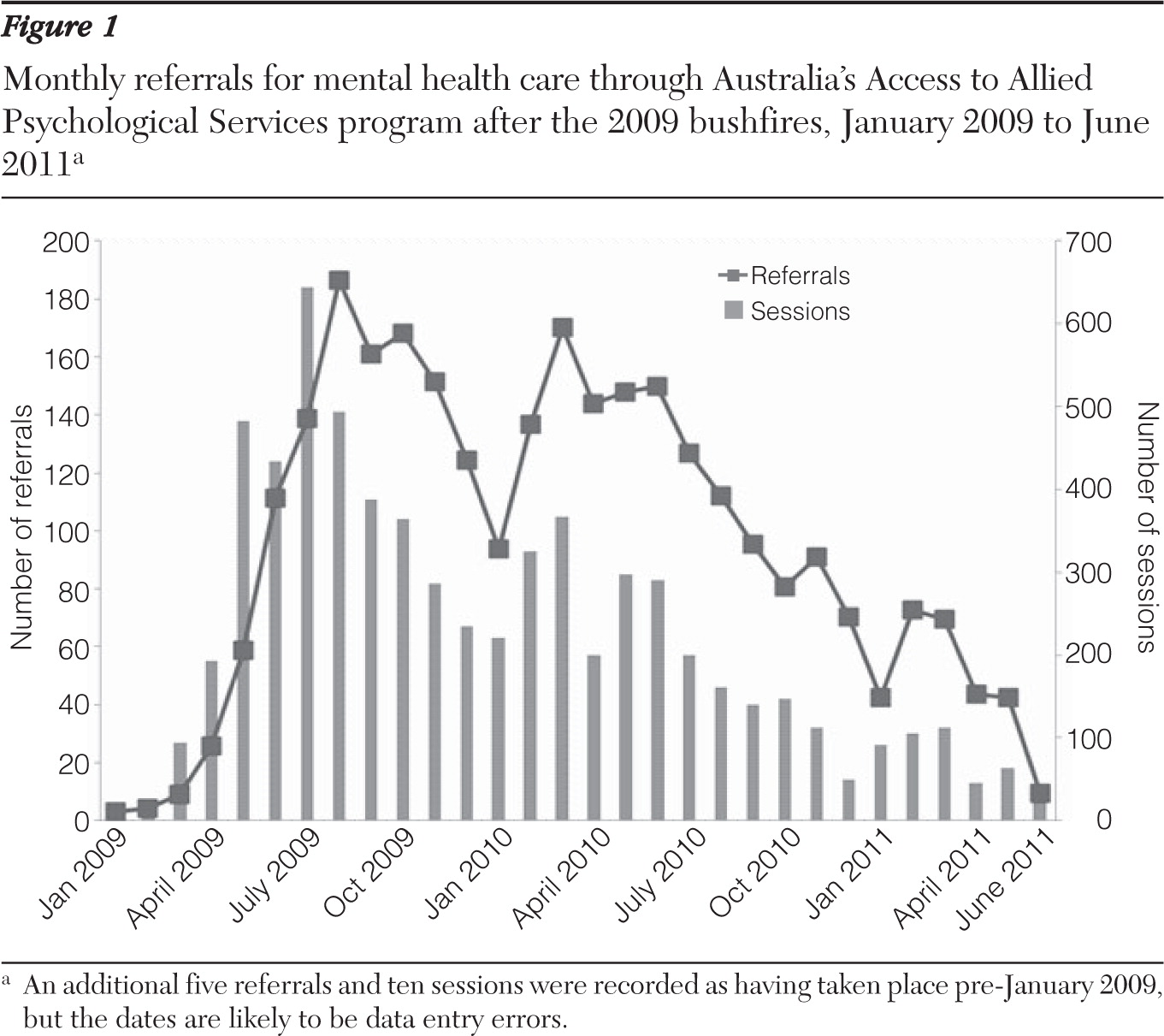
Figure 1 shows referrals and sessions by month for the nine general practice networks that supplied data from January 2009 to June 2011. The number of referrals and sessions gradually increased and peaked in July and August 2009, respectively. After declining, they peaked again in March 2010, around the time of the one-year anniversary of the bushfires. Since this second peak, referrals and sessions have been gradually decreasing and may be attributable to relocation of consumers or to a genuine reduction in need for the enhanced service. The decline in referrals and sessions in the last quarter may be attributable to data entry lags.
Sociodemographic and clinical profile of consumers
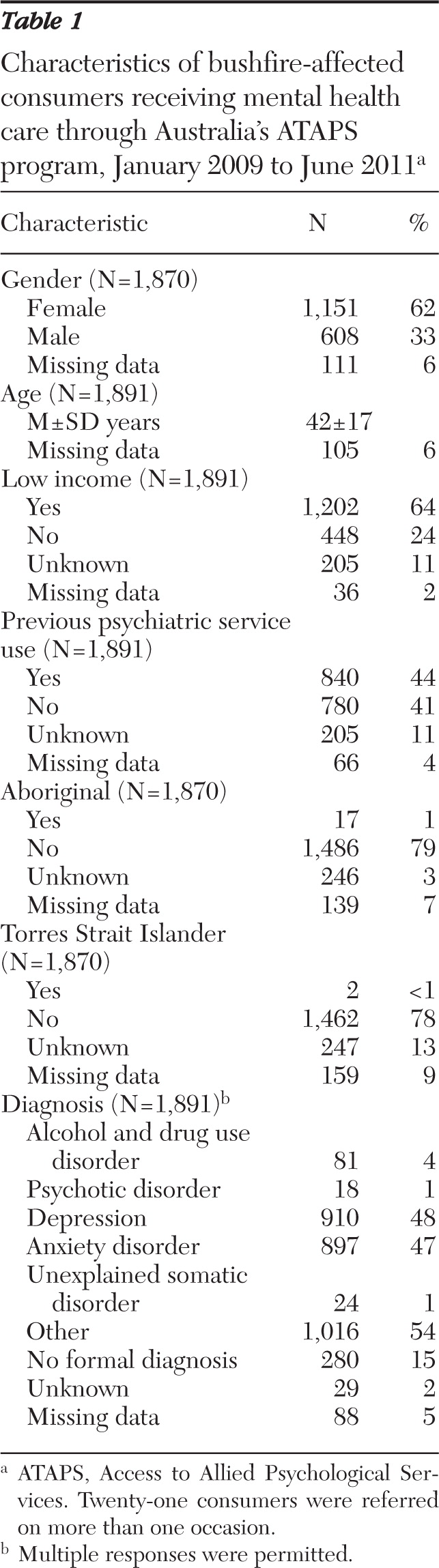
Table 1 summarizes some of the key characteristics of the consumers receiving care through the ATAPS bushfire services. Overall, 62% of consumers were female, and the mean age was 42 years. Almost two-thirds had low incomes, as judged by their general practitioners. Over two-fifths of consumers had not accessed mental health care before the bushfires. Approximately 1% of consumers were reported to be Aboriginal, and less than 1% Torres Strait Islander. Most consumers were diagnosed as having depression (48%), an anxiety disorder (47%), or a diagnosis classified as “other” (54%), and consumers may have had comorbid psychiatric diagnoses. Many of the free-text descriptors of other diagnoses were indicative of variants of stress, trauma, PTSD, and bereavement. A further 15% were reported not to have a formal diagnosis.
Characteristics of sessions
The profile of sessions delivered to bushfire-affected consumers is shown in
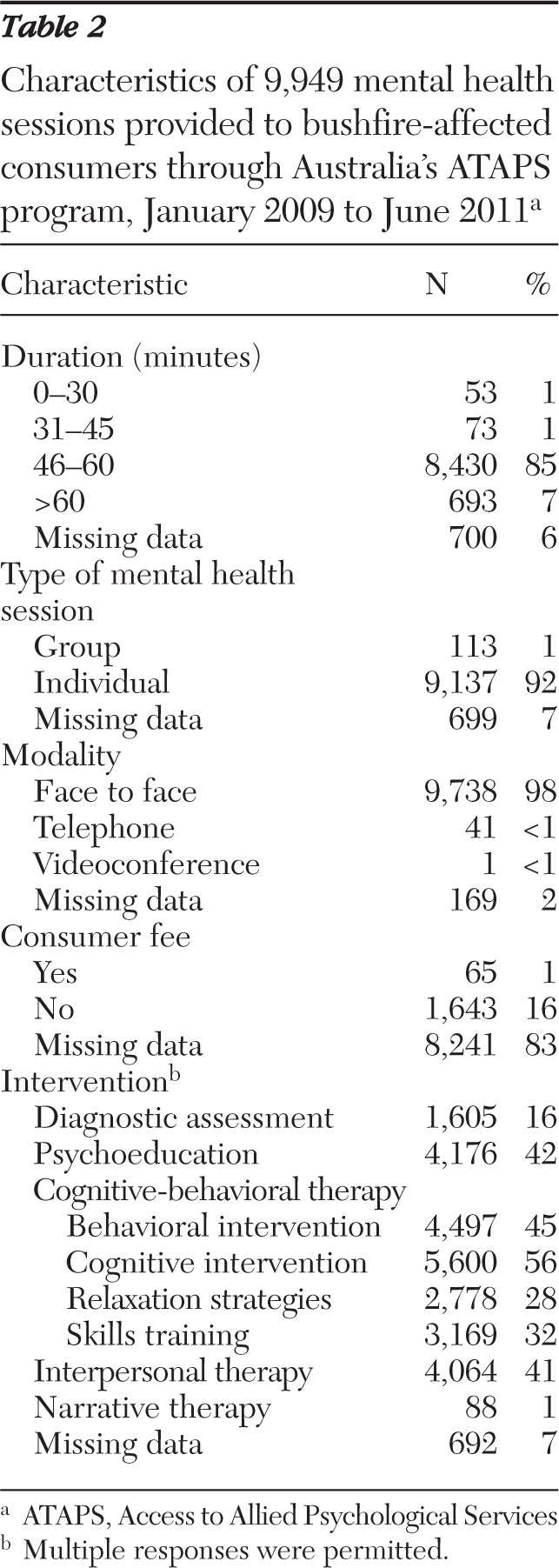
Table 2. Almost all sessions (92%) were delivered to individuals. Overall, sessions of 46–60 minutes accounted for the vast majority (85%) of services delivered. The most frequently delivered interventions were cognitive (56%) or behavioral (45%); however, psychoeducation, interpersonal therapy, CBT skills training, and CBT relaxation strategies were also commonly delivered. A small number of sessions were delivered via telephone, and one was delivered via videoconference. Of the 1,708 sessions where payment information was available, a majority (1,643 sessions, 96%) were delivered free of charge.
Consumer outcomes
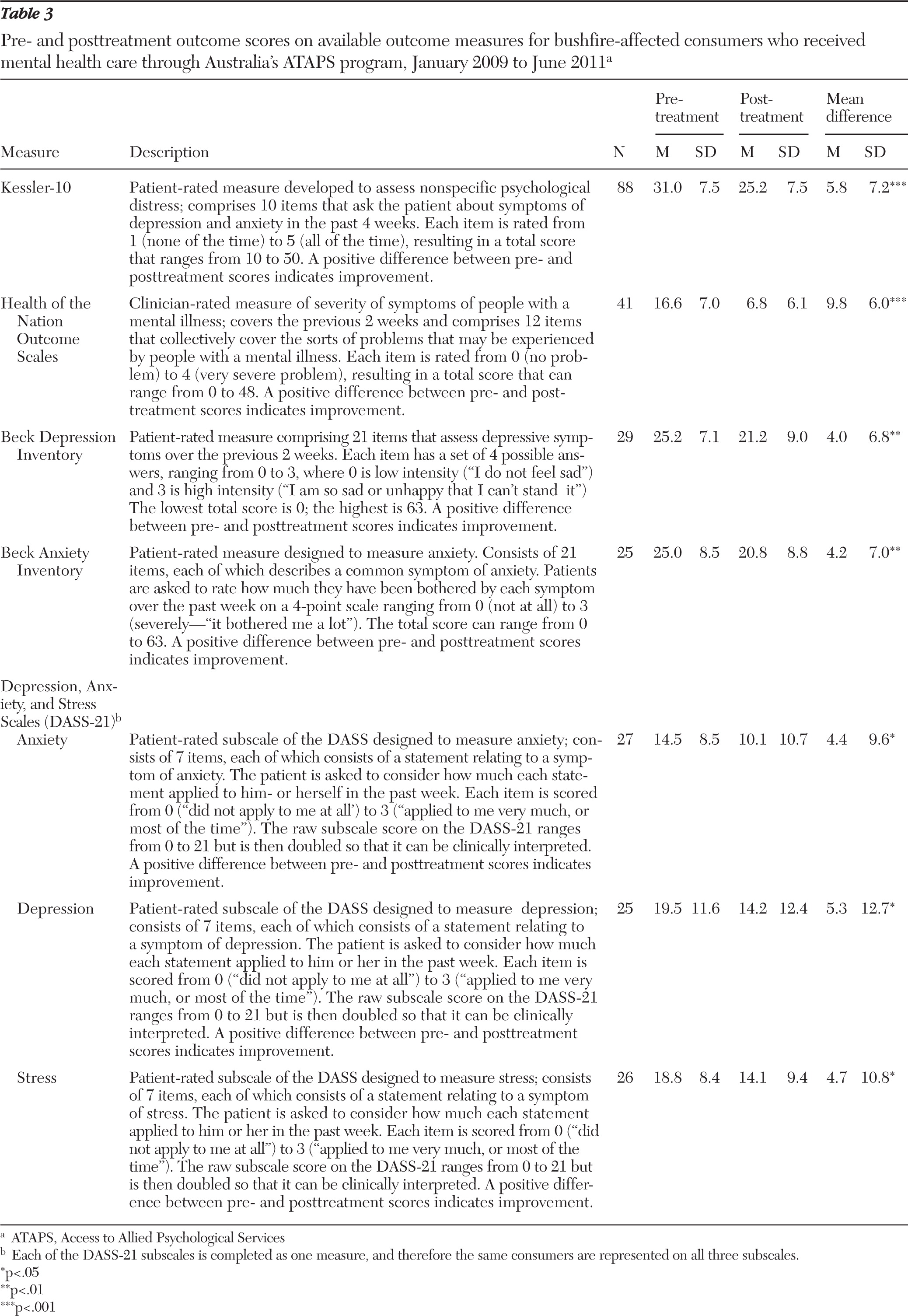
In total, 261 cases of matched pre- and posttreatment outcome measure scores were available, representing 12% (or 188 of 1,535) of consumers.
Table 3 shows the number of consumers (ranging from 25 to 88) assessed with each outcome measure and the mean difference in pre- and posttreatment scores on the five measures used: the Kessler-10 (
8), the Health of the Nation Outcome Scales (
9), the Beck Depression Inventory (
10), the Beck Anxiety Inventory (
11), and the Depression, Anxiety, and Stress Scales (DASS) (
12). With the exception of the DASS, the mean differences were based on total scores; in the case of the DASS, the mean differences were based on scores for each of the three subscales. Across all measures, the mean difference was statistically and clinically significant (with an average reduction in symptom severity from severe to moderate and from moderate to mild), indicating positive consumer outcomes.
Effects of the ATAPS enhanced services
Key informant interviews confirmed that ATAPS had produced positive outcomes for bushfire-affected consumers and highlighted other positive impacts, facilitating factors, and potential improvements.
Impact on general practice networks.
Overall, the ATAPS bushfire service was reported to have had positive impacts on participating general practice networks. Most notably, general practice networks reported an increase in their public profile among other agencies, schools, and the community. Complementary to this, general practice networks reported an increase in their awareness of regionally relevant issues, enabling them to support townships and services beyond their usual roles. They also developed or strengthened relationships with other organizations (including local, state, and federal government; emergency services; and community health). The benevolence associated with supporting general practitioners and consumers was also favorably viewed. In general, informants reported either no or few negative impacts of the ATAPS bushfire service. Examples of negative impacts included increased workload and uncompleted usual duties; workforce health issues associated with physical, emotional, and mental stress; inaccessibility of suitably qualified ATAPS professionals; and issues associated with temporary (or project-based) funding.
Facilitating factors.
Numerous factors facilitated the effective operation of the ATAPS bushfire service. Most notably, the flexibility of service guidelines optimized responsive and timely access to unlimited psychological services. The flexible guidelines contributed to an extremely favorable response to the service by general practitioners and allied health professionals. This was demonstrated by the high volume and immediacy of referrals made by the former, who often were already utilizing ATAPS, and the goodwill and expertise of the latter.
The opportunity to embed the specialist bushfire service within the ATAPS platform, particularly in locations with strong preexisting ATAPS models, facilitated utilization of the general practice networks' existing infrastructure, knowledge base, relationships, and local networks and therefore the capacity to immediately commence service delivery. Service delivery models used by each general practice network are flexible, thereby optimizing responsiveness to local needs (
13). In some instances, new allied health professionals were recruited to meet demand and expertise needs or to service a wider geographic area. Although most services were delivered in general practitioners' or allied health providers' offices, other locations (such as outreach to home) were used as necessary to ensure that those in need received services.
Good collaboration and support between general practice networks and other organizations, providers, and neighboring and other general practice networks were also important. The responsiveness of the Australian Government Department of Health and Ageing to the needs of general practice networks was imperative and was demonstrated by provision of an appropriate level of initial funding and extension of funding beyond the initial year in recognition that there was an ongoing need being met.
Improvements.
Despite its overall success, a number of potential improvements to the service were identified. A needs analysis of individual general practice networks was recommended to determine preparedness for response to future disasters. More opportunities for key stakeholders to provide government with feedback were desired. Creating a good overall communication strategy about the entire suite and coordination of available services, developing structural systemic relationships between services, and improving the engagement of general practice networks by the Victorian government were also recommended. Further flexibility of service guidelines was desired, particularly regarding the types of interventions permitted and eligible providers (such as grief and bereavement counselors).
The skill level of providers varied, indicating that the available provider training should have perhaps been mandatory as part of the specialist service provision model. More funding was desired for a range of activities other than direct service provision (including community recovery, marketing, increased administration, uncounted costs of workforce health problems, and monitoring people who had relocated). In order to identify existing, continuing, and unmet need and to facilitate planning for longer-term recovery, respondents recommended improving data collection and the availability of general practice network-level data.
Discussion
Overall, the ATAPS bushfire service was well utilized and received in most regions. From January 1, 2009, to June 30, 2011, bushfire referrals and sessions accounted for 18% and 22%, respectively, of all ATAPS referrals and sessions associated with the nine involved general practice networks.
The service uptake pattern, over a period in excess of two years postdisaster, resembled that of the crisis counseling programs (CCP) offered after Hurricane Katrina (
14) and September 11 (
15), with peaks for all three observed at around six to nine months and again about one year later. The exception to the latter was the September 11 CCP, and this is probably attributable to a change to a cost-based reimbursement at 12 months (
15). These uptake patterns indicate that postdisaster counseling should be made available for extended periods (
15), with shifting emphasis to meet the changing needs of high-risk groups (
16). Although CCP and ATAPS differ in that CCP was a community outreach program delivered by trained paraprofessionals, these paraprofessionals also identified and referred 7% (or 46,500) of individuals for more intensive psychological intervention (likely to resemble that delivered via ATAPS) (
17).
Furthermore, the brevity of services associated with the CCP approach is considered to be inconsistent with post-Katrina epidemiological research demonstrating high rates of disorders and clinically significant distress, suggesting a need for more intensive services (
14). Efforts have been made to deliver unlimited enhanced services or specialized crisis counseling services that involve a team-based approach, a master's-level counselor (trained in solution-focused therapy and CBT), and a resource coordinator, and these efforts to improve responsiveness have produced promising results (
18,
19). However, the enhanced primary mental health care approach described in this article presents a viable alternative model. The model is appropriate on the grounds that of the 35% of Australians with mental health problems who seek help, a majority consult general practitioners (
20), and most Hurricane Katrina survivors relied on the general medical sector for mental health care (
5).
Although a diagnosis was not required for consumers to access the ATAPS bushfire service, most consumers had a diagnosable anxiety disorder or depressive disorder or both. Although this was not an epidemiological study, this finding confirms previous reports that depressive and anxiety disorders are the most common mental disorders in the aftermath of disasters (
2,
21).
The findings were comparable to routine ATAPS in terms of the characteristics of consumers and sessions (
22) and the positive outcomes produced (
22,
23). However, bushfire-affected consumers were somewhat more likely to be males and to have an anxiety disorder and somewhat less likely to be indigenous and to have a depressive disorder. Bushfire ATAPS sessions were more likely to deliver psychoeducation, relaxation strategies, skills training, and interpersonal therapy but less likely to incur a fee payable by the consumer. Together, the interventions delivered and the positive outcomes produced by the bushfire ATAPS service provide support for the merit of CBT interventions, which have had successful trials among September 11 (
24) and Hurricane Katrina survivors (
3).
Some caution must be exercised in interpreting the findings because the evaluation had several limitations. Bushfire ATAPS uptake data were derived from our purpose-designed minimum data set. They are likely to be underestimated because bushfire referrals are unlikely to have been consistently identified in the minimum data set. This caveat was confirmed by the interview data, which revealed that some general practitioners were referring as needed to “routine” ATAPS without distinction. Nonetheless, the data available suggest that a substantial number of consumers received services.
Because the study specifically focused on one segment of specialist mental health services rather than the overall psychosocial response to the bushfires, conclusions about the overall need for mental health services and whether that need was met cannot be directly inferred. Adding to the preclusion of such conclusions was that treatment retention was not assessed and data to enable assessment of the sample's representativeness of the bushfire-affected population or the population more broadly were not available. Uniformity of data collection systems across the entire health sector and the ability to link these data as well as epidemiological studies of disaster-affected regions at various points both pre- and postdisaster may shed light on issues of demand and capacity (
25).
Within the scope of our evaluation, we could not include a comparison group, nor would it have been ethical or logistical to do so in a postdisaster context. Lack of a comparison group limits the certainty that treatment was responsible for the improvements in consumer outcomes, although improvements in the absence of treatment are unlikely to match the magnitude of improvements shown here. The proportion (12%) of patients for whom pre- and posttreatment outcome data were available was not optimal but is not uncommon for studies of this kind (
26). In addition, the appropriateness of the outcome measures used in a disaster context is unknown.
Conclusions
Despite these limitations, this evaluation advances the field in a number of important ways. It is novel in its focus on primary mental health care in a postdisaster context, and findings may be applicable in other disaster contexts internationally. Further, our evaluation corroborates previous findings regarding the most common mental disorders and the efficacy of evidence-based treatment postdisaster.
Notwithstanding the overall achievements of the ATAPS bushfire service, some challenges were experienced in terms of preexisting workforce issues and the desire for further flexibility of service guidelines. The evaluation provided valuable insights about processes that may be improved to optimize the ATAPS bushfire service, including communication, coordination, and structural systemic relationships between services.
Pivotal to the success of the enhanced ATAPS bushfire service were multiple interrelated factors. These included the opportunity to mobilize and enhance the existing infrastructure of the innovative ATAPS model in a disaster context, genuine desire by primary mental health care organizations and other stakeholders to help those in need, responsive modifications to service delivery guidelines, responsiveness of providers and of the Australian Government Department of Health and Ageing to the needs of general practice networks, and overall good collaboration among stakeholders.
The 2009 Victorian bushfires, among Australia's worst natural disasters devastating large parts of the community, put enormous pressure on existing service and support systems. Enhancement of the overall capacity of the primary mental health care system in response to the disaster enabled people with clinically diagnosable disorders and considerable psychological distress to access free or low-cost treatment. Most important, this treatment produced positive outcomes for consumers in terms of recovery by reducing symptoms and improving psychosocial functioning.
Acknowledgments and disclosures
This work was funded by the Australian Government Department of Health and Ageing.
The authors report no competing interests.