Co-occurring mental and substance use disorders are common among community and clinical populations, and it is estimated that half of individuals with mental disorders experience substance misuse in their lifetime (
1–
3). Prior research indicates that most individuals with co-occurring disorders do not seek specialty treatment but are often seen in general medical settings or by social services (
4,
5), pointing to a need to integrate systematic substance screening into primary care settings to identify individuals at risk and to facilitate treatment contacts. This approach is particularly relevant for low-income patients seeking mental health services in community health centers because of their limited access to specialty care.
To date, few studies besides research trials have examined substance screening and referrals for substance abuse treatment within the context of integrated mental health care. In this study, we examined rates of substance screening and treatment referral and correlates of treatment access in a large statewide integrated care program in Washington state (
6,
7).
Methods
Funded by Washington state and King County and operated by the Community Health Plan of Washington, the Mental Health Integration Program (MHIP) (
http://integratedcare-nw.org) provides mental health care in over 100 community health centers (
6,
7). MHIP is based on the collaborative care model (
8), in which mental health services are provided in primary care settings by an interdisciplinary team that includes the participant’s primary care provider, a clinic-based care manager, and a psychiatric consultant. Consultants regularly review cases with care managers and make treatment recommendations. Participants who do not improve or are psychiatrically complex receive higher levels of care (stepped care) (
8). Additionally, MHIP provides a Web-based patient registry to track participants’ clinical assessment, diagnoses assigned by their clinicians, treatment received, and outcome improvements.
Between 2008 and 2010, a total of 12,429 participants receiving welfare benefits as part of the state Disability Lifeline program were enrolled in MHIP. The MHIP program is limited to low-income, unemployed individuals who do not qualify for permanent disability benefits but have been disabled for at least 90 days because of a general medical or mental illness.
All participants (N=11,150, 90%) with a complete intake assessment were included in this study. The intake assessment includes a battery of clinical assessments such as the Global Appraisal of Individual Needs–Short Screener (GAIN-SS) for substance use problems. The GAIN-SS is a self-report screener that includes five items assessing weekly alcohol and drug use, problems caused by use, and use-induced withdrawal symptoms in the past year. This screener has been shown to reliably identify substance abuse and risk of hazardous use (
9).
Clinicians are instructed to assess participants with a positive score on screener about the nature and degree of their substance use and make a provisional diagnosis of substance abuse in the patient registry. Participants with a provisional diagnosis are considered screened positive and are given a referral for substance abuse treatment services. For analysis, a dichotomized variable was created to reflect those who reported accessing the recommended treatment services and those who declined such services.
Baseline demographic and clinical characteristics included age, gender, suicidal thoughts, treatment history, and diagnosis of depression, anxiety, posttraumatic stress disorder (PTSD), and bipolar disorder. Treatment process indicators included the number of follow-up contacts with the care manager in the first month of treatment and receipt of psychiatric case review. Care manager contacts in the first month of treatment were previously reported to be associated with participants’ clinical improvement (
6).
Rates of substance screening and treatment referrals were calculated. A mixed-effects logistic regression model was used to evaluate demographic and clinical correlates of treatment referral, taking into account the nesting of participants within health care organizations. All analyses were conducted on deidentified data collected for quality improvement purposes and were not considered research requiring individual patient consent by the institutional review board at the University of Washington. Only aggregate data are presented.
Results
Participants were predominantly male (N=6,301, 56%) with a mean age of 40.9±11.2 years (range 18–85 years). Baseline psychiatric diagnoses included depression (N=8,391, 75%), anxiety (N=6,306, 57%), PTSD (N=2,658, 24%), and bipolar disorder (N=1,990, 18%). Almost half of participants (N=5,379, 48%) endorsed thoughts of death or suicide. A total of 3,961 (36%) participants reported past treatment for mental disorders, and 2,712 (24%) reported past treatment for substance-related problems.
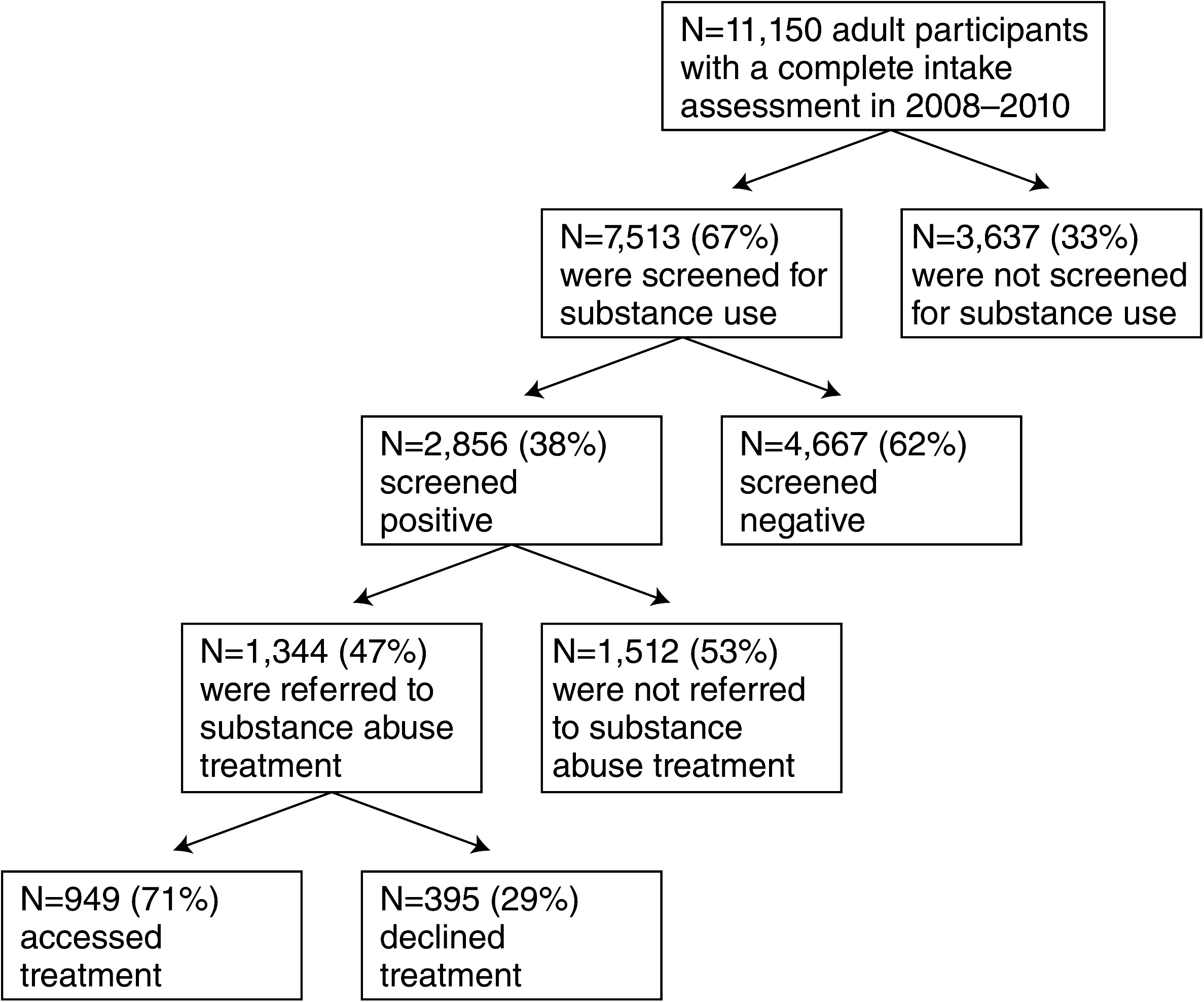
At intake, 7,513 (67%) participants were screened for substance abuse and 2,856 (38%) participants screened positive (
Figure 1). The screening rate across participating community health centers ranged from 16% to 98%. Alcohol was the most commonly misused substance (N=1,965, 69%), followed by cannabis (N=677, 24%), cocaine (N=358, 13%), methamphetamine (N=331, 12%), narcotics (N=274, 10%), and heroin (N=269, 10%). One-quarter of participants (N=1,843, 25%) reported using two substances, and 304 (11%) participants used three or more. Among participants with a positive screen, 1,344 (47%) were referred to substance abuse treatment services and of those, 949 (71%) reported using the recommended treatment services.
Several correlates were associated with increased access to recommended treatment services: history of substance abuse treatment (odds ratio [OR]=1.43, 95% confidence interval [CI]=1.09–1.89, p=.009), alcohol use (OR=1.55, CI=1.16–2.07, p=.003), heavy drug use (OR=1.54, CI=1.16–2.04, p=.003), PTSD (OR=1.42, CI=1.04–1.93, p=.026), and treatment follow-up contacts with a care manager (OR=1.61, CI=1.21–2.13, p=.001).
Discussion
One-third of low-income individuals receiving integrated mental health treatment in primary care were not screened for substance use. Among those who screened positive, approximately two-thirds were not referred to substance abuse treatment or did not access the recommended treatment services. Consistent with prior studies that have shown inadequate interventions and access to substance abuse treatment in various primary care settings (
10,
11), our evaluation also revealed missed opportunities in substance screening and referral to the needed services for this vulnerable population.
Opportunities for improving the care of participants with substance abuse treatment needs may include pay-for-performance incentives for systematic substance screening. In fact, a recent study found this approach to be effective in increasing quality of care and improving mental health outcomes (
7). Additionally, equipping program care managers and primary care providers with brief interventional skills, integrating mental health and substance abuse treatment services, and enhancing parity of health care benefits may help improve access to care for this population (
12–
14).
Participants with higher levels of psychiatric complexity and those who were followed up with greater intensity were more likely to use recommended substance abuse treatment. It is possible that increased treatment contacts with care managers mediate the pathway to successful treatment referral. The finding is compatible with the principles of stepped care, in which patients with higher levels of clinical need receive more intensive interventions. Future research to explore the possible mediation effects of treatment intensity on participants’ access to substance abuse treatment is recommended.
Several study limitations are noted. First, as with most observational studies, there are inherent limitations with regard to our ability to make causal inferences. Second, information about the actual dosage and modality of substance abuse treatments received and whether patients without a referral received treatment from other services was not available. Additionally, participants’ self-reports of access to recommended treatment may be biased toward socially desirable responses. Last, we were unable to measure the characteristics of the care managers and the clinics, which may influence the screening and referral process (
12,
14,
15).
Conclusions
Individuals with low income account for a disproportionate number of patients served in community health centers; however, their needs for substance abuse treatment services are often unmet. The significance of this issue warrants continued efforts in optimizing substance screening, office-based intervention, and referral process in the community health centers.
Acknowledgments and disclosures
The Community Health Plan of Washington (CHPW) and Public Health of Seattle and King County (PHSKC) provided funding for collection of the data used in these analyses during an ongoing quality improvement program. Dr. Chan and Dr. Unützer were supported through a contract from CHPW and PHSKC to provide training and technical assistance related to the program. Dr. Huang was supported by grant T32 MH20021-14 from the Health Services Division of the National Institute of Mental Health.
The authors report no competing interests.