Smoking is the leading cause of preventable mortality in the United States (
1). Smoking is a risk factor for lung cancer and heart disease and contributes to other health problems, such as diabetes and obesity (
2,
3). Previous studies have documented that many more people with serious mental illnesses smoke cigarettes compared with those in the overall population (
4,
5). Among those with serious mental illness, the prevalence of smoking has been found to be higher among persons with schizophrenia than among those with bipolar disorder or major depression (
5). Previous studies also indicate that persons with serious mental illness smoke more heavily, have longer smoking histories, and have lower rates of smoking cessation than smokers in the overall population (
6–
8). It is not surprising, then, that cigarette smoking contributes to the excess morbidity and mortality among people with schizophrenia and other serious mental illnesses (
9–
11).
Over the past decades there have been intense public health campaigns to reduce cigarette smoking in the overall population. Although 42.4% of adults in the United States were smokers in 1965, the prevalence had declined to 24.7% in 1997 and then to 19.3% in 2010, the most recent year for which data are available (
1,
12). Attention to cigarette smoking among persons with serious mental illness has lagged behind efforts in the overall population despite the high prevalence of smoking and the known health risks to persons with mental illness. This gap is due to a number of factors, including inattention by health care providers and also the relative isolation of persons with serious mental illness from appeals aimed at the mainstream population (
5,
13). Recently, however, greater efforts have been made to address smoking among persons with mental illness, and there are now more documented experiences of successful quitting in this group (
14,
15). However, it is not known to what extent smoking has declined in recent years among persons with serious mental illness in routine care (inpatient and outpatient) settings.
Previous studies also have examined the correlates of smoking and quantity of cigarettes consumed by persons with serious mental illness; these variables have been associated with male gender and older age—findings that mirror trends in the overall population (
5,
16,
17) and with Caucasian race in some studies (
17–
20). Previous investigations have also found that smoking by persons with serious mental illness is associated with co-occurring substance abuse (
5). Some studies have also found that smokers with serious mental illness have more severe psychiatric symptoms (
17,
18,
21–
24), poorer quality of life (
18), and more medical comorbidities (
18,
25) than nonsmokers and, in schizophrenia specifically, smokers are more likely to be receiving first-generation rather than second-generation antipsychotic medications (
17). However, much of the data for these studies were collected prior to 2005, before the most recent efforts to address smoking cessation in this population.
This study was undertaken to determine the prevalence of cigarette smoking and the quantity of cigarettes consumed by individuals with schizophrenia, bipolar disorder, or no disorder who were participating in a research program that recruited persons in the period 1999–2011 without regard to their smoking status.
Methods
Participants were individuals with schizophrenia, bipolar disorder, or no disorder who were enrolled in the period January 1999 to December 2011 in a Stanley Research Program study of the association between antibodies to infectious agents and serious mental illness. Recruitment of the schizophrenia group began in 1999, and recruitment of the bipolar disorder and no-disorder groups began in 2002. Details of the inclusion and exclusion criteria and recruitment procedures for the study populations have previously been described (
26–
28). The diagnosis of each of the participants in the psychiatric disorder groups was made by a board-certified psychiatrist on the basis of the Structured Clinical Interview for DSM-IV Axis I Disorders (
29). The participants without psychiatric illness were screened with the Structured Clinical Interview for DSM-IV Axis I Disorders Non-Patient Edition (
30). All participants provided written informed consent, and the studies were approved by the Sheppard Pratt Institutional Review Board.
As part of the background interview, each participant was asked “Are you a current cigarette smoker?” And, if the participant answered yes, the interviewer followed up with “How many packs per day do you smoke?” All participants were also asked about their education and other demographic variables, including maternal education as a proxy for family socioeconomic status (
31). All participants in the groups with schizophrenia or bipolar disorder were asked about the duration of their disorder and were evaluated on the Positive and Negative Syndrome Scale (PANSS) (
32). These participants were also categorized for history of substance abuse (apart from nicotine) on the basis of their medical record and their response to interview questions about the use of alcohol and drugs. Medications received at the time of study enrollment were based on the medical chart and self-report.
Demographic and clinical characteristics and smoking status were compared among study groups using analysis of variance for continuous variables and chi square analysis for dichotomous variables.
Logistic regression was used to examine temporal trends in both smoking prevalence and smoking quantity (among smokers only); likelihood ratio chi square tests determined whether these trends were statistically significant (p<.05). Polychotomous logistic regression was used to model quantity of cigarettes smoked; models evaluated whether the log odds of each consumption category (>.5–1.0 packs per day [ppd]; >1.0–1.5 ppd; and >1.5 ppd) decreased relative to the lowest category (≤.5 ppd). First, temporal trends in each smoking outcome were assessed separately for each diagnostic group; next, a model was fit that consisted of diagnostic group plus year plus their interaction. The demographic covariates age, race (Caucasian versus non-Caucasian), and gender were added to each model.
Logistic regression was also used to examine correlates of both smoking and cigarette consumption by participants with schizophrenia or bipolar disorder. As for the temporal trends analysis, polychotomous logistic regression was used to model the quantity of cigarettes smoked, and a categorical outcome variable was coded with the following categories: 0; >0–.5 ppd, >.5–1.0 ppd, and >1.0 ppd. The independent variables that were included in these models were all variables that had a significant bivariate association with the outcome variable: duration of illness, gender, race (Caucasian versus non-Caucasian), education, maternal education, substance abuse history, PANSS total symptom score, and diagnostic group (schizophrenia versus bipolar disorder). Age was not included in the model because the variable was highly correlated with duration of illness.
Within each diagnostic group, the association between smoking status and selected medications (olanzapine, clozapine, lithium, valproate, bupropion, and varenicline) and types of medications (second-generation antipsychotic and anticonvulsant) was examined with a series of chi square analyses; any significant association was followed up by multivariate analysis.
Results
Participant characteristics
The demographic and clinical characteristics and smoking status of the 991 participants, by diagnostic group, are presented in
Table 1. A majority of participants with psychiatric illness were enrolled from local psychiatric rehabilitation agencies (354 of 547, 65%), with the rest recruited from inpatient settings (132 of 547, 24%), day hospital programs (29 of 547, 5%), or office practices (32 of 547, 6%) at the research program site; recruitment setting was not significantly associated with smoking status. Almost all of the participants with schizophrenia or bipolar disorder (540 of 547, 99%) were receiving psychotropic medication at the time of their study enrollment. A total of 340 (81%) of the participants with schizophrenia and 61 (48%) of participants with bipolar disorder were receiving second-generation antipsychotic medications; 57 (14%) and 37 (29%), respectively, were receiving lithium; 148 (35%) and 75 (60%), respectively, were receiving an anticonvulsant medication; and 77 (18%) and 60 (48%), respectively, were receiving an antidepressant. A total of 43 (8%) were receiving bupropion, which may be used for smoking cessation, and no one was receiving varenicline, a smoking cessation medication.
Smoking prevalence and trends over time
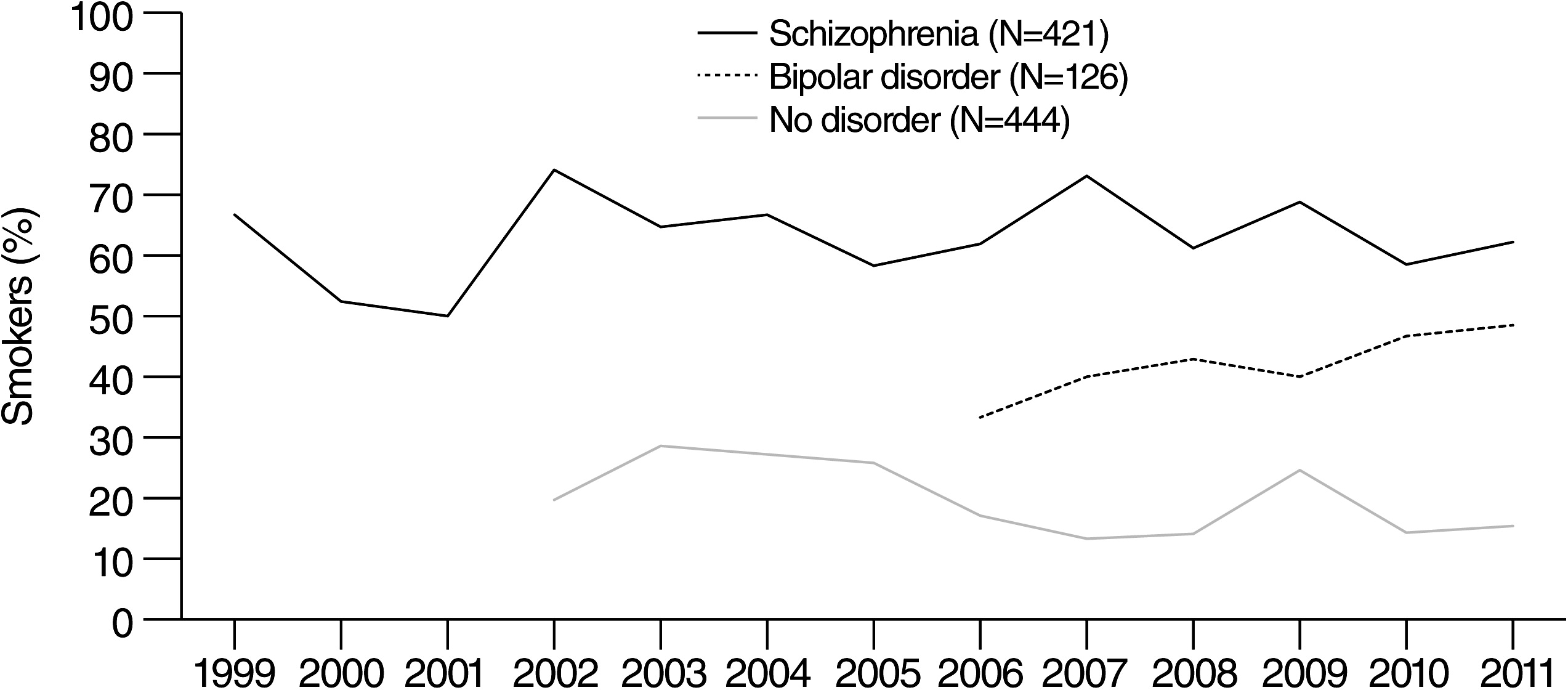
During the years of the study recruitment, a total of 268 of 421 (64%) individuals with schizophrenia, 55 of 126 (44%) with bipolar disorder, and 86 of 444 (19%) participants without psychiatric illness reported that they were current smokers. The prevalence of smoking in each group, by enrollment year, is shown in
Figure 1.
There was no statistically significant effect of recruitment year on smoking prevalence for any of the diagnostic groups (schizophrenia, bipolar disorder, or no disorder). An overall model consisting of diagnostic group, year, and diagnostic group × year interaction showed a statistically significant main effect for diagnostic group (χ2=182.5, df=2, p<.001) but no effect of year and no interaction. Adjusting for the covariates of age, race, and gender also did not affect the results.
Consumption of cigarettes and trends over time
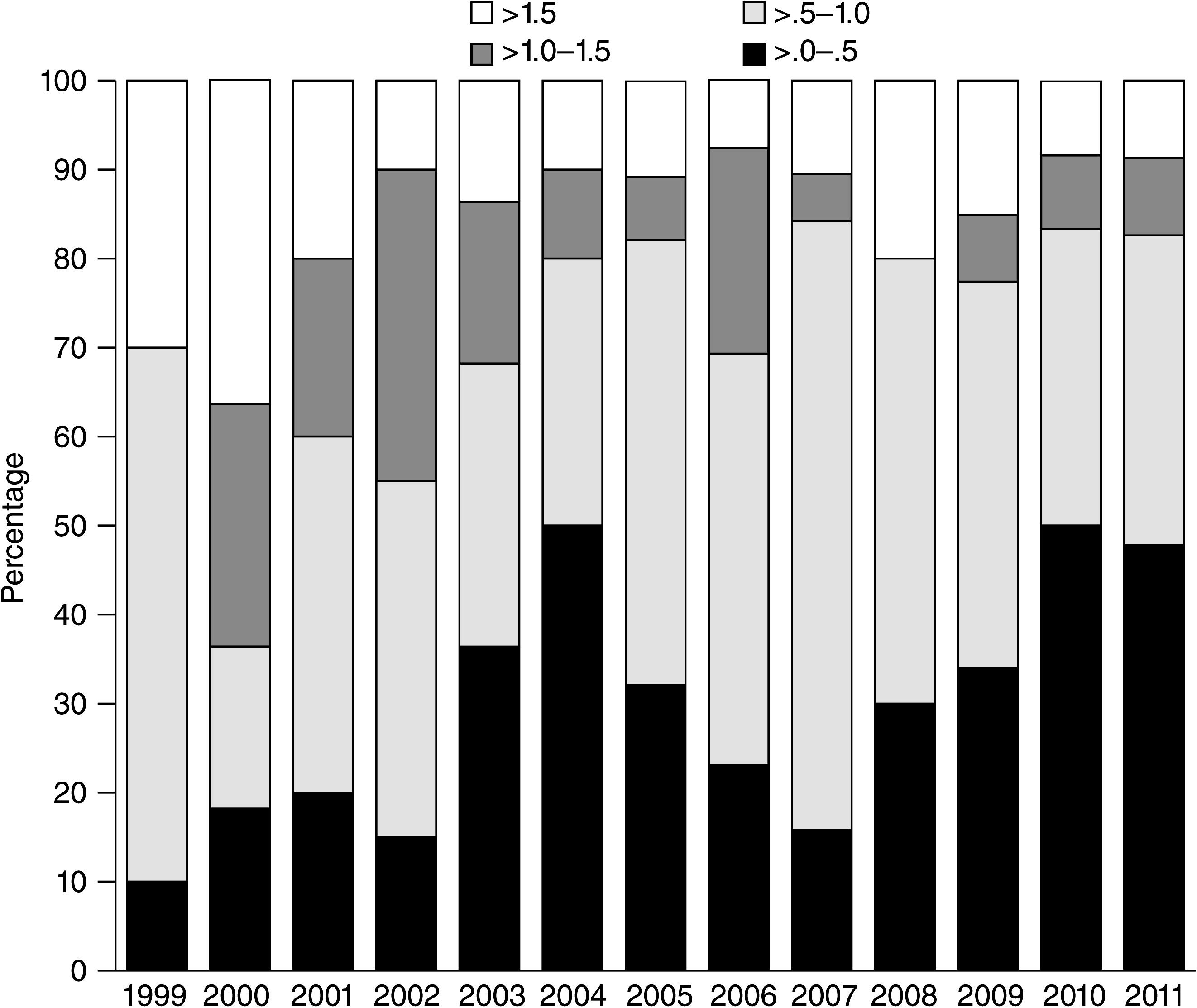
The quantity of cigarettes smoked per day by diagnostic group is shown in
Table 1 and by the smokers with schizophrenia is shown in
Figure 2. There were statistically significant decreases in cigarette consumption over the study period for smokers with schizophrenia (χ
2=12.9, df=3, p<.005) and for participants without mental illness (χ
2=15.5, df=3, p=.002) but not for smokers with bipolar disorder. For the smokers with schizophrenia, the log odds of being in the highest two consumption categories (>1.0–1.5 ppd and >1.5 ppd) relative to the lowest category (≤.5 ppd) decreased significantly over time (χ
2=10.3, df=1, p=.001, and χ
2=5.86, df=1, p=.016, respectively). For participants with no disorder, the likelihood of being in the consumption category >1.0–1.5 ppd, relative to the lowest category, <.5 ppd, showed a trend toward statistical significance (χ
2=2.92, df=1, p=.09). Adjusting for the covariates age, race, and gender did not change the results for the participants without a disorder, but the effect of year became nonsignificant for the smokers with schizophrenia.
An overall model consisting of diagnostic group, year, and diagnostic group × year interaction showed a highly significant effect of diagnostic group (χ2=65.4, df=6, p<.001), whereas neither the effect of study year nor the group × year interaction achieved statistical significance. When covariates age, race, and gender were added to the model, the effect of diagnostic group remained highly significant (χ2=50.8, df=6, p<.001), the effect of study year became nonsignificant, and the interaction term remained nonsignificant.
Correlates of tobacco use with mental illness
As shown in
Table 2, a multiple logistic regression model showed that across all years of study enrollment, current smoking among the participants with a psychiatric disorder was significantly associated with a longer duration of psychiatric illness, history of substance abuse, fewer years of education, Caucasian race, and schizophrenia compared with bipolar disorder diagnosis. In this model, we did not find a statistically significant association between smoking status and symptom severity as measured by the PANSS total score, gender, or socioeconomic status measured by maternal education. As also shown in
Table 2, an ordinal multiple logistic regression showed that the quantity of cigarettes consumed by the participants with mental illness was significantly associated with these same variables and with male gender.
Within the bipolar disorder and schizophrenia groups, there were no statistically significant associations between smoking status and receipt of selected specific medications (valproate, clozapine, olanzapine, or lithium) or classes of medication (anticonvulsant or any second-generation agent) except for bupropion, which was significantly and inversely associated with smoking for persons with schizophrenia (χ2=4.60, df=1, p=.032) but not for those with bipolar disorder. In a multivariate analysis with both mental illness groups, the odds of being a smoker and the quantity of cigarettes smoked were significantly lower for persons receiving bupropion (odds ratio=.41, 95% confidence interval=.21–.80, p=.009; z=–2.70, p=.007).
Discussion
We found marked differences in the prevalence of smoking and in the quantity of cigarette consumption among the diagnostic groups in this study. These group differences remained relatively constant over the observation period, and there were no significant time trends in prevalence of smoking or quantity of cigarettes consumed when analyses adjusted for demographic covariates.
The prevalence of smoking in our sample is generally consistent with, but at the lower end of, that observed in other recent U.S. cohorts of individuals with schizophrenia and bipolar disorder. In studies of schizophrenia published since 2000, the reported prevalence of smoking ranges from 61% to 88% (
4,
5,
17,
24). In the fewer studies of smoking with bipolar disorder, the reported prevalence ranges from 31% to 69% (
6,
19,
20,
33,
34). It is noteworthy that none of these previous studies compared persons enrolled at different time points to determine time trends as we did in this investigation.
In addition to showing differences in smoking between individuals with schizophrenia and individuals without a psychiatric disorder, our study also demonstrated that individuals with schizophrenia are more likely to be smokers and to consume larger numbers of cigarettes than individuals with bipolar disorder. With the exception of a study by Diaz and colleagues (
34), no studies have directly evaluated and compared smoking among individuals with schizophrenia and individuals with bipolar disorder in the same investigation. We enrolled individuals with either disorder from the same geographic area and treatment centers, and our analytic model included covariates that are also associated with smoking. Therefore, our comparisons between the two psychiatric groups are relatively free of obvious confounders.
The demographic and clinical correlates of smoking that we found are generally consistent with previous studies of smoking by persons with mental illness and mirror trends in the overall population: lower education (
1), male gender (
1,
4), a history of substance abuse (
5), and Caucasian race, though the latter is not found in all studies of persons with serious mental illness nor in the U.S. overall population (
1,
17–
20). We found no significant association between cigarette smoking or quantity of cigarettes consumed and the severity of psychiatric symptoms. Results of previous studies are mixed on this topic (
17,
18,
21–
24). Our data also suggest that cigarette smoking is not associated with the receipt of specific medications except bupropion. However, we do not know whether the lower amount of smoking by persons receiving bupropion was an effect of its use as a smoking cessation medication.
Strengths of our study include that we had a relatively large sample that included two groups with psychiatric illness and a control group with no psychiatric illness. Smoking was assessed among new study enrollees in a period that exceeded a decade, through 2011.
One limitation of our study was that we did not biochemically verify smoking status, although self-report of smoking is considered valid in epidemiological studies (
1). Another limitation was that we assessed smoking status only at study entry, so we do not know the change in smoking status or in the quantity of cigarettes consumed by participants over time. In addition, we did not collect data on the duration of smoking or quit attempts, which would be informative about the topography of smoking and provide data for additional comparisons between the groups.
Although our recruitment efforts were continual for the three diagnostic groups throughout the study period, enrollment into research studies is affected by many factors, and we cannot rule out the possibility that there may be unmeasured confounders that could distort the relationships among the groups or the apparent effects of time. It is also possible that the persons who participated in our studies are not fully representative of persons with these disorders in clinical settings because our participants voluntarily consented to a research study. However, smoking status was not a basis for inclusion in the study, so it is unlikely that participation introduced any clear bias with respect to smoking.
Finally, although our overall sample size was relatively large, individuals with bipolar disorder were underrepresented. In addition, we may have had limited power to detect time trends given the small number of individuals for some recruitment years for some diagnostic groups.
Conclusions
Our study demonstrates that the relatively high prevalence rates of smoking by individuals with schizophrenia or with bipolar disorder have persisted over the past decade despite increasing environmental restrictions on smoking, ongoing public health campaigns, rising cigarette prices, and growing stigma associated with smoking in many segments of the U.S. population (
35). Recently, there have been calls to action in the psychiatric community (
13,
36) and distribution of materials to promote smoking cessation among persons with serious mental illness (
37). A recommendation also has been made in one major schizophrenia practice guideline that people with schizophrenia who want to quit or reduce cigarette smoking should be offered treatment with bupropion, with or without nicotine replacement therapy, and that this pharmacological treatment should be accompanied by a smoking cessation education or support group (
38). However, these developments have not yet resulted in any substantive changes in smoking status or cigarette consumption for patients with schizophrenia or bipolar disorder in routine psychiatric settings. These results add urgency to the need for action to promote smoking cessation by persons with serious mental illness.
Acknowledgments and disclosures
This study was funded by grant 07R-1690 from the Stanley Medical Research Institute. The authors thank Melanie Bennett, Ph.D., for comments on a draft of the article.
Dr. Yolken is a member of the Stanley Medical Research Institute Board of Directors and Scientific Advisory Board. The terms of this arrangement are being managed by the Johns Hopkins University in accordance with its conflict of interest policies. The other authors report no competing interests.