Caring for veterans with posttraumatic stress disorder (PTSD) is one of the greatest challenges facing the Veterans Health Administration (VHA). Fortunately, several agencies have provided evidence-based treatment guidelines to improve PTSD care that emphasize the first-line treatments of serotonin reuptake-inhibiting agents, generally discourage the use of benzodiazepines, and marginally support the use of second-generation antipsychotics in certain situations on the basis of limited available evidence (
1–
6). Yet notwithstanding the efforts to disseminate these guidelines, current VHA prescribing rates of medications without strong guideline support remain high (
7,
8).
As a recognized leader in the delivery of high-quality care, the VHA is ideally positioned to improve the management of PTSD, but important questions remain. For example, there is great variation in the prescribing of benzodiazepines across the VHA (
9). It is possible that such variation reflects the complexity of PTSD cases in the veteran population. For example, insomnia is the most common symptom reported by veterans with PTSD, and anxiety symptoms often co-occur, both of which are very responsive to benzodiazepines (
10). Historically, PTSD treatment in the VA relied heavily on the use of benzodiazepines, and at one point diazepam was the top-selling psychotropic medication worldwide (
11). Some studies even suggest that tapering benzodiazepines can be problematic; tapering alprazolam for eight combat veterans with PTSD who were chronic users of the drug exacerbated their symptoms (
12). Because of these issues, it is possible that differences in provider beliefs about the effectiveness of benzodiazepine treatment accounts for the wide variation in prescribing of these medications at VHA facilities (
8,
9). Therefore, in order to change this practice, the initial focus must be on identifying and eliminating the key sources of variation.
There are two main practice settings in which medications for PTSD are commonly prescribed—primary care and mental health care. In theory, primary care providers could be driving the use of benzodiazepine prescribing for PTSD. First, all veterans enrolled in VHA care enter through the primary care gateway, whereas only 30%–70% of veterans see a mental health provider. Veterans may be treated in primary care because their mental disorder is uncomplicated, falling within the scope of primary care. Alternatively, the treatment setting may reflect an individual’s refusal to accept a mental health referral (
13). Because a growing percentage of VHA mental health treatment is taking place in primary care settings, we must consider the possibility that primary care physicians are responsible for most of the benzodiazepine prescriptions, either for non–mental health complaints (for example, restless legs, medical procedures, and sleep disorders) or for mental health problems. Second, given the broad scope of primary care, it may not be reasonable to expect these clinicians to be familiar with the clinical practice guideline for PTSD developed by the U.S. Department of Veterans Affairs (VA) and the U.S. Department of Defense (DoD) (
5). In contrast, mental health clinicians should be highly knowledgeable regarding the PTSD practice guideline and, therefore, less likely to prescribe benzodiazepines.
The degree of variation in psychiatric medication use between VHA facilities has also been raised as a concern. The current VHA system comprises roughly 140 main medical centers and close to 900 community-based clinics, and several studies have demonstrated a large degree of facility-level variation (
9,
14,
15). Unfortunately, we do not understand how the behavior of mental health clinicians contributes to such facility variation in prescribing practices.
Thus, as part of a larger initiative aimed to assess guideline-concordant care of veterans with PTSD, we conducted this study of fiscal year (FY) 2009 data with the primary aim of identifying prescribing frequencies attributable to various provider types. We hypothesized that primary care providers would constitute a major proportion of the prescribing of non–guideline-supported medications to veterans with PTSD. To provide context for interpreting the rates of non–guideline-based therapies, we also evaluated the associations between provider type and selective serotonin–norepinephrine reuptake inhibitors (SSRI/SNRIs) and second-generation antipsychotics. Further analyses examined variation across VHA facilities in overall prescribing frequency and variation attributed to provider types for these medications.
Methods
Study design and data sources
A cross-sectional study was conducted using national VHA pharmacy and clinical administrative data for FY 2009 obtained from the Austin Information Technology Center. Data sources were linked by using unique identifiers to combine prescription drug utilization from inpatient and outpatient encounters. The Decision Support System identified the medications, dose, days’ supply, and dates filled. The Outpatient Care Files and Inpatient Treatment Files identified demographic variables of interest (for example, age, sex, area of residence, and period of service) and psychiatric comorbidities of interest. Each of these data sources has been extensively studied (
1,
2,
4,
7,
11).
Patient population
The study population of interest was veterans with PTSD who were regular users of any VHA-prescribed medications provided in FY 2009. To start, veterans with at least one inpatient or outpatient encounter-based diagnosis of PTSD were identified by using the
ICD-9 code 309.81. This algorithm has been used in prior research examining PTSD, and the miscoding event rate has been shown to be infrequent (<4%) (
4,
11,
16–
18). Next, regular VHA medication use was identified during FY 2009. This was defined by an outpatient medication refill pattern in which the days’ supply periods spanned at least 240 days of 365 days available in the fiscal year (
19). This criterion excluded patients who were intermittent users of VHA pharmacy services or who were not receiving pharmacotherapy.
Data elements and outcomes
The primary intentions were to identify the proportion of prescribing for each class of medication that was attributable to mental health care and primary care clinicians and to describe variation in prescribing frequency at the facility level for all medication users and among the subgroup accessing mental health care.
Variable definitions
Medication use.
The study examined use of three medication classes. The classes were chosen to represent the spectrum of level-of-evidence ratings as specified in the VA-DoD clinical practice guideline for PTSD (
5). The first class included the SSRI/SNRIs, which have a level A rating, indicating that clinicians should provide these medications to eligible veterans with PTSD. The second medication class was the second-generation antipsychotics. These medications have been judged to have insufficient evidence for recommendation (level I) when used as monotherapy or as adjunctive therapy. The most recent exception according to the 2010 VA-DoD guidelines is risperidone, which has received a recommendation against routine use as an adjunctive medication for PTSD (level D rating). The third medication class included benzodiazepines, which have also received a level D rating. [A table listing the individual medications in each class is included in an online
data supplement to this article.] Medication use was based on the presence of at least one outpatient prescription fill during FY 2009 for any quantity, days’ supply, or dosage for the three drug classes.
Provider type and facility.
Provider types were identified by using the prescription drug files and categorized as psychiatrists and other mental health prescribers, primary care clinicians, and other prescribers. Other prescribers were defined as nonphysician prescribers (for example, advance practice nurse practitioners and physician assistants) credentialed to prescribe as mental health providers. All other credentialed prescriber types not defined in the above categories were defined as other prescribers (for example, nonpsychiatric subspecialty providers). When within-class prescriptions had more than one provider type, provider type was assigned to the most frequent prescriber type for that class. In facility-level analyses, each patient was assigned to one of the 137 VHA main facilities that accounted for the greatest number of PTSD encounters during FY 2009.
Comorbid mental health conditions.
Using a strategy similar to that for identifying PTSD, we also sought to highlight the prevalence rates of several other comorbid psychiatric disorders in the sample, recognizing that for many of these comorbid disorders the U.S. Food and Drug Administration has approved use of medications that have a level D rating in the PTSD guidelines. The
ICD-9 codes used to identify these disorders have been described elsewhere (
20).
Analyses
Descriptive statistics were used to examine the demographic and clinical characteristics of the study sample. The goals of the primary analysis were to report the prescribing frequency for three target medication classes (SSRI/SNRIs, second-generation antipsychotics, and benzodiazepines) and then to report the proportion accounted for by mental health specialists versus other types of providers. In addition to reporting our findings for the main study sample, we included several sensitivity analyses to examine the stability of our findings using different methodological approaches. These included restricting the analysis to patients who accessed mental health specialty care, applying two alternate case definitions for identifying patients with PTSD, requiring at least 90 days of medication use to define exposure, and applying an identical methodology to a different fiscal year (FY 2006).
Access to mental health specialty care was defined as receiving a prescription for any medication from a mental health provider. This subgroup specifically identifies patients who received medications from both primary care and mental health prescribers. Therefore, analysis of data from this subgroup assessed the shift in prescribing rates by provider type once patients had access to mental health prescribers. Alternative PTSD-coding algorithms were examined in order to assess any impact on prescribing rates related to the different methods of identifying PTSD. The first algorithm identified PTSD codes only when they were listed in either the primary or secondary coding position for at least one inpatient encounter or at least two outpatient encounters. The second algorithm limited the cohort to PTSD codes for any inpatient or outpatient encounter when PTSD was in the primary coding position only.
The final goal of the analysis was to evaluate the degree of variation across VHA facilities in prescribing frequencies and in the proportion of prescribing attributable to mental health specialists. Facility-level frequencies for both of these variables were determined for each of 137 VHA facilities, and variation was characterized in box plots using median and interquartile ranges (IQR).
Results
As a result of our cohort selection process, 356,958 veterans with PTSD were identified who also received regular VHA medication prescriptions in FY 2009. The average age of the study sample was 57.4 years, and most veterans in the sample were white males who had served during the Vietnam era (65.0%).
Table 1 presents data on other demographic and clinical characteristics of the sample.
Rates of use by provider type
Table 2 presents data on prescribing frequencies and provider types. In the primary analysis of the FY 2009 sample of 356,958 patients, 65.7% received a prescription for an SSRI/SNRI, 37.0% received a benzodiazepine prescription, and 25.6% received a prescription for a second-generation antipsychotic. Mental health clinicians accounted for a majority of prescribing across all three medication classes, 70.0% for SSRI/SNRIs, 79.7% for second-generation antipsychotics, and 68.8% for benzodiazepines.
Sensitivity analyses
Table 2 also presents results of the sensitivity analyses. The first analysis required at least 90 days of medication exposure (the primary analysis looked at use of any duration). Overall prescribing frequencies diminished as a result of the more restrictive definition. The proportion of prescriptions by mental health providers was relatively unchanged for SSRI/SNRIs (70.2% versus 70.0% in the primary analysis) and second-generation antipsychotics (80.2% versus 79.7%) but was somewhat increased for benzodiazepines (72.7% versus 68.8%).
The second sensitivity analysis focused on the subgroup of patients accessing mental health specialty care (N=259,495), which represented 72.7% of the overall sample. The demographic and clinical characteristics of this subgroup were similar to those of the overall group, except the subgroup tended to be younger and from a post-Vietnam era, to be female, and to come from urban areas (data not shown). In addition, this subgroup had slightly higher rates of comorbid psychiatric disorders. Compared with the overall sample, prescribing for this subgroup shifted toward prescribing by mental health providers: SSRI/SNRIs, 84.1%; second-generation antipsychotics, 87.4%; and benzodiazepines, 80.4% (
Table 2).
Use of alternative PTSD diagnostic coding algorithms had little impact on our findings (
Table 2). Finally, prescribing frequencies for second-generation antipsychotics and benzodiazepines were slightly higher in FY 2006 than in FY 2009. The data suggest that the prescribing frequencies for these medications declined because a lower proportion of the prescribing was done by mental health providers, whereas the proportion done by primary care providers increased slightly (
Table 2). In comparison, rates of SSRI/SNRI prescribing remained relatively flat between FY 2006 and FY 2009.
Facility variation
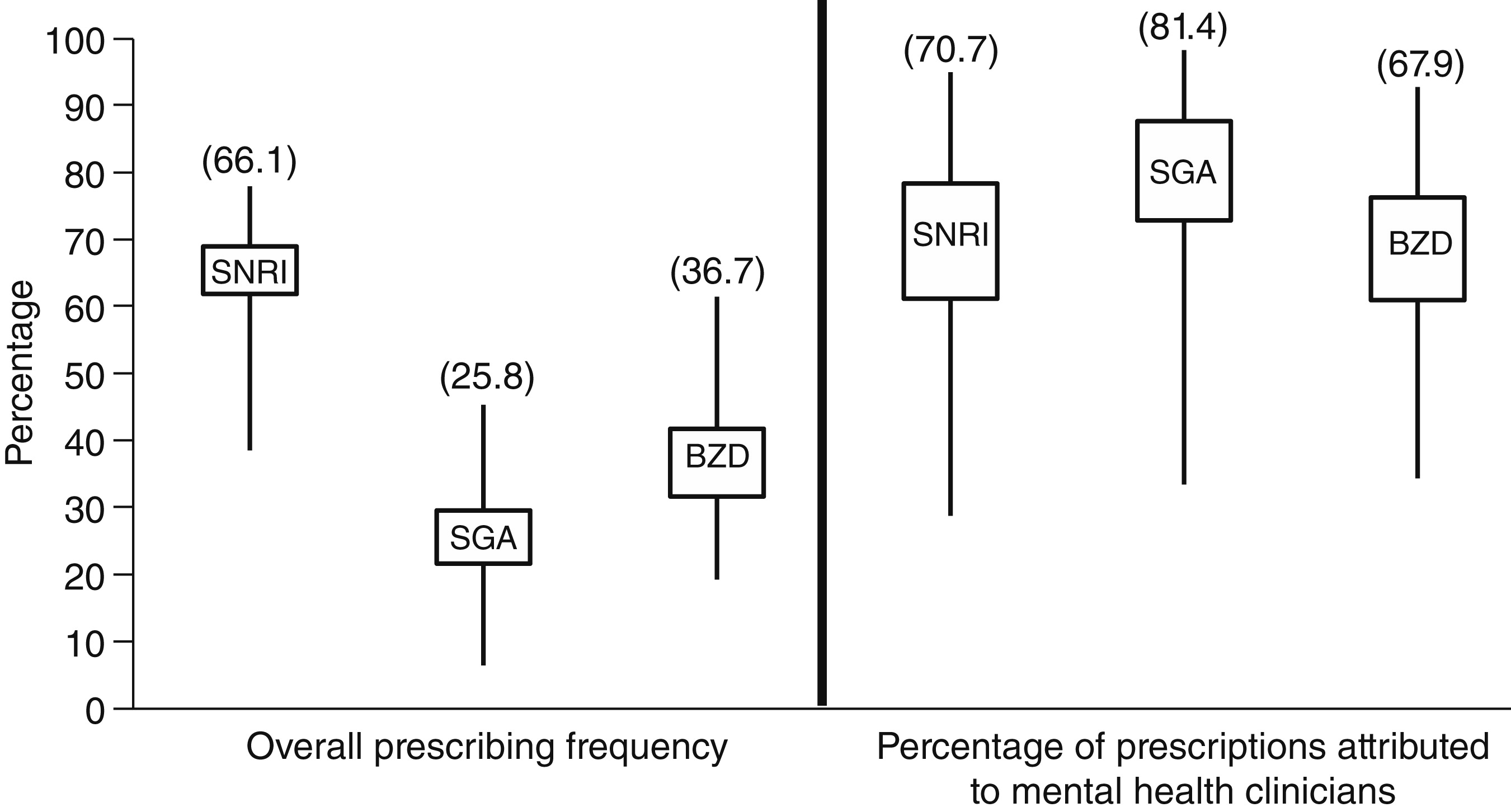
The final objective was to examine variation in prescribing frequency and proportion attributable to mental health providers across VHA facilities (
Figure 1). The median facility-level prescribing frequency for SSRI/SNRIs was 66.1%. The 25th percentile of SSRI/SNRI prescribing was 61.9%, and the 75th percentile was 69.0%, yielding an IQR of 7.1%. The degree of variation as expressed by IQR was slightly more for second-generation antipsychotics (IQR=7.9%) and was highest for benzodiazepines (IQR=10.1%).
Figure 1 also shows the variability in the proportion of prescribing accounted by mental health providers. The overall degree of variability was wide; mental health prescribers accounted for <40% of prescribing in some facilities but more than 90% in others.
Discussion
Our primary objective was to identify the prescribing frequencies for three classes of medications rated in the VA-DoD PTSD guideline and the proportions attributable to various provider types. Our primary finding suggests that non–guideline-recommended treatments (for example, benzodiazepines) are frequently prescribed by mental health clinicians for veterans with PTSD. This finding is contrary to our hypothesis and suggests that prescribing by mental health care specialists contributes considerably to the misalignment between guideline-based care and actual practice. The level of variation between facilities among all medication users was modest for the three classes of medications. However, when the analysis examined facility-level variation in prescriptions from a mental health care specialist, greater variability across each of the classes was found; the greatest variation occurred for SSRI/SNRI medications.
These findings represent a unique set of analyses of VHA pharmacy data and provide a novel perspective on prescribing practices among VHA clinicians, particularly with regard to adherence to guideline-based pharmacotherapy for PTSD. There are limits to what one can infer from archival data such as these, but our findings raise a number of questions about why current prescribing guidelines are inconsistently adopted by mental health clinicians. How well are clinicians familiar with these guidelines? Are clinicians familiar with the guidelines but disregarding them because they are not convinced by the scientific evidence? Do clinicians consider the guidelines inapplicable to the psychiatric patients under their care, many of whom have complex illness profiles with high rates of comorbidity? Although each of these scenarios may apply, other research on the alignment between guidelines and practice patterns has identified clinicians’ lack of awareness of guidelines as one of the most common barriers to best pharmacotherapeutic practices (
21).
To place our findings in context, others have demonstrated treatment variability by provider type outside the VA. In a study by Weisberg and colleagues (
22), 539 primary care patients with an anxiety disorder were interviewed to determine differences in prescribing rates of SSRI/SNRIs and benzodiazepines by provider type. Among patients with an anxiety disorder who received medication, mental health and primary care clinicians tended to prescribe SSRI/SNRIs at similar rates. In contrast, benzodiazepine prescribing was twice as high among patients who accessed specialty mental health care (45%) than among those who accessed treatment in primary care (24%). Although our study is not directly comparable, our findings are generally consistent in that mental health clinicians in our study prescribed benzodiazepines for patients with PTSD at approximately twice the rate of primary care providers.
We also found differences in the level of variation between facilities for all medication users and for those who received prescriptions from mental health providers. We recognize that this is not a new discovery; previous research has found that benzodiazepine prescribing for veterans with depression varied across facilities (
8). However, our findings deepen understanding in regard to the main prescribing source. From a national perspective, most veterans with PTSD who received treatment in a VHA facility received at least one prescription from a mental health provider (median 73.1%); however, rates of prescribing by mental health providers in some facilities were as low as 44%. Examining the variation across facilities allowed us to determine the proportion of variation attributable to mental health care providers. We found facility-level variation in the proportion of prescriptions from these practitioners for all three classes of medications (
Figure 1). This finding is novel and deserves further investigation, especially to determine whether the variation reflects lack of knowledge of evidence-based pharmacotherapy for PTSD.
As systems place more emphasis on standardizing practices based on clinical guidelines, balancing the desire to achieve symptomatic relief while following the guidelines has never been more challenging for clinicians. It is a difficult task to accurately determine whether the benefit of a benzodiazepine will outweigh the risk of polypharmacy or abuse potential. Many mental health providers “inherit” patients who previously received benzodiazepines from other clinicians, creating an immediate tension as the clinician seeks to balance individual patient factors with the need to provide guideline-supported care. In our study 65% of veterans receiving mental health care for PTSD had served in Vietnam, and many of these veterans were started on benzodiazepines by non-VHA physicians or were started before the development of practice guidelines recommending against benzodiazepine pharmacotherapy for PTSD. Once these medications are started, it is difficult to terminate them (
23). Fortunately, the results of randomized controlled trials can guide clinicians in regard to safe and effective benzodiazepine tapering for chronic users (
23,
24).
Competing indications for benzodiazepines among veterans with PTSD may also justify prescription. In addition, benzodiazepines are sometimes used as bridge therapy for symptomatic relief when a patient is started on SSRI/SNRIs, which can initially worsen symptoms of anxiety. Nonetheless, we did not find rates of comorbidity sufficient to justify the magnitude of benzodiazepine prescribing for these patients, especially in light of the weight of evidence of contraindications. We recognize that setting a goal of zero benzodiazepine use seems unreasonable because many patients with PTSD have used benzodiazepines for long periods without evidence of harm and possibly with some benefit for co-occurring symptoms or disorders. Our findings, however, clearly indicate that further work is needed to determine whether the high rates of benzodiazepine prescribing reflect a difficult and complex patient profile or a failure to effectively disseminate current practice guidelines that recommend against prescribing benzodiazepines for PTSD.
Several limitations in this study require comment. Our results are somewhat different from those of a recent study by Jain and colleagues (
25). These authors analyzed survey responses of 482 veterans with PTSD and concluded that prescribing practice may have been in concordance with existing guidelines when their analysis accounted for the presence of comorbid psychiatric disorders with potential indications for benzodiazepines. However, these authors also noted that a number of patients received benzodiazepines before first-line pharmacotherapy had been prescribed. Ultimately, our data could not differentiate between patients with varying degrees of symptom severity. Clinicians in mental health settings are more likely to be responsible for the treatment of veterans with a greater burden of PTSD symptoms and complex comorbid conditions, which are important factors to consider in evaluating our findings.
Some of the patients in the subgroup that received prescriptions from a mental health provider may have had only minimal contact with the mental health provider, who prescribed refills for medications previously prescribed for nonpsychiatric indications in order to see the patients through to their next primary care visit. A primary care provider may have been providing a similar service to another patient subgroup. Primary care providers may triage veterans with PTSD to mental health care settings at higher rates than veterans with depression or generalized anxiety disorder—disorders with which primary care providers have more experience. Primary care providers’ greater experience in managing depression compared with PTSD is likely to affect referral patterns and prescribing differences.
The methods used to identify PTSD may also be subject to interpretation. We identified PTSD codes in administrative data that represented either the primary diagnosis or a secondary diagnosis. For example, a condition such as panic disorder may have been the primary diagnosis, with PTSD as the secondary diagnosis (or comorbid condition). In such situations, use of a benzodiazepine would have been appropriate. This limitation affects our ability to interpret the appropriateness of a given therapy. Finally, the sample represents an older, male veteran population that may not be representative of other populations. This research explicitly addresses a previously unanswered—and recently highlighted—question regarding the influence of clinician type on benzodiazepine prescribing (
26).
Implementing evidence-based treatments in everyday practice remains challenging. According to Corrigan and colleagues (
27), many factors contribute to the failure to achieve this goal, including service providers’ attitudes, lack of organizational leadership, and insufficient resources dedicated to practitioner education and clinical staff development. Although our study cannot offer insights into which factor is most responsible, it emphasizes the need for research to identify the clinical and system factors that differentially influence provider behavior with respect to prescribing benzodiazepines.
Conclusions
In this study of veterans with PTSD who were receiving medications prescribed by VHA clinicians, 37.0% received a benzodiazepine. In a subgroup of those who accessed care in VHA mental health settings, 43.6% received a benzodiazepine. These findings indicate that non–guideline-supported pharmacotherapy for veterans with PTSD is frequently practiced. Furthermore, our data showed that mental health clinicians provided alarger proportion of these prescriptions than other types of practitioners. We hope that future research will lead to greater understanding of these findings.
Acknowledgments and disclosures
This project was supported by the U.S. Department of Veterans Affairs (VA) Mental Health Quality Enhancement Research Initiative (RRP 11-001). Additional support was provided by career development awards from the VA Health Services Research and Development Service (Dr. Abrams: CDA 10-016; Dr. Lund: CDA 10-017) and the National Center for PTSD at the White River Junction VA Medical Center. None of these sponsors had any role in the study design, methods, analyses, or interpretation or in the preparation of the manuscript and the decision to submit it for publication. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VHA.
The authors report no competing interests.