In recent years, suicide among veterans has become a national concern, largely because of questions raised about the human costs of Operation Enduring Freedom and Operation Iraqi Freedom (OEF/OIF), the wars in Afghanistan and Iraq. As these wars progressed, increased funding was allocated to services provided by the Veterans Health Administration (VHA), the health care system of the Department of Veterans Affairs (VA). VHA began to enhance its mental health services in 2005. Although these enhancements are continuing, the end of OIF and the projected end of OEF provide a useful time for review of the extent to which the provision of enhanced services led to decreases in suicide rates. For VHA, the goals of this review were to evaluate the impact of its mental health enhancements. For the country as a whole, this evaluation can identify lessons to be learned from VHA that could be applied more broadly.
Key findings about suicide among individuals who utilize VHA services are publicly available in reports and in Congressional testimony (
1–
9). To summarize, the suicide rate among those who utilized VHA services was 35.1 per 100,000 patients per year (37.3 among men and 13.7 among women) in 2005 and 35.9 (38.3 among men and 12.8 among women) in 2009, the most recent year for which data are available. During this time, mental health enhancements led to major increases in total mental health staffing in VA medical centers and clinics, where staffing grew 36.7% from 2005 to 2009, or from 13,567 to 18,543. The increase was particularly notable in outpatient mental health staffing, which grew by 52.8%, or from 6,031 in 2005 to 9,218 in 2009. Partially offsetting these staff increases, the population of VHA patients grew by 6.7%, from 5.01 million in 2005 to 5.35 million in 2009, and the number of veterans with confirmed mental health conditions grew by 28.1%, from 887,613 in 2005 to 1,136,731 in 2009. Overall, total mental health staffing per 1,000 mental health patients increased by 6.72%, or from 15.3 in 2005 to 16.3 in 2009. Outpatient mental health staffing per 1,000 mental health patients grew by 19.3%, from 6.80 in 2005 to 8.11 in 2009.
Because the increases in mental health staffing from 2005 to 2009 were substantial, the observation that increases of this magnitude could occur without an associated decrease in suicide rates raises questions for VHA about the relationship between mental health services and suicide prevention. Moreover, to the extent that it is possible to generalize from observations in VHA to other health care systems, these questions are salient for the nation as a whole. However, before drawing conclusions from this observation, it is important to evaluate the VHA system in greater detail. Because some degree of variability is inevitable in the implementation of any major program changes, this evaluation considered the relationship between mental health staffing and suicide rates across VHA’s 21 regional Veterans Integrated Service Networks (VISNs). The null hypothesis was that there were no associations across the VISNs between proportional changes in mental health staffing and proportional changes in suicide rates. The alternative hypothesis was that changes in mental health staffing were associated with changes in suicide rates across the VISNs and, therefore, that the effect observed in the system as a whole was a result of counterbalancing between effects that occur in different regions. Disproving the null hypothesis would essentially confirm a potential role for enhancing mental health services as part of suicide prevention.
Health and mental health and suicide prevention in the VHA
The VHA provides health care services to 8.34 million enrolled veterans in 152 hospitals and 807 community-based outpatient clinics located in 21 VISNs (
10). Eligibility is based on assignment to one of eight priority groups on the basis of criteria such as the presence and degree of service-connected disability, disability from other causes, specific exposures during military service, and income levels. In addition, veterans who served in OEF/OIF are eligible for services regardless of other criteria during the first five years after they return from deployment.
As previously described (
11), VA’s suicide prevention program is based on the principle that prevention requires ready access to high-quality mental health services, supplemented by two additional components: public education and awareness programs promoting engagement for those who need help, and specific services addressing the needs of those at high risk. Policy requirements for increased access and the implementation of evidence-based, recovery-oriented care were supported through increased mental health staffing and the adoption of the 2008 handbook
Uniform Mental Health Services in VA Medical Centers and Clinics (
12), a policy document that specifies the services that must be available to all veterans with mental health conditions. For suicide prevention specifically, establishing the program included creating a national office for suicide prevention, partnering with the Substance Abuse and Mental Health Services Administration and its Lifeline to add a veterans’ call center to its national 800–273-TALK crisis line (
13), and funding suicide prevention coordinators (SPCs) with support staff in each VA medical center and in the largest outpatient clinics. The SPCs at each facility receive referrals from the hotline, facilitate coordination and care of suicidal patients within the facility, and conduct outreach to providers and stakeholders in the community.
Other actions included policy requirements for screening at least annually of all VA patients for common mental health conditions, with follow-up evaluation of the risk of suicide among those who screen positive; for identifying veterans at high risk of suicide and for ensuring that they receive enhanced care; and for using safety planning (
14) as an intervention for those at high risk. Parts of the program that are still evolving include collaborations with the U.S. Department of Defense, extensions of the crisis line to include an Internet chat function and other novel mechanisms for forming connections, and systems of surveillance for nonfatal and repeated suicide attempts.
Methods
Data sources
Suicide rates among patients utilizing VHA health care services were derived from causes of death obtained from the National Death Index and VHA clinical and administrative records for 2005 and 2009. As previously described (
1), the population at risk for each year was the number of individuals who were alive at the beginning of the year and who used services during that year or the previous year. Information about the patient population and about staffing was derived from VHA clinical and administrative records. The calculation of staffing per 1,000 mental health patients was based on those with confirmed mental health conditions, that is, conditions that were noted on at least one inpatient mental health admission or two outpatient clinical encounters regardless of the setting and regardless of whether the condition was a focus of treatment. Comparisons across VISNs used measures of proportional change for suicide rates and mental health staffing or mental health staffing per 1,000 mental health patients calculated as the value for each variable for 2009 divided by the value for 2005.
Statistical analyses
VISNs were selected as the most practical level for analysis and inference because the average number of suicides per VISN per year, 92.39 in 2009, is large and stable enough to allow relevant analyses. In contrast, analyses at the level of the individual medical center, where the average number of suicides per year is 13 or 14, would require pooling across years, with decreasing resolution for evaluating changes over time. Analyses were conducted utilizing IBM SPSS, version 20.
Results
Between 2005 and 2009, the average VISN-level changes in mental health staffing, mental health staffing per 1,000 mental health patients, the size of the patient population, and suicides rates paralleled the observations for the system as a whole (
Table 1). Further analyses were conducted to evaluate the relationships between the changes in these measures across VHA’s 21 VISNs.
Significant correlations were found between proportional changes in suicide rates and measures related to staffing allocated to outpatient services. However, no significant correlations were found between changes in suicide rates and changes in total staffing or staffing of inpatient services, residential care, and mental health intensive case management (
Table 2). Correlations were significant for both proportional increases in mental health outpatient staffing and mental health outpatient staffing per 1,000 mental health patients. Other analyses, not shown, did not find any significant associations between suicide rates and mental health staffing by discipline (for example, psychiatrists, psychologists, social workers, or nurses) or within outpatient subspecialty programs (for example, programs focusing on posttraumatic stress disorder, substance abuse, or psychosocial rehabilitation).
Other analyses compared VISNs that had greater and lesser staffing enhancements. The median VISN increased mental health outpatient staffing from 2005 to 2009 by a factor of 1.62. The ten VISNs above the median had an average increase in mental health outpatient staffing of 73.9%±10.6%, with increases ranging from 62.6% to 93.6%. In contrast, the ten VISNs below the median had an average increase in staffing of 39.3%±12.3%, with increases ranging from 22.1% to 61.1% (F=46.42, df=1 and 18, p<.001).
The VISNs above the median had an average decrease in suicide rates of 12.6%±11.7%, with changes ranging from an increase of .3% to a decrease of 33.0%. In contrast, those below the median had an average increase in suicide rates of 11.6%±25.1%, with changes ranging from an increase of 57.4% to a decrease of 29.6% (F=10.4, df=1 and 18, p=.005).
The median VISN increased mental health staffing per 1,000 mental health patients by a factor of 1.21. The ten VISNs above the median had an average increase in mental health outpatient staffing per 1,000 mental health patient of 36.5%±10.5%, with increases ranging from 21.1% to 53.0%. In contrast, the ten VISNs below the median had an average staffing increase of 9.6%±8.2%, with changes ranging from a decrease of 6.0% to an increase of 20.8% (F=40.5, df=1 and 18, p<.001). Those above the median had an average decrease in suicide rates of 11.2%±13.8%, with changes ranging from a decrease of 32.1% to an increase of 12.2%. In contrast, those below the median had an average increase of 13.8%±25.7%, with changes ranging from a decrease of 29.6% to an increase of 57.4% (F=7.36, df=1 and 18, p=.014).
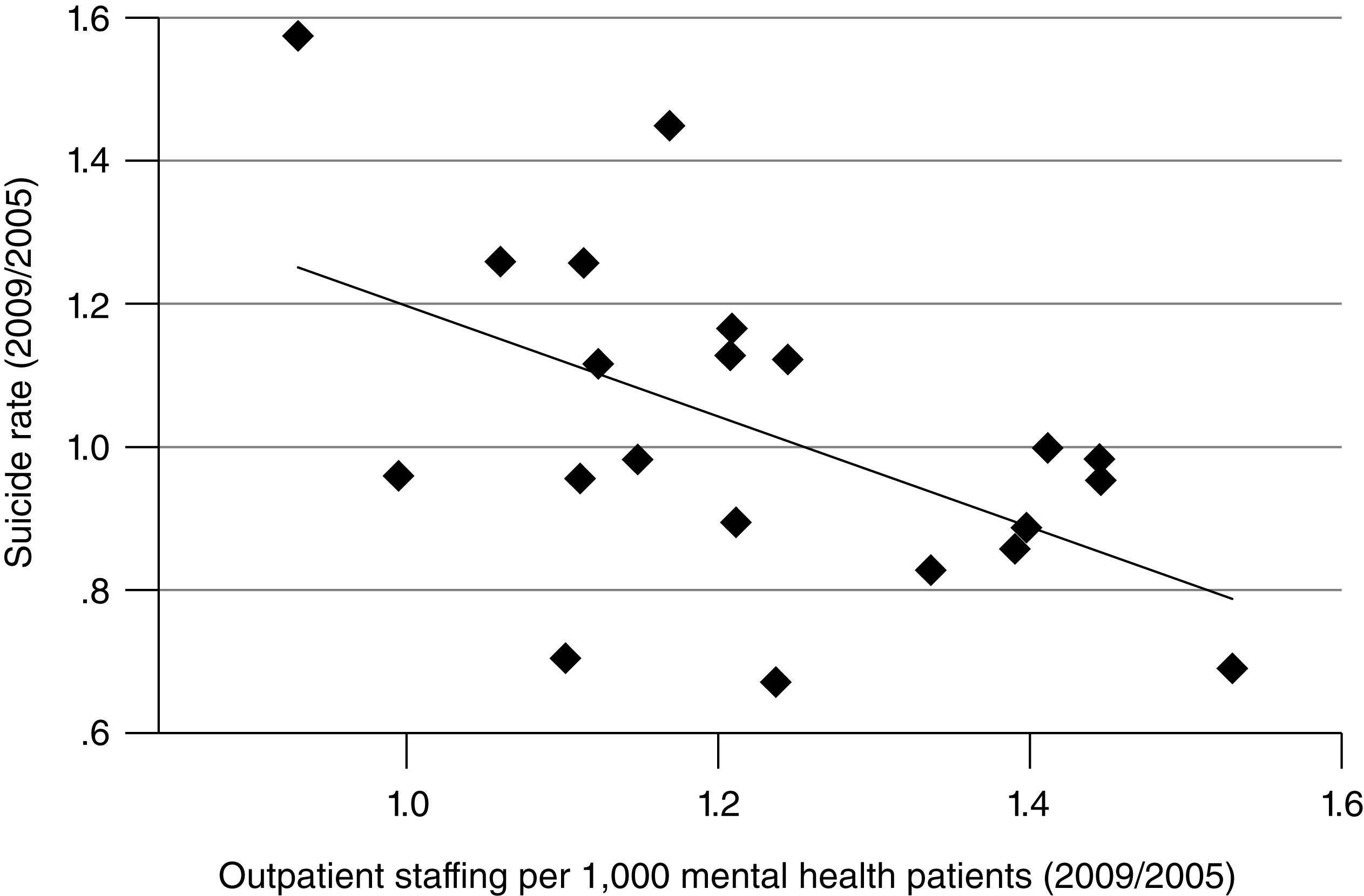
Regression analyses were used to model the associations of changes in staffing with changes in suicide rates and to estimate effect sizes (
Figures 1 and
2). The association between proportional changes in outpatient mental health staffing and proportional changes in suicide rates fit model 1, with R
2=.21, p=.039:
The estimate for the intercept was 1.83 (95% confidence interval [CI]=1.06–2.61), and for the slope, the estimate was –.52 (CI=1.01 to –.03). Based on these estimates, a 10% decrease in the suicide rate from 2005 to 2009 in the average VISN would correspond to a 36.8% increase in outpatient mental health staffing.
The association between proportional changes in outpatient staffing per 1,000 mental health patients and in suicide rates fit model 2, with R
2=.28, p=.013:
The estimate for the intercept was 1.97 (CI=1.24–2.70), and the estimate for the slope was –.00077 (CI=–.00136 to –.00003). Based on these estimates, a 10% decrease in the suicide rate from 2005 to 2009 in the average VISN would correspond to a 27.5% increase in outpatient mental health staffing.
Discussion
For VHA, these analyses were conducted primarily to evaluate its mental health and suicide prevention programs. The substantial mental health enhancements that occurred between 2005 and 2009 included increases in mental health staffing, requirements for the implementation of evidence-based care, and a specific program for suicide prevention. However, these enhancements did not lead to overall decreases in suicide rates among veterans who utilized VHA health care services.
As discussed above, this observation leads to a number of questions. First, for VHA, it raises questions about whether the mental health enhancements were the right ones to achieve suicide prevention as an outcome. Second, for VHA and others, the finding that major increases in mental health staffing can occur without an associated decrease in suicide rates raises basic system-level questions about the relationship between mental health services and suicide prevention.
A number of factors could have obscured effects related to staff increases, including an unstable baseline related to changes in suicide rates that occurred before the mental health enhancements (
11) and increases in suicide rates in middle-aged and “young-old” men in the overall population of the country since 2005 (
15). The analyses reported here were conducted to determine whether the lack of an overall effect could be explained, in part, through effects such as these together with variability between VISNs in the extent to which they implemented the mental health enhancements, as evaluated by using increases in mental health staffing as a metric.
The findings reported here demonstrate that proportional changes in suicide rates from 2005 to 2009 were related to proportional changes in mental health outpatient staffing, measured either as the ratio of outpatient staffing in 2009 divided by this parameter in 2005 or as the ratio of outpatient staffing per 1,000 mental health patients in 2009 divided by this parameter in 2005. Other analyses compared changes in suicide rates in the VISNs above and below the median for staffing increases and found that VISNs with the greatest proportional increases in mental health outpatient staffing had decreases in suicide rates of 11%–13% while those with the lowest proportional increases had increases in suicide rates of 14%–16%. The most reasonable explanation for these findings is that VHA’s mental health enhancements and its suicide prevention program were effective but that the enhancements led to decreases in suicide rates only where staffing increases were greatest.
Other analyses were conducted to estimate effect sizes. Calculations based on linear regression models allowed the estimate that, for the average VISN, it would have required a 25.7%–36.8% increase in mental health outpatient staff members over 2005 levels to decrease suicide rates by 10%. Further analyses are needed to evaluate potential mediators of the observed effects. Possibilities include improvements in access, the intensity of mental health services for those who use them, the quality of the care provided, and the provision of specific evidence-based treatments. It is important to recognize that it is not possible to apply this estimate across all VISNs, to use it to predict the impact of further changes in the system, or to estimate the staffing increases required to achieve the aspirational goal of eliminating suicide (
16).
Limitations in the methods and conclusions lie in the retrospective, observational nature of the design. Accordingly, it is not possible to distinguish between the impact of the observed staffing increases and other characteristics of the VISNs. The leadership in each VISN that contributed to decisions about staffing increases could also have resulted in decisions about other actions that could have affected suicide rates. The estimate of staffing increases needed to achieve a 10% decrease in suicide rates is based on the assumption that changes in suicide rates are, in fact, attributable to changes in staffing, not to confounding factors. Moreover, the estimate is valid only to the extent that the underlying linear regression model is valid, and only for the average VISN with its population, medical and mental health services, and suicide prevention programs.
Conclusions
The conclusion must be that staffing increases, mental health enhancements, and suicide prevention activities in VHA facilities were effective where they were implemented most completely. Accordingly, current activities in VHA are focusing on decreasing the variability in implementation.
There have been a number of reviews of the effects of specific mental health treatments for suicide prevention (
17,
18), but few studies and reports have been published on the impact of modifications to mental health services that are provided to a defined population (
16). In this context, the findings presented here may be relevant beyond VHA. Although observations of the VHA system as a whole suggested that substantial enhancements to mental health services can occur without an impact on suicide rates, evaluations across VHA’s regional networks demonstrated significant associations. The implications for the field of suicide prevention must be that enhancements in mental health care can translate into decreased suicide rates.
Acknowledgments and disclosures
Support was provided by the Office of Mental Health Operations and the Office of Suicide Prevention of the VHA. Data for this report were acquired and analyses were conducted by the VHA for evaluation of its mental health and suicide prevention programs.
The authors report no competing interests.