When used in conjunction with outpatient mental health treatment and community supports, evidence-based medications can help individuals with schizophrenia and bipolar disorder live independently in the community. Treatment guidelines for schizophrenia recommend the continuous use of antipsychotics (
1), whereas treatment guidelines for bipolar disorder recommend the continuous use of antipsychotics, antidepressants, lithium, or certain anticonvulsants (
2,
3).
There is a considerable gap between the recommendations of clinical guidelines and actual practice (
4,
5). Individuals with schizophrenia and bipolar disorder frequently have gaps in medication use (
6,
7), which increases their risk of hospitalization, loss of employment, and disruptions in relationships (
8–
11).
Several factors may influence whether individuals fill their prescriptions. These include side effects common to antipsychotics and other psychiatric medications, such as weight gain, sexual dysfunction, and increased risk of metabolic syndrome (
12); poor therapeutic relationships with providers (
13,
14); and demographic characteristics, such as age and race (
4). Medication utilization management practices, including copayments, prior-authorization requirements, refill restrictions, or monthly supply limits, could present barriers to filling prescriptions. Some evidence suggests that Medicaid beneficiaries with schizophrenia are less likely to receive medications when they encounter copayments (
15). Surveys of individuals with schizophrenia have found worse medication adherence among those who perceive a greater copayment burden (
16).
One study of 30 states found that Medicaid programs that implemented prior-authorization polices experienced slower growth in spending for second-generation antipsychotics and no offset in the use of older antipsychotics, suggesting that prior authorization resulted in restricting access to antipsychotics (
17). Another study in Maine found that discontinuation of second-generation antipsychotics increased 29% after the implementation of prior-authorization requirements (
18). There is also some evidence that Medicaid beneficiaries with bipolar disorder are less likely to use medications when faced with prior-authorization requirements for second-generation antipsychotics (
19) or restrictions on the number of medications reimbursed per month (
20).
Much of the research that has used claims data to examine factors that may influence the continuous use of medications among people with schizophrenia or bipolar disorder has been conducted within a single state, has examined a single policy change, or has not been able to isolate the impact of individual medication utilization management policies or beneficiary characteristics (
21). There is a need for research among a diverse group of states that accounts for the range of utilization management practices and beneficiary characteristics that may influence medication continuity.
This study used Medicaid claims data from 22 states to answer two questions: First, to what extent are medication utilization management practices associated with medication continuity among Medicaid beneficiaries with schizophrenia and bipolar disorder? Second, is medication continuity associated with beneficiary characteristics, including race-ethnicity, gender, age, or geographic location?
Drawing on the research reviewed above, we hypothesized that medication continuity would be worse among beneficiaries who live in states that require higher copayments or prior authorization for medications and among those who are younger or in racial-ethnic minority groups (
4). These analyses were conducted as part of a project that investigated the delivery of evidence-based care among Medicaid beneficiaries with schizophrenia or bipolar disorder (
22).
Methods
Data
The study used Medicaid Analytic Extract (MAX) data from 2007. MAX data contain all Medicaid-funded medical and pharmacy claims for beneficiaries in every state and the District of Columbia. The data are created from eligibility and claims files submitted by states to the Centers for Medicare and Medicaid Services and include information on diagnoses and demographic characteristics (race, ethnicity, gender, age, and county of residence) for each beneficiary enrolled in Medicaid at any point during the year. Variables in MAX are standardized to create comparable measures of service use across states. Some states include encounters for Medicaid-funded services provided through managed care arrangements, including health maintenance organizations (HMOs) or behavioral health organizations in the MAX files; for other states, encounter data are incomplete or missing.
The analysis included beneficiaries diagnosed as having schizophrenia or bipolar disorder in states with complete and reliable fee-for-service claims or managed care encounter data. The study population was limited to adults ages 18–64 who had schizophrenia or bipolar disorder and who qualified for full Medicaid benefits on the basis of disability for at least ten months in 2007 and who had no other health insurance, including Medicare. Inclusion in the analysis required a primary diagnosis of schizophrenia or bipolar I disorder on at least one inpatient claim or two outpatient claims on different dates (
23,
24). Beneficiaries with a diagnosis of both bipolar disorder and schizophrenia were categorized according to the most frequent diagnosis during the year, with inpatient claims weighted more heavily than outpatient claims if we observed an equal number of claims for each diagnosis.
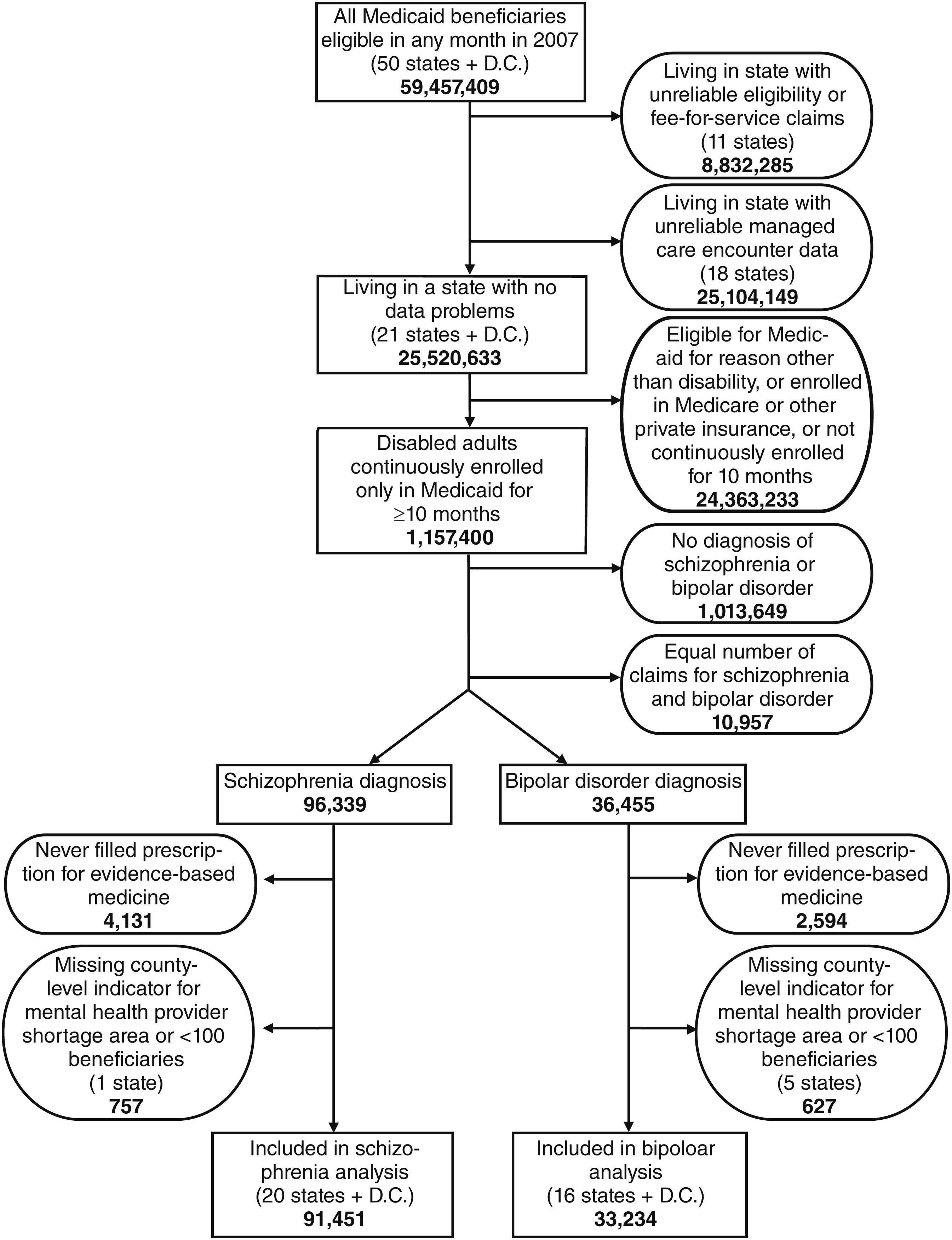
We systematically examined the completeness of data for all states to identify those appropriate for inclusion in the study. States with unreliable Medicaid eligibility data, fee-for-service claims, or managed care encounter data were excluded. In the remaining 22 states, approximately 11,000 beneficiaries were excluded because they had an equal number of claims for schizophrenia and bipolar disorder and therefore could not be assigned to either group, which limited the ability to assess their medication continuity because different medications can be used for these disorders. Finally, beneficiaries were excluded if the county-level indicator used to construct the variable for living in a mental health provider shortage area (described below) was missing or if there were fewer than 100 observations in the state; this resulted in the exclusion of one state for the schizophrenia cohort and five states for the bipolar disorder cohort.
Institutional review board approval was not required for this project. The data use agreement governed the security of the data and protected the confidentiality of beneficiaries.
Measures
Medication continuity was operationalized with a medication possession ratio (MPR). For schizophrenia, the MPR was calculated as the ratio of the days’ supply of all filled antipsychotic prescriptions (including all oral and depot or injection antipsychotics as defined by National Drug Codes on pharmacy claims and J codes on medical claims) to the number of days that passed from the initial antipsychotic prescription dispensing until the end of the calendar year (December 31, 2007) or until Medicaid disenrollment. Beneficiaries with schizophrenia were not required to remain on the same antipsychotic to be counted as receiving medication continuously. Prescription fills for different antipsychotics that covered the same period were considered a single prescription for purposes of counting the days’ supply of medication, unless the overlap was fewer than five days, in which case we assumed the beneficiary had filled the next month’s prescription early.
For bipolar disorder, the MPR was calculated in a similar fashion except that the numerator of the ratio included antipsychotics, lithium, and three anticonvulsants (carbamazepine, valproate, and lamotrigine). Beneficiaries with bipolar disorder were not required to remain on the same medication or medication class to be counted as receiving medication continuously. This strategy recognized that treatment of bipolar disorder may necessitate changing medication classes in response to changes in symptoms or functioning.
To aid in interpreting the MPR consistently with previous research, we created a dichotomous variable to differentiate beneficiaries with low and high medication continuity, with high medication continuity defined as an MPR of at least 80% (
6).
Information from the National Pharmaceutical Council was used to construct variables for state Medicaid medication utilization management practices (
25), which included prior-authorization requirements for antipsychotics, anticonvulsants, or antidepressants; monthly limits on quantity of medication that can be supplied (limit of ≤31 days versus >31 days); number of allowable refills without provider reauthorization (six or fewer versus more than six); and copayment requirements for branded and generic medications.
Information from the Health Resources and Services Administration was used to create a variable to indicate whether a beneficiary lived in a county designated as a mental health provider shortage area in 2007 (
26). A separate variable was created with data from the Area Resource File to designate whether the beneficiary lived in a metropolitan area (at least one urban cluster with a population of at least 50,000), micropolitan area (at least one urban cluster with a population of at least 10,000 but less than 50,000), or rural area (no urban cluster of at least 10,000) (
26).
Information from the Substance Abuse and Mental Health Services Administration (
27) was used to construct a variable that measured the proportion of state mental health agency funding directed to community-based services in 2007 with a 10-point scale corresponding to 0%−100% funding. This variable served as a weak proxy for states’ orientation to community-based versus institutional services, but it may not have accounted for county variation in funding for mental health services.
Finally, given that outpatient mental health services may encourage the use of medications, a variable was created to measure whether a beneficiary had at least one claim for outpatient mental health services during the year. Variables were also constructed to measure whether the beneficiary had a diagnosis or procedure code for diabetes, cardiovascular disease, or substance use disorder during the year. Individuals with these conditions, which are more common among this population than the general population (due, in part, to medication side effects and health risk behaviors), may experience overall health problems that could interfere with filling psychiatric medications. Conversely, those with comorbid conditions may be more likely to fill prescriptions as a result of more frequent contact with providers.
Analysis
Chi square analyses were conducted to examine bivariate relationships. Random-effects logistic regression analyses modeled the odds of high medication continuity. This regression technique accounted for the clustering of beneficiaries within each state to measure the extent to which residence in a state accounted for variation in the outcome beyond the medication utilization management practices and state characteristics that could be directly measured.
Given that different medications can be used for schizophrenia and bipolar disorder and, therefore, that the utilization management practices or other factors that could influence the use of these medications also may differ, we modeled the odds of high medication continuity by using separate cohorts of beneficiaries with schizophrenia or bipolar disorder.
The odds of high medication continuity among beneficiaries with schizophrenia were modeled as a function of residence in a state with a prior-authorization requirement for antipsychotics; generic medication copayments of $.50 to $1, $2, or $3 ($0 reference group); branded medication copayments of $1, $2, or $3 ($0 reference group); the percentage of state mental health agency funding directed toward community-based services; demographic characteristics that included beneficiary gender, age, race-ethnicity (African American, Latino or Hispanic, other or unknown, with non-Hispanic Caucasian as reference group), and residence in a mental health provider shortage area; HMO enrollment versus no managed care enrollment; the presence of a comorbid substance use disorder, cardiovascular disease, or diabetes; and the receipt of outpatient mental health services.
The odds of high medication continuity among beneficiaries with bipolar disorder were modeled as a function of the same covariates as used for the schizophrenia cohort with one exception—the regression included a variable for the number of prior-authorization policies for antipsychotic, antidepressant, and anticonvulsant medications in a state to avoid modeling each prior-authorization policy separately. Given the small number of beneficiaries in states with prior-authorization requirements for anticonvulsants, using a variable that counted the number of prior-authorization policies in the state increased statistical variation, resulting in a more stable coefficient. We also hypothesized that the number of prior-authorization requirements could inversely affect medication continuity for beneficiaries with bipolar disorder given their use of different classes of medications.
The regressions originally included variables for states’ limits on refills and monthly medication quantities, both of which were not statistically significant in the bivariate or multivariate analyses and were therefore excluded from the final regression models. To present parsimonious models, the final regressions did not account for residence in a metropolitan, micropolitan, or rural area because most beneficiaries lived in metropolitan areas such that medication continuity did not vary by these designations in bivariate or multivariate analyses.
Results
Study sample
The final sample included two cohorts: 91,451 beneficiaries in 20 states and the District of Columbia who had schizophrenia and had filled at least one prescription for an antipsychotic during the year and 33,234 beneficiaries in 16 states and the District of Columbia who had bipolar disorder and filled at least one prescription for an antipsychotic, lithium, or any of the three aforementioned anticonvulsants during the year (
Figure 1).
Beneficiaries were diverse in terms of age, race-ethnicity, and residence in a mental health provider shortage area (
Table 1). Beneficiaries resided in states that used different medication utilization management practices and varied in the proportion of state funding directed to community-based mental health care (
Table 2). State Medicaid programs differed in their required copayments for generic and branded medications. Roughly 20% of beneficiaries were enrolled in some type of managed care.
Sixty-four percent of beneficiaries with schizophrenia and 54% of beneficiaries with bipolar disorder had high medication continuity in 2007 (not shown in tables). The proportion with high medication continuity differed across states, as reported elsewhere (
22).
Factors associated with medication continuity
Residence in a state that required prior authorization for antipsychotics was associated with worse medication continuity among beneficiaries with schizophrenia, after other variables in the model were controlled for (
Table 3). Medication continuity was also worse among beneficiaries with bipolar disorder who lived in a state with a greater number of prior-authorization requirements for different classes of medications (p=.058).
Higher copayments were associated with worse medication continuity. For beneficiaries with schizophrenia, a $2 or $3 copayment for generic medications was inversely associated with medication continuity. A $1 copayment for branded medications was inversely associated with medication continuity for both beneficiaries with schizophrenia or bipolar disorder. HMO enrollment was inversely associated with medication continuity.
Older age was associated with slightly better medication continuity. Beneficiaries who were African American or Latino or Hispanic had worse medication continuity compared with non-Hispanic Caucasian beneficiaries, as did beneficiaries of other or unknown race-ethnicity with schizophrenia. The presence of a substance use disorder or cardiovascular disease was inversely associated with medication continuity, whereas the presence of diabetes was associated with better medication continuity. For beneficiaries with schizophrenia, medication continuity was also worse among those in a mental health provider shortage area. Finally, medication continuity was slightly better among beneficiaries who had at least one outpatient mental health visit, and for those with schizophrenia, continuity was better among those who lived in a state where a higher proportion of state mental health funding was used for community-based services.
Discussion
This study identified several factors associated with medication continuity among Medicaid beneficiaries with schizophrenia and bipolar disorder. Higher medication copayments, prior-authorization requirements, HMO enrollment, and other state and demographic characteristics were inversely associated with medication continuity. The use of person-level Medicaid claims data from a diverse group of states and the analysis of several medication utilization management practices while accounting for other state and beneficiary characteristics expanded on previous literature to identify the relative contributions of these factors.
The inverse relationship between prior-authorization requirements and medication continuity is consistent with previous studies that have used different data sources or that have been limited to a smaller number of states (
17–
19); it is notable that these studies arrived at similar conclusions despite using different methods and data. Taken together, the findings from these studies present compelling evidence that prior-authorization requirements may adversely affect the ability of this population to maintain use of medications. Although we did not examine the outcomes of poor medication continuity in this study, other studies have suggested that prior authorization and other medication utilization management practices may fail to achieve cost savings in this population as a result of increased hospitalizations (
17,
20).
Although higher copayment requirements for generic medications were inversely associated with medication continuity for schizophrenia, the absence of a linear relationship between copayment amounts for branded medications and medication continuity is notable. There are several possible explanations for this finding. The implementation and enforcement of medication utilization management practices in Medicaid programs is often nuanced and may exclude certain medications or classes of medications from copayment requirements (such details were not available for this study). Thus it may be that some states with higher copayments for branded medications excluded certain psychotropic medications from copayment requirements such that there was insufficient variation to detect a relationship. Alternatively, given that this study could not directly measure every feature of states’ mental health systems or Medicaid programs, it is possible that the variable for branded medication copayments functioned as a proxy for some other state characteristic. Future studies should build on this work to account for other state characteristics that may explain the lack of a linear relationship. Although a cross-sectional analysis of claims data cannot fully describe the complex and dynamic relationship between copayment amounts and medication continuity, these findings are intended to provide a foundation for further inquiry and are largely consistent with previous work (
16).
Beneficiaries who lived in states where a higher proportion of state mental health agency funding was directed to community-based services or who were not in a mental health provider shortage area had better medication continuity. Medication continuity was also better among those who had at least one outpatient mental health visit. Although these findings seem reasonable given that the use of outpatient care may encourage the use of medications, these findings should be interpreted with caution because this study used crude measures for these variables. These measures may not reflect county variation for mental health care. In addition, this study did not measure the number of outpatient mental health visits because the data lacked sufficient detail to make reliable cross-state comparisons in outpatient mental health care (
22).
Several demographic characteristics were associated with medication continuity. Consistent with previous research, younger beneficiaries had worse medication continuity (
4). The symptoms and impairment associated with schizophrenia and bipolar disorder often begin during young adulthood—a period characterized by diagnostic instability, changing treatment plans, and substantial life changes. The findings underscore the need to help youths stabilize and maintain their medication regimens to prevent disruptions in their educational and employment trajectories. Also consistent with previous research, African Americans had worse medication continuity than Caucasians (
4). Finally, beneficiaries with a diagnosis of a substance use disorder or cardiovascular disease had worse medication continuity, and those with diabetes had better continuity. Beneficiaries with diabetes may have more regular contact with providers and therefore more opportunities for medication monitoring; perhaps their diabetes also accustoms them to maintenance of regular routines that facilitate steady medication usage. Alternatively, those with high medication continuity may be more prone to developing diabetes as a result of medication side effects (
28). This study could not determine the direction of the relationship between comorbid conditions and medication continuity because there was only a single year of data. In addition, because comorbid conditions are often not diagnosed or treated in this population, the findings may understate the true relationship between comorbid conditions and medication continuity.
The findings should be interpreted within the context of several other limitations. As mentioned, reliable measures were not publicly available for many features of state Medicaid programs or mental health systems. Readers should interpret the findings with caution given the small number of states in this study that employed restrictive medication utilization management practices or had managed care arrangements. The use of claims data alone does not allow for the measurement of all beneficiary characteristics that could influence medication continuity, which may include family support and connections with providers (
11,
14). Individuals who were dually eligible for Medicaid and Medicare were excluded because Medicare Part D claims were not available and because this study was focused on Medicaid policies and payment practices. It is possible that dually eligible beneficiaries differ from Medicaid-only beneficiaries in the duration and severity of their illness. Finally, future studies should account for medication burden—or the total number of medications prescribed for an individual—because some studies have shown that greater medication burden is associated with better medication adherence (
29).
Conclusions
As state Medicaid programs refine their benefits packages in the context of continuing budget pressures and federal and state health care reforms, they may wish to consider the consequences of imposing certain medication utilization management practices on beneficiaries with serious and persistent mental illnesses. The findings from this study suggest that exempting this population from prior-authorization requirements and copayments for medications may improve medication continuity. Further work is needed to identify other policies and factors that could improve medication continuity in this population.
Acknowledgments and disclosures
The authors conducted this work under contract HHSP23320095642WC/HHSP23337012T with the Office of the Assistant Secretary for Planning and Evaluation (ASPE), U.S. Department of Health and Human Services (DHHS). The authors appreciate the guidance of Richard Frank, Ph.D., John Drabek, Kirsten Beronio, Frank Yoon, Ph.D., Crystal Blyler, Ph.D., and their technical advisory panel. The views and opinions expressed in this article are those of the authors and do not necessarily reflect the views, opinions, or policies of ASPE or DHHS.
The authors report no competing interests.