Restraint has been defined as “any manual method or physical or mechanical device, material or equipment that immobilizes or reduces the ability of a person to move his or her arms, legs, body or head freely,” whereas seclusion is “the involuntary confinement of a person alone in a locked room or an area where the person is physically prevented from leaving” (
1). Although the use of seclusion or restraint may minimize harm in psychiatric emergencies, the risks and costs of these procedures to both patients and staff have resulted in several national and international recommendations to restrict their use (
2–
5). In theory, seclusion-restraint could be discontinued by decree, if patient violence is not a consideration.
According to the literature, the highest seclusion-restraint reduction rates have been achieved by simultaneously improving several elements of care to prevent crises that lead to seclusion or restraint. Such elements include improved leadership, staff development, use of data, consumer involvement, use of seclusion-restraint reduction tools, and postevent analyses (
6–
10). Decreases in seclusion-restraint rates have ranged from 47% to 92% in 70 U.S. institutions that applied these six core strategies under the State Mental Health Authority (
10–
15). Violence considerably decreased in some of these units but increased in others that were mandated to reduce coercion (
10,
16).
So far, published seclusion-restraint prevention interventions have not reported statistical comparisons on quantitative changes between the use of seclusion-restraint and incidence of violence after objectively comparing stratified intervention units and control units for persons with severe psychotic disorders (
17). Without such a direct comparison, both the safety of the intervention and the size of its effect remain unclear, because other factors could also coincidentally influence seclusion-restraint reduction and violence, including new regulations, seasonal variation (
18), pharmacological practices (
12), and patient selection. Controlled data on the safety and effectiveness of seclusion-restraint reduction strategies are needed for an estimation of the possible benefits and risks of new interventions. For this reason, our aim was to study the feasibility of preventing coercive measures without violence in a cluster-randomized controlled study of high-security wards for males with schizophrenia in Finland.
Methods
Participants and settings
In Finland, two state-run secured hospitals are the last resorts for the criminal and civil patients with psychotic disorders and violent behavioral problems. About two-thirds of these patients are in the Niuvanniemi Hospital in Kuopio. In 2009 the hospital served 300 adult inpatients—164 forensically involved patients (55%) and 136 additional patients—in 13 wards. About 86% of the inpatients were men, 97% of whom had schizophrenia spectrum disorder or a delusional disorder. The patients having the highest risk for violence and seclusion were admitted to the high-security wards that had the highest staff-to-patient ratios. Practically all patients used second-generation antipsychotics—primarily clozapine—and many received antiepileptics and mood stabilizers as adjuvants. The pharmacological practices did not change during the project. [Medications received in 2006–2009 are listed online as a
data supplement to this article.] Seclusion was the primary coercive method. Mechanical restraints and injections were rarely used, and physical restraints were used only briefly to transfer a patient to a seclusion room.
Before the information year, the need for coercion reduction was quite unknown among the hospital staff (N=804), despite the high seclusion-restraint rates. Two intervention wards and two control wards served the most treatment-resistant men with schizophrenia in Finland (N=88 beds). The utilization rate of the beds was 95%−98%. The same senior psychiatrist, not involved in the study, made the psychopharmacological decisions in both ward groups.
Eligibility criteria
The study was designed according to the Consolidated Standards of Reporting Randomized Trials and its extension to cluster-randomized trials (
19) (
www.consort-statement.org/extensions/designs/cluster-trials). Allocation of the participants was based on treatment ward (place-based allocation). [A CONSORT flow diagram is available online in the
data supplement to this article.] Of the 13 wards for adults at the Niuvanniemi Hospital, four of the wards for males used seclusion and restraint. To avoid the possibility of unbalanced comparisons (for example, two wards with a high level of seclusion-restraint versus two wards with a low level of seclusion-restraint), intervention and control ward groups were stratified by use of seclusion-restraint (
www.randomization.com). New patients were assigned to the wards by physicians who were not involved in the study, according to the normal practice of the hospital. The protocol was not changed during the study.
Funding, curriculum, and resources
This trial was part of a Niuvanniemi Hospital performance improvement project during 2008–2009. It was funded by the National Institutes of Health and Welfare as a part of research funding for state hospitals in Finland. The ward system study from the project was registered and accepted by the ethical committee of the Kuopio University Hospital District. Because the effect of the intervention was studied via examination of the hospital registers, informed consent of the patients was not required. The curriculum was based on the 2003 training curriculum of the National Executive Training Institute (
20) and the National Association of Mental Health Program Directors (
21) and on a publication from a collaboration of the American Psychiatric Association and other mental health organizations (
9). The task force for this trial was not involved in the ward organization and did not participate in the care of the patients. It consisted of a master’s-level senior nurse, a doctoral-level cultural anthropologist–psychotherapist-counselor, and a doctoral-level researcher who was a forensic psychiatrist. They studied the data from hospital registers, planned the project, tailored the crisis prevention tools (
22,
23), and both educated and helped the wards to use the core strategies of seclusion-restraint reduction. The increase of resources during the study period amounted to two person-years per year.
Information year
As of January 2008, all wards in the hospital were informed of the project and the need to reduce the use of seclusion and restraint. The team visited five state hospitals in Pennsylvania and Florida to see the implemented intervention strategies in practice settings. The team reported its observations to the leaders of the hospital who worked in the steering group. Together, in two general information meetings, they informed the staff of the need to reduce the use of seclusion and restraint. The allotted intervention wards were declared in October 2008.
Intervention
Between January and June 2009 the researchers assisted staff of the intervention wards to initiate the new practices, and they assisted again between July and December to maintain the intervention. The leaders of the intervention wards were supported with individual and group counseling (one hour per week) and in daily postevent analyses with the senior nurse or counselor (30 minutes per day). Staff critically reviewed problems, rules, and practices and received information on the risks and traumas associated with seclusion-restraint, the prevention of crises, and the new tools (one hour per week). The cultural anthropologist–psychotherapist-counselor used participation-observation methods to help the counseling processes and helped the wards to develop individual preventive strategies and alternatives to seclusion (one hour per week).
The service users educated the project workers in consumer specialist meetings (one hour per week) about their own experiences with violence and coercion, individual triggers of violence, and effective calming activities. They also suggested new ways and practices to decrease fear, violence, and coercion and brainstormed with staff and doctors about the ward rules and practices during weekly community meetings (45 minutes). According to the patients’ request for activities, some patients and staff volunteered to work together one hour per week on building projects in the courtyard. Because many patients and staff found it difficult to discuss their experiences of coercion and violence, they wrote, photographed, and illustrated a book together, titled
Behind Locked Doors (
24).
Statistics on coercion and violence were used to guide the practices in many ways. Intervention wards used a progress sheet to record and track daily the number of seclusion-restraint incidents observed, and staff discussed the monthly figures with the senior nurse (30 minutes per month). The statistics were also discussed in the monthly steering group and at two general information meetings. Individual graphics of violence and seclusion were used in counseling and crisis planning.
Crisis prevention tools were tailored with input from staff and patients (
22,
23) to aid in individual crisis prevention, deescalation of tense situations, and coping with crises. The tools included a questionnaire of traumatic experiences and violent behavior and a list of common triggers, warning signs, calming activities, and daily activities. The individual crisis plan, which was an agreement on the calming activities to be used if the warning signs of violence appeared, was revised and developed after each crisis (
22,
23).
Each morning the project senior nurse and cultural anthropologist–psychotherapist-counselor discussed with staff the violent incidents that occurred and reported on the practices, restrictions, and alternative methods used, according to the postevent analysis sheet. These meetings identified and praised successful interventions and otherwise helped the staff to improve their practices.
Measurement
The monthly duration of seclusion-restraint and the number of patient-days with seclusion, restraint, or room observation were collected for both groups from computerized hospital registers. The details of physical violence against persons were obtained from computerized and modified staff observations of aggression scales, some additional items used at the hospital since the 1990s, and from the yearly workforce surveys. The data were verified from other registers.
Outcome measures
Effect of the intervention.
The monthly incidence rate ratios (IRRs) between the intervention and control wards during the stabilized intervention (between July and December 2009) consisted of the following three parameters, all divided into 100 patient-days: seclusion, restraints, or room observation days (the number of patient-days when any seclusion-restraint or room observation was used); seclusion-restraint time (the patient-hours spent in seclusion or restraint); and violence (the number of incidents of physical violence against any person, including self-harm). In addition, the number of injuries to patients and staff during the intervention year was compared with data for the previous year.
Effect of the project on the hospital.
To illustrate the facilitywide benefits and harms of the project, the IRRs of the monthly seclusion-restraint times (per 100 patient-days) for the entire hospital during the information year and the intervention year were compared with those of the two preceding years, with year 2007 as a reference. The reasons for and length of staff sick-leave time and injuries to both patients and staff were also considered.
Statistical methods
Incidence rates with 95% confidence intervals (CIs) were calculated by assuming a Poisson distribution. IRR estimates were calculated by using a Poisson regression model or negative binomial regression model when appropriate.
Results
Sample characteristics
The four high-security wards participating in this ward system study were the last resorts for men with psychotic illness and a history of severe violence in Finland. During the intervention year, the two intervention wards accounted for 1,306–1,400 patient-days per month, with 50 beds (24 and 26 beds). The two control wards accounted for 930–1,003 patient-days per month, with 38 beds (17 and 21 beds). Overall, 95%–98% of the beds were occupied. With the exception of a small number of Asians, the clients were Finnish-speaking Caucasians. The mean±SD age of the patients was 40.2±10.6 in the intervention cluster and 38.4±10.6 years in the control cluster.
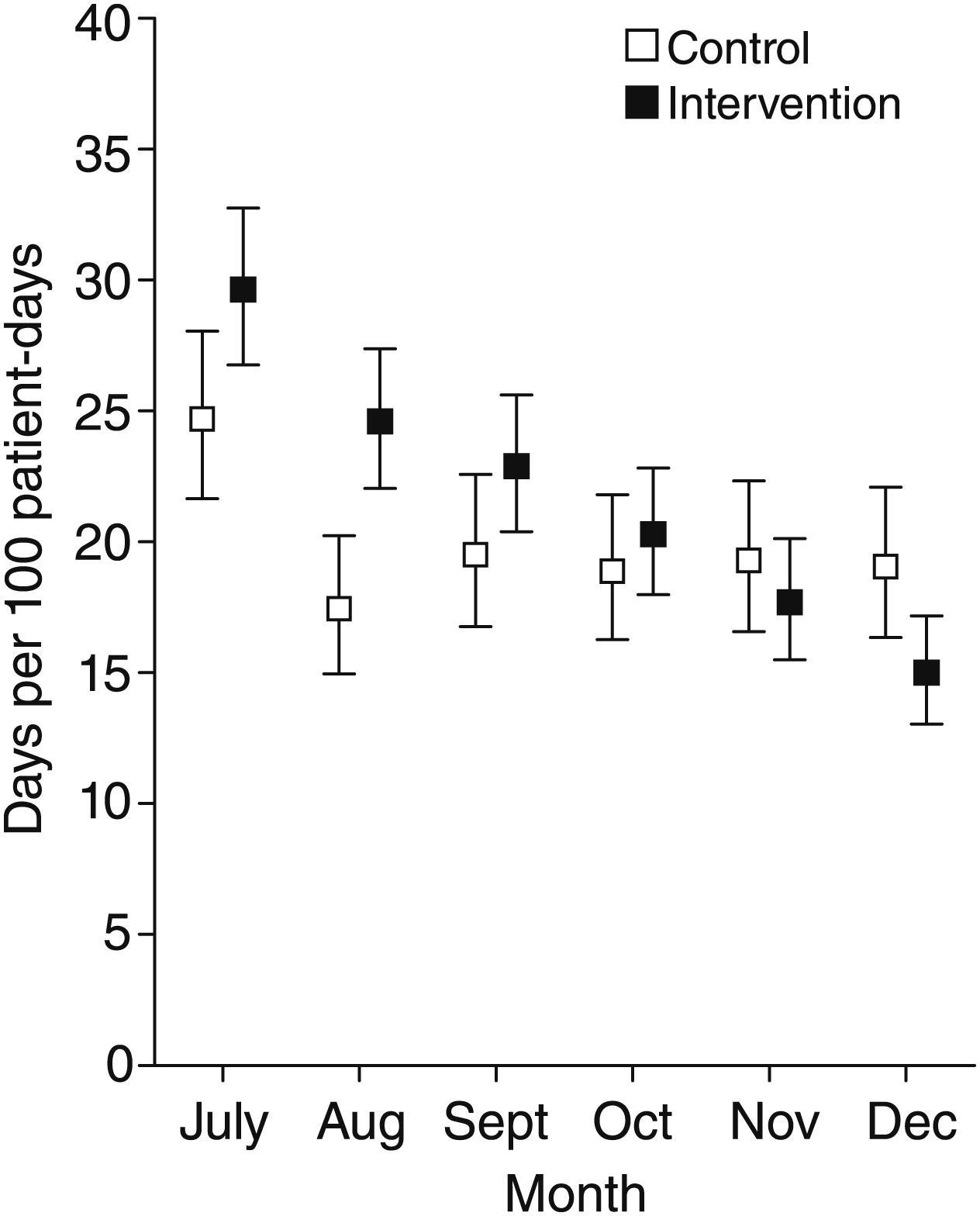
The effect of the intervention
Seclusion-restraint and observation days decreased during the supported intervention from 30% to 15% of the total patient time for intervention wards (IRR over time=.88, CI=.86–.90, p<.001) versus a decrease from 25% to 19% for control wards (IRR=.97, CI=.93–1.01, p=.056). The difference between the groups was significant (p=.001), despite the significantly lower rate in December than in July for both intervention wards (IRR=.51, CI=.43–.60, p<.001) and control wards (IRR=.77, CI= .63–.94, p=.009) (
Figure 1). [Details of recorded seclusion-restraint days and time and violence incidence are available online in the
data supplement.]
Seclusion-restraint time decreased from 110 to 56 hours per 100 patient-days for intervention wards (IRR over time=.85, CI=.78–.92, p<.001), yet increased from 133 to 150 hours for control wards (IRR=1.09, CI=.94–1.25, p=.24). The difference between the groups was significant (p=.001). The difference between July and December was significant for intervention wards (IRR=1.14, CI=1.05–1.23, p=.001) and for control wards (IRR=.77, CI=.63–.94, p<.001) (
Figure 2).
Violence decreased for both groups, from 1.1% to .4% of patient-days for intervention wards (IRR over time=.92, CI=.79–1.05, p=.23) versus from .1% to <.01% for the control wards (IRR=.90, CI=.64–1.23, p=.51) (
Figure 3). The difference between intervention and control wards was not statistically significant (p=.91). The severity of violence diminished in the intervention wards. Patient-to-patient violence or self-harm resulted in a broken bone for one patient during the intervention year (versus one suicide and one restraint death before the intervention in 2008). For the control wards patient injuries remained minor, consisting of superficial wounds. The consequences of patient-to-staff violence remained minor for both groups and consisted of superficial wounds and bruises.
Effect of the project on the hospital
Monthly seclusion-restraint time had increased before the project (2006–2007) but declined during both project years (
Figure 4). The IRR for annual seclusion-restraint time, compared with 2007, was .75 (CI=.73–.78) in 2008 and .49 (CI=.47–.51) in 2009.
More reports of patient-to-staff violence were recorded at the entire hospital: 18 reports during the information year (2008) and 22 reports during the intervention year (2009), compared with 13 reports before the project (2007). However, patient-associated injuries to staff resulted in 75% and 65% fewer sick days, respectively, during the information and intervention years, compared with the year before the project (29 days in 2008 and 40 days in 2009, versus 114 days in 2007). The mean duration of a sick leave resulting from patients was 80%−82% shorter during the project (1.6 days per injury for 2008 and 1.8 days per injury for 2009, versus 8.8 days per injury in 2007). The only patient-to-staff injury at the hospital occurred on a nonproject ward and resulted in a mild contusion.
Surprisingly, monthly staff physical violence management training with colleagues resulted in a three- to fourfold higher number of sick days compared with sick days resulting from patient violence (89 sick days from staff training versus 29 days from patient-related incidents for 2008, and 165 sick days from colleague-related incidents versus 40 days from patient-related incidents for 2009). Compared with patient-to-staff injuries, these staff-to-staff injuries also resulted in longer sick leaves: mean 6.4 days per injury from colleagues versus 1.6 days per injury from patients for 2008 and 12.7 days per injury from colleagues versus 1.8 days per injury from patients in 2009.
Discussion
This cluster-randomized controlled trial has demonstrated that in providing care for patients with schizophrenia and a history of violent behavior, it is possible to prevent the use of coercive measures without an increase in violence. Both the proportion of patient-days when any coercion was used and the time spent in seclusion-restraint decreased significantly more in the intervention wards than in the control wards, without an increase in violence. Contrary to fears and expectations that had sustained the coercive culture, the severity of patient-to-patient injuries (including self-mutilation) did not increase, and in fact severity decreased in the intervention wards. Injuries to staff remained minor.
In this study it was not possible to completely isolate intervention and control wards. The general distribution of information for the project possibly contributed to a collateral reduction of coercion rates in the control wards by “washing out” the effect of unawareness of the need to reduce seclusion-restraint practices. All wards were informed of the study and were considered eventual candidates for the intervention. The leaders of the hospital worked as a steering group; some nurses worked on many wards, and the intervention was discussed openly. Therefore, the study may have underestimated the effect size of the intervention. Also, awareness of the observation could have increased the seclusion-restraint reduction seen in both groups. This effect was, however, controlled by the control-group design of the study.
Throughout the hospital, a strong, time-specific effect of the project on seclusion-restraint rates and staff sick time was noticed during information and intervention years. The overall proportion of seclusion-restraint and observation days decreased steadily after the initiation of the project, and the annual rate of seclusion-restraint time was finally less than half the rate of the preceding year. Perhaps better coverage through the reporting of minor violence during the project—because of daily postevent analyses in the intervention wards, for example—increased the reports of minor patient-to-staff injuries at the hospital, because the yearly staff sick time associated with patient-to-staff injuries was 70% lower during the project years than before it. Presumably these injuries were also less traumatic given that the mean length of a sick leave episode was 81% shorter than before. This association between seclusion-restraint reduction with decreased sick time is in line with some previous reports of the six core strategies (
10,
25). Surprisingly, during our two project years physical violence management training sessions between coworkers resulted in a three- to fourfold number of sick days and a four- to sevenfold increase in sick time per injury compared with sick leaves resulting from patient-to-staff violence. These results suggest that all coercive contacts and even training may be dangerous and should be taken into account in the preventive efforts.
It has been considered important to conduct randomized controlled trials of seclusion-restraint reduction strategies but difficult to find psychiatric units that are homogeneous enough to allow for such a controlled trial (
6). In this study, the difference across clusters was minimized by stratification of the wards into similar groups by seclusion-restraint rates and by including only the wards that had admitted the most violent males with schizophrenia in Finland. Seclusion-restraint was not replaced by other coercive methods or new pharmacological practices, and the problem of various definitions of a seclusion-restraint episode was controlled by calculating the proportion of patient-days a patient was exposed for any duration of coercion. The patients admitted to the high-security wards had more severe problems than the discharged ones, and the most violent patients remained at the study wards.
A reduction in seclusion-restraint rates can be achieved by various methods. Randomized controlled studies of short-term risk assessments in acute psychiatric wards have also decreased coercion rates (
26,
27). Given that only a third of seclusion-restraint episodes in Finland are associated with violence (
28), the simultaneous use of several seclusion-restraint reduction strategies to improve the ward culture was likely to also improve the effectiveness of our intervention in the high-security units. One year is too brief a time for a fundamental cultural change in this environment. However, this study also seemed to increase empowerment and communication among the subcultures of patients, nurses, and doctors.
Conclusions
This study provides the first randomized controlled evidence for the ability to reduce the use of seclusion-restraint without a concomitant increase in violence in the care of persons who have schizophrenia and a history of violent behavior. A similar reduction may also be feasible under less extreme circumstances.
Acknowledgments and disclosures
This project was funded by the Finnish Ministry of Health through the developmental fund for Niuvanniemi Hospital. This study would not have been possible without the help and information from Dr. Kevin A. Huckshorn, Dr. Janice Lebel, and the leaders and staff of the state hospitals in Pennsylvania and South Florida.
Dr. Tiihonen is a member of the AstraZeneca and Janssen-Cilag advisory boards. He also reports serving as a consultant for or receiving fees for expert opinions or lectures from AstraZeneca, Bristol-Myers Squibb, Eli Lilly, F. Hoffman–La Roche, GlaxoSmithKline, Janssen-Cilag, Lundbeck, Novartis, Organon, and Pfizer. The other authors report no competing interests.