In the past 25 years, consumer-operated service programs (COSPs) for persons with severe mental illness have greatly increased, become a major component of the mental health system, and been recognized as effective in fostering recovery (
1). These organizations have key common ingredients of program structure, including consumer involvement in hiring decisions, governance, and budget control (
2), consumer control in determining policies and procedures, and a nonhierarchical program structure (
3).
Consumer-run organizations, however, have encountered challenges in adhering to nonhierarchical structures. The literature distinguishes two types of such organizations on the basis of governance structures: the participatory-democracy self-help agency (SHA)—a participatory democracy in which members can help make significant organizational decisions—and the board- and staff-run COSP (BSR-COSP)—in which member decision making is confined to program content (
4–
7). Although the latter may provide services more efficiently, the former is structured to allow members wider decision-making opportunities (
7). Independent work has empirically validated differences in the program environments of these two organizational types (
8). SHAs allow members a voice in major organizational decisions through participatory processes such as community meetings. BSR-COSPs do not. Both types have a director who is a consumer, at least 50% consumer representation on the board of directors, and consumer authority to hire and fire professionals employed within the organization (
9). In the BSR-COSP, this authority resides in hierarchically structured consumer leadership rather than in collective decision-making processes.
Recent research has indicated that the SHA seems to offer significant advantages in promoting recovery (
10) and that BSR-COSP participants may be at a significant disadvantage in their recovery efforts (
11). This study attempted to understand reasons underlying these differences.
Cooley (
12), in his exploration of the “looking-glass self,” surmised that we learn to understand who we are by incorporating what we perceive to be how others see us. Thus, if individuals hold negative attitudes toward people with mental illness, such attitudes are likely to affect how people with mental illness see themselves. Much work has focused on self-stigma, but few studies have considered how behavioral interactions might change attitudes (
13–
15). Cooley’s insight is related to the importance of behavioral interactions in influencing self-perception. COSPs counter stigma by demonstrating behaviorally (as opposed to offering testaments) that people with a history of mental health issues are capable of running a complex organization. Consumers engage in responsible actions that have a direct impact on their view of self and others. This engagement presumably can help them “recover” from stigmatization. However, organizations whose structure implicitly suggests that members lack certain capabilities may engender members’ negative attitudes toward self and others—in effect, promoting self-stigma.
Although enthusiasm for consumer-operated service organizations is widespread, few have been evaluated with methods used in controlled trials (
16–
18). One such trial has demonstrated the effectiveness of SHAs working in concert with community mental health agencies (CMHAs) to promote recovery objectives (
10). A second trial found that BSR-COSPs working in concert with CMHAs produced negative recovery outcomes (
11). The study presented here considered the relative effectiveness of SHAs and BSR-COSPs in working with CMHAs to address stigmatizing attitudes. Such self-stigma may impede provision of peer support, a significant self-help component (
19).
Methods
Settings and participants
The study involved a two-group randomized controlled trial, first conducted with five SHA-CMHA pairs of service providers (
10) and then with one BSR-COSP–CMHA pair (
11). Each agency pair served a single geographic area. The consumer programs were drop-in centers that offered peer-support groups, material resources, socialization, and direct services, such as money management, counseling, and provision of information or referral. Programs were open approximately eight hours a day for six days a week. Average daily attendance was 20 to 50 members. Only in SHAs could members take part in major organizational decisions related to budget and personnel. In the BSR-COSP, only staff, administrators, and the organization’s governing board could decide such issues. A consumer served as the director of each SHA or BSR-COSP, and most members of the governing board were consumers. A high degree of staff control distinguished the BSR-COSP from the five SHAs (
8). The BSR-COSP was a clearly top-down organization with a dominant leader; all major decision making was confined to the board and staff, with community meeting decisions restricted to activity planning. Two SHAs had mixed organizational characteristics: they had strong leadership and organization, but they made significant attempts to involve members in major decisions at community meetings. Two other SHAs practiced power sharing by delegating major decision making to members at community meetings.
The CMHAs were county mental health organizations providing outpatient services, including assessment, medication review, individual and group therapy, case management, and referral.
Study design
Between 1996 and 2001, new CMHA clients accepted for service under California medical necessity criteria were invited to enroll in the studies (
10,
11). Clients were randomly assigned (at a ratio of approximately one to four in the SHA trial and a ratio of two to three in the BSR-COSP trial) to continued CMHA treatment or combined services—that is, to a provider at a CMHA clinic plus attendance at a consumer-operated program or simply to a provider at a CMHA clinic. Thus one group in each trial received combined CMHA and either SHA or BSR-COSP services. Institutional review board approval was obtained, and participants provided informed consent.
Interviews were conducted by former mental health clients and professionals. During interviews with each client, demographic information was gathered, and the Diagnostic Interview Schedule for the DSM-IV (
20) was used to assign a diagnosis. Multiple outcome measures were pretested in a sample of 310 long-term users of SHAs in northern California (
21) and with CMHA clients. These measures were employed at baseline and in a follow-up interview at eight months.
Measurement
Self-stigma was assessed by participants’ expressed attitudes toward people with mental illness on the Attitudes Toward Persons With Mental Illness Scale (ATPMIS) (Segal SP, unpublished manuscript, 2013). A factor-analytic study of the ATPMIS indicated that it measures three dimensions of stigma: rejection based on perceived increasing threat posed by more intimate contact, rejection based on perceived lack of competence and trustworthiness, and rejection based on severity of illness indicated by having been hospitalized. The ATPMIS has 18 items, which have been used in many studies of expression of stigmatizing attitudes (
22). Each item is scored from 1, strongly agree, to 6, strongly disagree. The total possible score is 108, with lower scores indicating more acceptance and positive attitudes. Mean substitution is used for missing values when a minimum of nine items are answered. The ATPMIS reliability (Cronbach’s alpha) at the SHA-CMHA trial baseline was .87, and at follow-up it was .88. At both baseline and follow-up of the BSR-COSP–CMHA trial, it was .98. [More information about the ATPMIS is included in an online
data supplement to this article.]
The Organizationally Mediated Empowerment Scale (OMES) assesses the extent to which members are empowered by organizational participation (
23). The 17-item OMES presents yes-no questions, such as “At [your center] have you taken part in deciding what rules people need to follow?” “At [your center] have you taken part in deciding how much money should be spent on a service or program?” The OMES reliability (Cronbach’s alpha) is between .87 and .90, and the stability coefficient is .62. The OMES has convergent and discriminant construct validity, clustering with extraorganizational empowerment (out-of-organization decision activity and action) and distinguishing itself from self-efficacy and social functioning measures (
24). In this study, OMES reliability (Cronbach’s alpha) at baseline and follow-up was .86 and .80, respectively, with a stability coefficient of .56.
The Self-Efficacy Scale (SES) (
25) measures self-confidence in one’s ability to effect certain actions. It conceptually bridges two dimensions of the empowerment construct—control over personal life and material situation and control and influence over others within and outside the organization (
24). This bridging characteristic links the individual’s confidence in his or her ability to be efficacious in common life activities with his or her sociopolitical or group actions. The SES has a reliability (Cronbach’s alpha) of between .89 and .92, and a stability coefficient of .62 (
24). In this study, SES reliability at baseline and follow-up were .88 and .92, respectively.
Analyses
Analyses were completed with SPSS, version 20. Frequencies and means were computed for descriptive characteristics. Differences between samples were evaluated with chi square tests and analyses of variance; significance tests were two-tailed. Individuals attend consumer-operated programs with varying degrees of commitment. Some drop in for coffee, and others engage in services to help them secure stable housing and employment, for example. Early work has emphasized the positive experience of long-term users (
21). To account for this, the samples were weighted by the inverse of the probability of clients’ reaching eight months of service in the assigned condition.
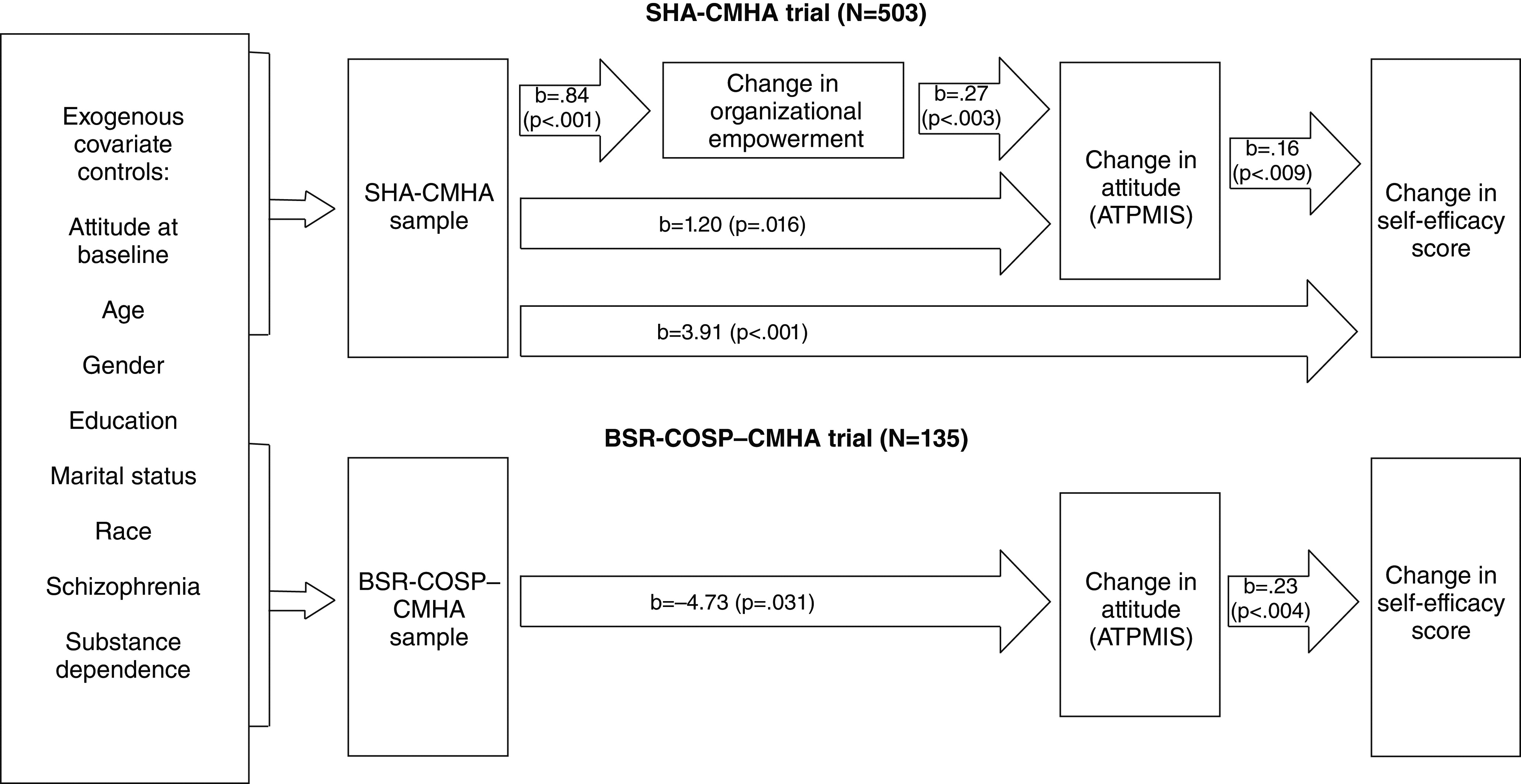
This study sought to determine the effect of service condition and organizational empowerment on change in self-stigma (measured with ATPMIS) and the possible impact of such a change on recovery potential (measured with SES) over an eight-month period, after controlling for differences associated with possible poor randomization or dropout before final assessment. It did so by using SPSS’s multivariate ordinary least-squares regression program to evaluate a fully recursive path model with four endogenous variables—change in SES, change in ATPMIS, change in OMES, and service condition—and seven exogenous covariate controls. Higher SES change scores (eight months minus baseline), ATPMIS change scores (baseline minus eight months), and OMES change scores (eight months minus baseline) indicated a positive change. Service condition was coded 1 or 0 for combined services versus CMHA only. Exogenous covariate controls included the demographic and disability characteristics of age, gender, race (African American versus other), education (less than high school, high school graduate, or postsecondary education), marital status (never married versus other), mental illness diagnosis (schizophrenia versus other), and substance dependence (yes versus no).
Results
Of the 1,042 individuals asked at baseline in the SHA-CMHA versus CMHA-only trial, 896 (86%) agreed to enroll. Of the enrolled, 56% (N=505) received services for at least eight months, including 51% (N=403) of the SHA-CMHA sample and 46% (N=102) of the CMHA-only sample. Of the 189 individuals asked at baseline in the BSR-COSP–CMHA versus CMHA-only trial sample, 162 (86%) agreed to enroll. Of the enrolled, 139 (86%) received services for at least eight months, including 86 (86%) in the BSR-COSP–CMHA sample and 53 (85%) in the CMHA-only sample. No CMHA-only participant in either trial self-referred to the consumer-run program during the study. In the SHA-CMHA trial, the mean±SD number of visits per month was 6.50±9.34 to the SHA (median=2; mode=2) and 3.21±2.72 to the CMHA (median=2; mode=1). The mean number of visits per month in the BSR-COSP trial was 4.24±.43 to the BSR-COSP (median=4; mode=4) and 2.1±1.7 to the CMHA (median=1; mode=1). Demographic and diagnostic information is reported in
Table 1.
The mean item score at baseline on ATPMIS items was 2.96 for participants in the SHA-CMHA trial and 2.49 for those in the BSR-COSP–CMHA trial. [A table in the online
data supplement presents responses to five ATPMIS items of the two samples in this study, with comparisons to responses from a previous study (
26). ATPMIS responses indicated that compared with the general population, people with mental illness had more positive attitudes toward others with similar disabilities; in addition, attitudes of the people with mental illness were more positive in the study reported here than in the past study.]
As shown in
Table 2, participants in the two trials did not differ on baseline OMES and ATPMIS scores. However, in the SHA-CMHA sample, OMES and ATPMIS scores at eight months differed significantly from baseline. Such differences were not found for BSR-COSP participants. In the SHA-CMHA trial, the significant baseline difference in SES scores between SHA-CMHA and CMHA-only participants (favoring the latter group) disappeared by eight months. In the BSR-COSP trial, an increasing though nonsignificant difference in SES scores developed over the eight months between the BSR-COSP–CMHA participants and the CMHA-only participants, with the former group’s scores trending down.
Correlations between ATPMIS change scores and the number of visits to the respective consumer-operated service indicated that increased BSR-COSP attendance was associated with less of a change in positive attitude (r=–.34, p=.002); in the SHA-CMHA sample, no correlations were found between these variables. Correlations between OMES change scores and attendance indicated that increased SHA attendance was related to increases in organizational empowerment (r=.29, p<.001); no such correlations were found for the BSR-COSP sample.
Table 3 presents results for the endogenous variable relationships in the path models. All model regressions in both trials were significant (p<.001). In the SHA-CMHA trial, SHA participation had a direct positive effect on attitude change (b=1.20, p=.016) and the positive effect was mediated by a change in OMES scores (b=.27, p=.003) (
Figure 1). Positive change in OMES scores was associated with SHA participation in the SHA-CMHA sample (b=.84, p<.001), after the analysis controlled for all exogenous covariates. In the SHA-CMHA trial, SHA participation and the ATPMIS positive change scores had direct effects on positive change in the SES (b=.16, p=.009; b=3.91, p<.001, respectively). OMES change had no direct effect on SES; its relationship (positive effect on SES) was fully mediated by ATPMIS positive change (
Figure 1).
In the BSR-COSP–CMHA trial, BSR-COSP participation had a direct negative effect on attitude change (b=−4.73, p=.031); this effect was not mediated by a change in OMES scores (
Table 3;
Figure 1). The negative change in ATPMIS scores fully mediated the relationship between BSR-COSP participation and change in SES scores (b=.23, p<.004)—that is, less change in positive attitude was associated with less change in positive SES scores, the result of which appeared to be a modest average decline in SES scores.
The effect size (η
p2) for SHA participation was a minimum of 10% of the variance. The effect size (η
p2) of BSR-COSP participation was a minimum of 13% of the variance. These effect sizes can be characterized as medium (6%−13.8%) to large (>13.8%) (
27,
28).
Discussion
To promote better community care, mental health professionals should understand not only that social acceptance of people with mental illness may be critical to the effectiveness of peer support efforts but also how such acceptance may influence recovery. Because mutual support holds incredible promise, it is important to further examine the attitudes that people with mental illness have toward one another. This study offers some insight into how participation in different types of consumer-operated programs may influence attitudes and how attitudes contribute to recovery success.
In a previous study, SHA-CMHA trial participants showed significant improvement in recovery outcomes over eight months (
10). Compared with receipt of CMHA services only, SHA participation combined with CMHA services was associated with significant gains in personal empowerment, self-efficacy, and independent social functioning and with reductions in hopelessness and symptoms (
10). However, BSR-COSP–CMHA trial participants showed significant decrements in personal empowerment, self-efficacy, and independent social functioning over the same period, compared with those who received CMHA services only (
11). Across trials, no outcome differences were observed for the CMHA-only groups. The differential recovery outcomes were attributed to differences in organizational environments of the SHAs and the BSR-COSP (
11). As noted above, the empowering role in decision making given to SHA members is in sharp contrast to the limited decision-making opportunities afforded BSR-COSP members.
As shown in the analysis presented here, both trial samples had highly positive attitudes toward people with mental illness at baseline. Consistent with current findings (
29), these attitudes indicated that individuals in both samples were more willing than individuals in the 1978 general population and in a 1978 sample of people with mental illness to accept people with mental illness in close relationships and allow them more responsibility in these relationships (
30). In the respective trials, participation in combined treatment changed participants’ attitudes in opposite directions—consistent with the positive and negative outcomes observed in the trials. SHA-CMHA participants developed more positive attitudes than their CMHA-only counterparts, and BSR-COSP–CMHA participants became less accepting than those in the CMHA-only group. In a manner consistent with Cooley’s (
12) “looking-glass self” hypothesis, it appears that SHA-CMHA participants, who were afforded responsible roles in their organization (whose organizational empowerment was increased) developed more positive attitudes toward persons with mental illness and expressed greater willingness to afford responsibility to and interact with other people with similar conditions. However, BSR-COSP–CMHA participants, for whom decision-making responsibilities were not encouraged, may have come to see themselves and other participants as less responsible, less deserving of responsibility, and requiring more cautious association.
Because the association of positive attitude change was not entirely mediated by organizational empowerment—that is, a significant direct effect of participation in the consumer-operated program was also found—perhaps the more positive outcomes of the SHA-CMHA group enabled these individuals to see themselves as more responsible, whereas the more negative outcomes of the BSR-COSP–CMHA group produced more guarded views. These observations are somewhat validated by the direct effects observed between attitude change and the recovery indicator self-efficacy in both trials.
This study extends the results of two previous trials. Like all randomized controlled trials, it is limited in generalizability to the study context, its sample, and the time at which the data were gathered, and it needs replication. Statistical analyses are subject to the assumptions associated with use of these techniques (
31). Limitations unique to each trial are reported elsewhere (
10,
11). The BSR-COSP results are attributable to a single organization, and whether other BSR-COSPs are characterized by the same high degree of staff control is an empirical question yet to be addressed.
Despite these limitations, the findings are consistent with the consumer-survivor literature in regard to the importance of organizational empowerment and participatory democracy in programs’ success. The findings mirror the types of positive and negative behavioral consequences seen in other empowering and disempowering mental health organizations (32).
Conclusions
In a review of the stigma literature, Rüsch and colleagues (
15) noted, “There are a number of factors that create an advantageous environment for interpersonal contact and stigma reduction. This includes equal status among participants, a cooperative interaction as well as institutional support.” This characterization clearly distinguished the SHA from the BSR-COSP settings. Future research should go beyond the simple notion that bringing consumers together to help themselves is always a good thing. One needs to consider the nature of the self-help experience and how that experience affects attitudes to self and others and other recovery outcomes.
Acknowledgments and disclosures
This study was supported by research grant RO1-MH37310 from the National Institute of Mental Health and by the Mack Center on Mental Health and Social Conflict.
The authors report no competing interests.