Illness self-management has emerged as a promising strategy for addressing chronic health conditions among persons with serious mental illness. Life expectancy for persons with a severe mental illness ranges from eight (
1) to 32 years (
2) shorter than for the general population. The combined impact of serious mental illness and comorbid general medical conditions contributes to significant functional impairment and disability. Self-management of both general medical and mental disorders appears to hold the greatest promise for achieving improved outcomes. However, existing self-management interventions have addressed either general medical illness or psychiatric illness, but not both (
3,
4).
Randomized trials have evaluated interventions for self-management of general medical illness by persons with serious mental illness, including the Health and Recovery Peer Program (
5) and Living Well (
6). Both interventions are adapted from the Chronic Disease Self-Management Program (
7) and consist of weekly group sessions taught by lay peers with chronic general medical conditions. The Health and Recovery Peer Program was associated with improved patient activation in perceived ability to manage health conditions and health behaviors and with more primary care visits (
5). Living Well has been shown to improve self-efficacy, behavioral activation, and self-management as well as general health functioning (
6).
Whereas data on illness self-management for medical conditions among persons with serious mental illness are limited, over 40 randomized controlled trials demonstrate the effectiveness of psychiatric illness self-management consisting of psychoeducation, behavioral tailoring, training in relapse prevention, and cognitive-behavioral techniques (
8). Illness Management and Recovery (IMR) was developed by bringing these practices together in a ten-module curriculum delivered to individuals or in groups (
9). IMR has been shown to be effective in three randomized trials (
10–
12) and is associated with greater knowledge of psychiatric illness (
10), fewer hospitalizations (
13), and reduced suicidal ideation (
14) as well as with improved psychiatric symptoms, psychosocial functioning, and quality of life (
11). The Substance Abuse and Mental Health Services Administration recognizes IMR as an evidence-based practice and provides a standardized version in a tool kit to facilitate widespread implementation (
15).
The purpose of this study was to evaluate the feasibility and effectiveness of integrated IMR (I-IMR), an intervention that extends IMR for psychiatric conditions to the self-management of chronic general medical conditions. Integrated self-management training for psychiatric and general medical illnesses is complemented by nurse health care management (
16) and builds on the demonstrated success of IMR in usual mental health service settings. We conducted a randomized controlled pilot trial comparing I-IMR to usual care among middle-aged and older adults with serious mental illness and a comorbid general medical condition. We addressed the following hypotheses: I-IMR will be feasible for use by older adults with serious mental illness and will be associated with improvement in self-management of both psychiatric and general medical illness, greater participation in psychiatric and primary health care encounters, and lower acute care service use.
Methods
A randomized controlled trial compared outcomes among participants in the eight-month I-IMR program and participants in usual care at two and six months postintervention (ten- and 14-month follow-ups). The study took place from November 2006 to March 2009 at two community mental health centers in New Hampshire, one in Manchester and one in Nashua. Participants were recruited through self-referral and clinician referrals and were paid for completing assessments but not for attending I-IMR sessions. Informed consent was obtained through procedures approved by the Committee for the Protection of Human Subjects at Dartmouth College and the New Hampshire Bureau of Behavioral Health.
Participants
Eligible individuals met the following inclusion criteria: age ≥50; enrollment in treatment at a community mental health center for at least three months; diagnosis of a primary
DSM-IV axis I disorder confirmed by the Structured Clinical Interview for DSM-IV (
17), including schizophrenia spectrum, bipolar disorder, or major depression associated with pervasive impairment lasting at least one year across multiple areas of psychosocial functioning; diagnosis by a physician of diabetes, chronic obstructive pulmonary disease (COPD), congestive heart failure, ischemic heart disease, hypertension, hyperlipidemia, or osteoarthritis; stable treatment with psychopharmacological medication for a minimum of eight weeks; and receipt of voluntary informed consent for participation. Exclusion criteria included no prior participation in the IMR program, residence at a nursing home or psychiatric hospital, diagnosis of dementia, terminal illness with life expectancy of one year or less, or a score below 24 on the Mini Mental State Examination, indicating moderate to severe cognitive impairment (
18).
Interventions
Integrated IMR.
The I-IMR program integrates components of conventional IMR related to psychiatric illness self-management with strategies for self-management of general medical illness. [A list of I-IMR modules is available online as a
data supplement to this article.] The psychiatric component includes psychoeducation about illness and treatment, cognitive-behavioral approaches to increase medication adherence, training in relapse prevention, instruction about coping skills to manage persistent symptoms, and social skills training (
9). The general medical illness component consists of an individually tailored curriculum that applies the same skills and strategies for self-management of psychiatric illness to the self-management of general medical illness. In addition, a nurse health care manager facilitates coordination of necessary preventive and ongoing health care. The I-IMR curriculum consists of ten modules that are delivered over a period of eight months during weekly sessions led by an I-IMR specialist. The sessions are customized to the specific needs and disorders of each client.
The I-IMR specialist had a master’s degree in social work and received 1.5 days of training in administering I-IMR. The training was based on the standardized program tool kit and program manual. Throughout the study, the I-IMR specialist received supervision during a weekly call with one of the authors (SIP), a clinical psychologist with expertise in behavior change, motivational interviewing, and illness self-management. The I-IMR specialist provided training and support to participants in identifying and achieving personal recovery and wellness goals, breaking down goals into manageable steps, and working on achieving these goals. The specialist used a combination of psychoeducational, motivational, and cognitive-behavioral teaching strategies, including role-playing and homework assignments. Skills training was tailored to each participant’s psychiatric and general medical condition and consisted of modules and materials for goal setting and self-management.
A primary care nurse was embedded one day per week at each mental health center to coordinate health care appointments, medication adjustments, and transfer of information and to provide counseling on self-management and lifestyle changes for chronic health conditions. Participants met with the nurse health care manager twice per month to discuss progress and obstacles in meeting general medical and mental health goals. A full description of the I-IMR program is available elsewhere (
16).
Usual care.
Participants in both groups continued to receive the same services that they had been receiving prior to the study. Usual care at each site included pharmacotherapy, case management or outreach by nonnurse clinicians, individual therapy, and access to psychosocial support and rehabilitation services.
Measures
Feasibility was measured by participant attendance. Throughout the eight-month program, there were approximately 30 weekly sessions with the I-IMR specialist and 15 biweekly sessions with the nurse. The minimum attendance required to benefit from skills training and nurse management was defined as ten sessions with the I-IMR specialist and five sessions with the nurse.
Psychiatric illness self-management skills, including medication adherence, a relapse prevention plan, and knowledge of symptoms and coping strategies, were measured by using the client-rated and clinician-rated Illness Management and Recovery Scales (
19), each with 15 items rated on a 5-point scale, with higher scores indicating better self-management skills. Both scales have good internal and test-retest reliability for persons with serious mental illness (
20) and are correlated with independent assessments of community functioning (
21).
Self-management of general medical illness was measured by using the Stanford Chronic Disease Self-Efficacy Scale (SCDSES) (
22), comprising five items rated on a scale of 1, not at all confident, to 10, totally confident. The score is an average of all five items, with higher scores indicating greater self-efficacy. Disease-specific measures of self-management for diabetes, COPD, hypertension, hyperlipidemia, and arthritis were adapted from the SCDSES for this study (
22). Symptoms and functioning were evaluated by using the Brief Psychiatric Rating Scale (BPRS) (
23). The Multnomah Community Ability Scale (MCAS) (
24) was used to assess community functioning. This 17-item scale covers four subcategories related to interference with functioning, adjustment to living, social competence, and behavioral problems (
25). Items are rated from 1, impaired, to 5, normal.
Participation in psychiatric and general medical encounters was measured by using the communication role subscale of the Stanford Physician Communication Scale (
22). Possible scores range from 0 to 5, with higher scores indicating a more active role in communicating questions and needs.
Participation in psychiatric and general medical encounters was also evaluated by using the information-seeking preference and decision-making preference subscales of the Autonomy Preference Index (
26). These subscales measure the desire for information or involvement in decision making, with 0 indicating no desire, 50, neutral desire, and 100, strong desire.
Use of acute care services was measured by using self-reports of hospitalizations and emergency visits for psychiatric or general medical disorders over the prior three months. A three-month recall period has demonstrated greater accuracy than longer recall periods for predicting health service utilization (
27). All measures were completed during independent, blinded assessments by trained research interviewers at baseline and at 10- and 14-month follow-ups.
Statistical analyses
Two-tailed t tests and chi square analyses were used to compare study groups by demographic characteristics, psychiatric history, and outcome measures at baseline. Means and standard deviations were calculated for number of I-IMR specialist and nurse sessions attended by each group. For analysis of treatment effects, total scores or subscale scores for each outcome measure were the dependent measure. Treatment effects were evaluated by using intent-to-treat analyses for the full sample of randomly assigned participants. Because there were no significant differences between I-IMR and usual care groups at baseline and there were only two follow-up assessments, rather than fitting parametric curves with random effects, we included the baseline as a covariate and controlled for diagnosis, gender, and interaction of diagnosis and gender. Baseline-adjusted mean response profile models (
28), also referred to as covariance pattern models, were calculated for the following dependent variables: psychiatric and general medical illness self-management skills, mental health symptom severity, community functioning, and shared decision making with both psychiatric and primary care clinicians. This approach falls within the general mixed-effects model framework (
28,
29), but it is more appropriate for repeated-measures data with few assessment points. Within-subjects correlations were managed by selecting appropriate covariance structures, and missing data were accommodated with maximum likelihood estimation.
Because the outcomes were statistically adjusted for baseline levels, treatment effects were evaluated by group main effects (differences in group means). Two-tailed statistical tests were conducted, and differences with a p value of ≤.05 were considered statistically significant. Estimates of effect size were calculated on the basis of analyses of covariance, adjusting the correlation between baseline and 14-month follow-up, because this approach has more power for randomized controlled trials (
30). Between-group effect sizes at endpoint were computed with Cohen’s d by using the thresholds defined by Cohen (
31) for small (.20), moderate (.50), and large (.80) effect sizes. A generalized linear model approach was used to compare hospitalizations and emergency visits between I-IMR and usual care groups over time. All statistical analyses were performed with SPSS, release 19.0.
Results
Participants assigned to I-IMR (N=36) and those assigned to usual care (N=35) did not differ significantly on baseline demographic or diagnostic measures (
Table 1). Of the 71 participants, 56 (79%) completed the postintervention assessment at the ten-month follow-up, and 54 (76%) completed the postintervention assessment at the 14-month follow-up. Rates of follow-up were lower among participants assigned to I-IMR than among participants assigned to usual care (N=25 [69%] and N=31 [89%], respectively, at ten months and N=24 [67%] and N=30 [86%], respectively, at 14 months), although these differences were not significant. Overall, I-IMR participants attended 15.8±9.5 sessions with the I-IMR specialist and 8.2±5.9 sessions with the nurse. A majority of I-IMR participants (N=27, 75%) attended ten or more sessions with the I-IMR specialist and five or more sessions with the nurse. That group attended 20.1±5.8 sessions with the I-IMR specialist and 10.6±4.6 sessions with the nurse. At baseline, these participants and those who attended fewer sessions differed only on the BPRS retardation subscale (p=.005).
Self-management
Self-management outcomes at baseline and ten- and 14-month follow-ups are shown in
Table 2. I-IMR was associated with greater overall improvement in both client-rated and clinician-rated psychiatric illness self-management skills. Among I-IMR participants, there was greater improvement in self-management of diabetes, and nonsignificant trends emerged indicating greater improvement in self-management of general medical illnesses and COPD. No differences were found for improvement in self-management of hypertension, hyperlipidemia, and osteoarthritis. There were also no differences between groups for improvement in psychiatric symptom severity and community functioning.
Physician encounters
Compared with usual care, I-IMR was associated with a greater preference for receiving detailed diagnosis and treatment information during primary care encounters (
Table 2). I-IMR was also associated with nonsignificant trends for a greater preference for receiving detailed diagnosis and treatment information and less preference for decision-making autonomy during psychiatric encounters as well as a more active role in communicating questions and needs with primary care physicians.
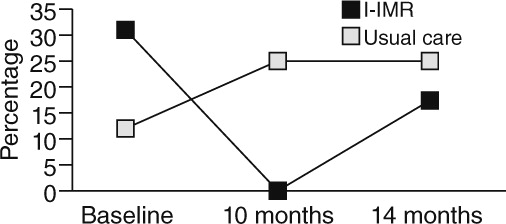
Health service utilization
Despite randomization, at baseline the proportion of participants who reported at least one psychiatric or general medical hospitalization during the prior three months was over twice as high among I-IMR participants (31%; N=11) than among usual care participants (17%; N=4), although this difference was not significant. At ten-month follow-up, none of the I-IMR participants had experienced a hospitalization during the prior three months, compared with one-quarter (N=7) of usual care participants. At 14-month follow-up, 17% (N=4) of I-IMR participants had been hospitalized during the prior three months, compared with 25% (N=7) of participants assigned to usual care (
Figure 1). The proportion of participants self-reporting psychiatric or medical hospitalizations decreased among I-IMR participants compared with usual care participants (χ
2=4.36, df=1, p=.037). There were no between-group differences over time for self-reported emergency visits.
Discussion
Consistent with our open pilot study of the I-IMR program (
16), a majority (75%) of participants attended at least ten I-IMR sessions and five nurse sessions over the eight-month intervention, supporting the feasibility of I-IMR for persons with serious mental illness and chronic general medical conditions. Compared with usual care, I-IMR contributed to improvements in self-management of psychiatric illness and diabetes, greater participation in primary health care encounters, and fewer psychiatric or general medical hospitalizations. To our knowledge, this is the first study demonstrating the feasibility and potential effectiveness of simultaneous delivery of training in psychiatric and general medical illness self-management with nurse support for persons with serious mental illness and chronic general medical conditions.
I-IMR was associated with greater psychiatric illness self-management, consistent with prior randomized trials of IMR (
10–
12,
32,
33). Our finding of improved self-management for diabetes but not for other general medical conditions is consistent with studies of older adults without mental illness. Programs aimed at improving diabetes self-management activities, for example, diet, self-monitoring, and medication management, showed robust effect sizes, whereas self-management of chronic conditions with less immediate benefits, such as osteoarthritis, had a more modest impact (
34). Together, these findings suggest that I-IMR is potentially effective in improving self-management abilities for both psychiatric and general medical illness, contributing to overall functioning. The per-person cost for the 36 participants in the eight-month I-IMR program was $1,509 in 2012-adjusted dollars, which reflects the salaries of a full time I-IMR specialist and the equivalent of one half-time nurse. Given that I-IMR is designed to reach persons at high risk of incurring significant treatments costs, these costs were considered modest.
Previously we reported that adults with serious mental illness prefer to take an active role when interacting with their psychiatrist and a passive role when interacting with their primary care physician (
35). This study found that I-IMR was associated with a trend for preferring more information during psychiatric encounters and a significantly greater preference for obtaining more information during medical encounters. This preference for greater information is consistent with I-IMR’s emphasis on encouraging health care consumers to become more knowledgeable and informed. In contrast, although not statistically significant, I-IMR was associated with developing a preference for a slightly greater role for physicians in decision making during psychiatric and medical encounters. Hence, although I-IMR may contribute to a greater preference for more information, it may simultaneously result in a greater preference for involving the physician in making decisions in complex situations.
The decrease in hospitalizations among I-IMR participants is consistent with a prior trial of IMR (
13) and with findings from evaluations of other chronic illness self-management programs (
7). However, given that I-IMR includes self-management training and nurse care management, it is not possible to identify the relative contributions of each component to reduced psychiatric or general medical hospitalizations. Caution is also warranted when interpreting these findings because the proportion of participants who reported at least one hospitalization in the three months prior to baseline was greater among participants who received I-IMR than among participants who received usual care. However, it is most likely that this difference further supports (rather than detracts from) our findings of fewer hospitalizations at follow-up associated with I-IMR, given that prior hospitalizations are a strong predictor of and risk factor for subsequent hospitalizations in comparable patient groups (
36).
Another limitation was the small sample size of our pilot study, potentially increasing the risk of type II error—concluding prematurely that I-IMR was ineffective in improving outcomes for which it may have beneficial effects—and of inability to reliably determine whether the effects of I-IMR were sustained over time. The small sample size was also a likely contributor to baseline differences in the proportion of participants in each group with schizophrenia spectrum disorders or bipolar disorder, although these differences were not statistically significant. We do not expect that any differences in these diagnostic distributions were of clinical importance because a prior study by our group comparing skills training and usual care among older adults (≥50 years old) with serious mental illness found no differences by diagnosis with respect to self-efficacy and functional outcomes (
37,
38).
In addition, given that this investigation was a pilot study aimed at assessing the feasibility and potential effectiveness of I-IMR, we did not evaluate physical and laboratory measures of disease outcomes. Finally, participants were predominantly Caucasian. Hence we were unable to determine the feasibility and potential effectiveness of I-IMR in ethnically diverse populations, although prior studies of IMR have demonstrated robust results in more representative samples (
11).
Conclusions
Our results demonstrated that providing integrated training and support for self-management of psychiatric and general medical illness is feasible and potentially effective. Furthermore, I-IMR has the advantage of directly building on the original IMR program, which has been associated with successful widespread dissemination and training in usual mental health delivery settings across the nation (
10). This record of success potentially provides a ready context for implementation among agencies where clinicians are already trained to deliver IMR. In addition, uninitiated providers have the opportunity to adopt an illness self-management intervention that accommodates the challenge of a growing number of patients with comorbid general medical and psychiatric illness (
39). Training and supporting adults with serious mental illness in self-management of psychiatric and general medical disorders complement growing efforts to establish patient-centered medical homes for persons with serious mental illness in the context of current and future accountable care organizations (
40). Providing integrated illness self-management training embraces the interrelationship of recovery and wellness, while directly recognizing that general medical and mental health are inextricably essential in supporting optimal functioning and quality of life for the “whole person” (
41).
Acknowledgments and disclosures
Grant support was provided to Mr. Riera from the National Institute of Mental Health and the Substance Abuse and Mental Health Services Administration (R34 MH074786). The authors thank Margaret Almeida, R.N., M.B.A., Sarah Bishop-Horton, Ed.M., Elena Bogdan, R.N., Patricia Bolter, M.S., Patricia Carty, M.S., Edward G. George, M.B.A., Mark Guillemette, M.S., M.Div., Peter Jannelle, M.B.A., Ed Mahoney, D.Min., M.Th., Chip Maltais, B.S., Kris McCracken, M.B.A., Erica O’Neal, M.D., and Nancy Sharkey, R.N.
The authors report no competing interests.